There are no clinical recommendations in oncology for duodenal cancer, but they have been awarded to its anatomically tiny structural part - the duodenal major or papilla of Vater, into which the duct common to bile and pancreatic enzymes opens.
Traditionally, all serious duodenal diseases are automatically considered together with pathologies of the stomach, although the duodenum is the initial part of the intestine, and the duodenum is united with the stomach only by anatomical proximity.
- Anatomy of the duodenum
- Causes of duodenal cancer
- Diagnosis of duodenal cancer
- Stages of duodenal cancer
- Prognosis for duodenal adenocarcinoma
- How does duodenal cancer manifest?
- Treatment of duodenal cancer
Fundamentals of pathophysiology
Duodenal cancer is characterized by severe symptoms.
Approximately 65% of all small intestinal neoplasms are malignant, and approximately 45% of these tumors are adenocarcinomas.
Small adenocarcinomas of the duodenum have striking similarities to adenocarcinomas of the colon.
These similarities are mainly epidemiological - tumors have similar geographic distributions and common risk factors.
In addition, as in the case of adenocarcinomas of the colon, tumors of the duodenum develop from precancerous forms of adenomas. Malignancy of precancerous forms occurs sporadically in the context of a family history.
The reason is often associated with the accumulation of genetic mutations from generation to generation. Only an established malignant tumor of the duodenum quickly spreads metastases to distant areas of the body through the lymphatic and circulatory systems.
Despite the similarities between tumors of different parts of the intestine, adenocarcinomas of the small intestine tend to spread along the tract towards the stomach. Approximately 55% of small intestinal tumors develop in the duodenum, 25% in the jejunum, and 20% in the ileum.
The duodenum is the initial part of the small intestine, so it is exposed to harsh environments and chemicals in food. In addition, studies have shown that sometimes bile secreted into the duodenum can be carcinogenic.
Genetic analysis of sudden duodenal adenocarcinomas has revealed similarities and differences in the pathogenesis of colorectal carcinomas. Often these tumor processes share common genetic causes.
Small bowel tumors
Primary duodenal tumors can be either benign or malignant. Most of these tumors are asymptomatic. Tumors usually present clinically as malignant tumors. These include adenocarcinoma, lymphoma, leiomyosarcoma, neurofibrosarcoma, rhabdomyosarcoma, melanosarcoma, plasmacytoma and carcinoid. Most of these tumors occur in patients aged 50 to 70 years. The clinical picture is dominated by bleeding, abdominal pain, weight loss, fever and intestinal obstruction (intermittent or constant).
According to most statistics, the most common malignant tumor of the small intestine is adenocarcinoma. Adenocarcinomas are usually found either in the duodenum, or at the ampulla of the major duodenal papilla, or in the proximal jejunum. Primary adenocarcinoma of the duodenum constitutes (according to operational and sectional data) 0.033% of all tumors of the gastrointestinal tract (Taenzer WP et al, 1972). The tumor grows exophytically or in the form of an ulcer, or has an infiltrating growth pattern. Duodenal cancers are characterized by a rapid course and early spread into neighboring organs - the pancreas, retroperitoneum, hepatoduodenal ligament, and also early metastasize to regional lymph nodes.
Primary adenocarcinoma of the duodenum must be differentiated from secondary carcinoma arising from the major duodenal papilla, pancreas, biliary tract, or right kidney.
Malignant lymphoma of the duodenal bulb
In rare cases, metastases of other tumors are found in the duodenum.
In 12% of patients, Zollinger-Ellison syndrome is caused by a tumor of the ectopic pancreas, localized in the duodenum or in the antrum of the stomach (Ellison LH et al. 1964).
Tumors of different histological nature occur in the small intestine. From 30 to
Lymphomas account for 50% of all small intestinal tumors. Primary intestinal lymphomas (non-Hodgkin's) appear as a local formation (Western run) or diffuse infiltration (Mediterranean type). The incidence of lymphomas is increased
in patients with gluten enteropathy (celiac disease), Crohn's disease of the small intestine, AIDS, after organ transplantation, and with autoimmune diseases. Clinically
Lymphomas present with malabsorption, diarrhea, weight loss, pain, perforation and bleeding.
Endoscopic semiotics. Multiple irregularly shaped ulcers are visible on all
walls of the duodenal bulb. The edges of the ulcers are fuzzy, their bottom is uneven, lumpy, covered with a dirty gray fibrinous coating.
Among tumors of the small intestine, carcinoids occupy a special place, manifesting
both benign and malignant tumors. Carcinoids range from 4 to
23% of tumors of the small intestine (Krasnokutsky Yu.A.. 1996). Among all localizations of carcinoid tumors, the small intestine accounts for 22-25% (Crocetti E. et al., 1997). It is noted that the ileum is most often affected, while carcinoid tumors of the duodenum account for no more than 8% of carcinoid tumors of the gastrointestinal tract. Tumors are localized in all parts of the duodenum and even in the area of the major duodenal papilla (Derizhanova I.S. 1991; Laura V. et al. 1997).
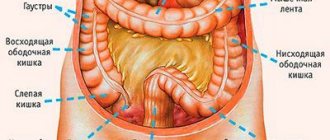
In the racemic colon, carcinoids are found, as a rule, in people over 40 years of age, mainly in men. According to T.P. Makarenko and M.I. Brusilovsky (1966), carcinoids of the small intestine should be considered from the very beginning as malignant neoplasms.
Clinical manifestations of tumors of this localization are extremely scarce. Only some patients have signs of intestinal dyspepsia (abdominal pain without specific localization, flatulence, unstable stool). As a rule, with tumors up to 1 cm in diameter, the process is generally asymptomatic. More pronounced clinical manifestations are observed with tumors more than 1.5 cm in diameter. The disease can occur in the form of chronic intestinal obstruction, when the patient is bothered by paroxysmal pain, constipation, and periodic bloating for several years. Sometimes the clinical picture resembles that of an acute infectious intestinal disease, when the patient experiences debilitating diarrhea (up to 30 times a day), and in later stages, a carcinoid tumor can manifest as obstructive intestinal obstruction, recurrent intestinal bleeding, perforation and peritonitis.
An extremely rare complication is intussusception of the terminal ileum.
intestines into the cecum (Marcids S. et al., 1990).
Carcinoids are a small tumor that is located in the submucosal layer of the intestinal wall, although it does not have a capsule. The tumor is most often localized on the antimesenteric side of the intestine. During the growth process, the tumor first infiltrates the muscular and then the serous layers. It should be noted that carcinoids cause a fibrotic reaction in surrounding tissues and organs, which often leads to significant adhesions, kinks and torsions of intestinal loops, causing intestinal obstruction in some cases. The histological structure of carcinoid resembles alveolar cancer.
The tumor can be solitary or multiple. J. Hoferiduer and R. H. Stanhlgrcn (1963)
Dual localization of the tumor was observed. Askanazy in one case encountered 32 tumor nodes in the small intestine. M.V. Dockcrty and KS.Ashbu.rn (1943) - 68, and P.Z. Kotlyarchuk (1927) - over 100 tumors. An observation by RJ Sanders and HR AxLell (1964) was published, in which 209 small tumor nodes were noted in the small intestine. According to RXSanders and H.RAxleU, multiple small bowel carcinoids are observed in 29% of cases.
Carcinoids of the small intestine in 50-70% of cases metastasize mainly to the mesenteric lymph nodes and liver, less often to the lungs, bones, ovaries and brain.
Analyzing 209 cases of colonic carcinoids, CGMoerlel et al. (1961) came to the conclusion that the frequency of metastasis is proportional to the size of the tumor.
For tumors less than 1 cm in diameter, metastases to the lymph nodes occur in 2%
cases, with carcinoids with a diameter of 1-2 cm, metastases are found in 30% of patients,
and for larger tumors - in 88% of cases. Ileal carcinoids metastasize most often (65-75%). These metastases differ from the primary tumor in their larger size and increased secretion of serotonin. Even with non-radical surgical treatment, cases of spontaneous regression of metastases have been described.
There is an opinion that the manifestation of carcinoid syndrome is most often associated with the presence of multiple metastases. This syndrome is observed in 25% of patients with metastases and is caused mainly by two reasons: overproduction of serotonin and the loss of the liver’s ability to inactivate it. In carcinoid syndrome there are three leading symptoms: 1. chronic enteropathy; 2. paroxysmal circulatory disorders with redness of the skin of the face, neck, upper half of the body; 3. damage to the valvular apparatus of the heart. One of the manifestations of carcinoid syndrome should be considered the formation of peptic ulcers in the stomach and duodenum, which, according to RAMacDonald (1956), is observed in 38% of cases.
Carcinoid tumors of the duodenum are very rare. They
range from 1.3 to 2.8% of all carcinoid tumors of the gastrointestinal tract. Many authors emphasize the frequent association between carcinoid tumors of the duodenum and gastric or duodenal ulcers.
Carcinoids are found throughout the small intestine, but their favorite localization is the terminal ileum and appendiceal process.
A rare location of carcinoid is the duodenum. In the clinical course of the process with duodenal carcinoids, three main ones are distinguished:
forms: stenotic, icteric and hemorrhagic. When the tumor is localized in the area of the major duodenal papilla, jaundice develops, and when ulceration occurs, bleeding occurs.
According to various authors, five-year survival rate for small intestinal carcinoids
without metastatic lesions is approximately 95%, with metastases
to regional lymph nodes - 62-83%, in the presence of distant metastases - 38% (GPThomson et al, 1985).
Leiomyosarcomas in the small intestine are less common and are usually large when diagnosed. Sometimes melanoma is found in the rectum.
Among benign tumors of the small intestine, adenomas (usually duodenal), leiomyomas (intramural) and lipomas (ileal) predominate. Some authors consider leiomyoma to be the most common benign tumor of the small intestine (Hancock RJ, 1970), others consider adenoma (Ratisr Yu.A.. 1962: Pcrzin K.N. et al., 1984). A later publication reported that of 196 benign tumors of the small intestine, 51 were adenomas, 43 were leiomyomas, 35 were lipomas, 22 were Brunner's gland adenomas, 21 were lymphangiomas, 14 were vascular tumors, and 10 were fibroids. Very rarely, fibroids and neuromas are found in the racemic colon.
Apparently, adenomas are the most common tumors of the duodenum, especially the large duodenal papilla, and then their frequency gradually decreases in the jejunum and ileum.
Adenomas most often occur in elderly patients, the peak occurs in the seventh decade. Gender doesn't matter. The clinical picture depends on the location and type of lesion. Often the clinical picture of the disease cannot be analyzed due to the layering of symptoms of the underlying disease (malignant and benign tumors of the stomach, lungs, uterus). Sometimes exophytically growing tumors reach large sizes and can be palpated by the patients themselves. Tumors are often large and disintegrating, so peritonitis is a possible complication.
With small tumors, intestinal obstruction may develop due to intussusception.
Small intestinal adenomas can be divided into two subtypes: tubular and villous adenomas. Tubular adenoma in the duodenum is usually asymptomatic, although with large lesions, patients may experience pain and bleeding.
The X-ray picture is nonspecific.
Endoscopic semiotics. The tumor may be broad-based or pedunculated
its surface is smooth or lobed. The tumor size is from 0.5 to 3 cm in diameter. The tumor is usually single, but multiple adenomas have also been described. Large adenomas can ulcerate and obstruct the intestinal lumen.
The clinical picture of villous adenoma is characterized by pain in the epigastric region, gastrointestinal bleeding, intestinal obstruction, jaundice and pancreatitis. In some patients, symptoms may be vague and nonspecific.
Endoscopic semiotics. A lumpy tumor is identified, usually solitary.
The size of the tumor is from 5 to 8 cm in diameter. A villous tumor becomes malignant more often than a tubular adenoma.
Malignant tumors often coexist with benign adenomas.
Timely diagnosis of small intestinal tumors does not exceed 13%. More than 60% of patients undergo emergency surgery for tumor complications. Diagnosis of tumors of the small intestine is based on radiography of the small intestine and X-ray examination with barium sulfate. Angiography is necessary to characterize the vessels in the tumor, CT allows one to assess the size of the formation (especially lymphomas), ultrasonography and scintigraphy - to determine metastatic lesions of other organs.
Duodenoscopy plays a leading role in the diagnosis of duodenal tumors.
with biopsy.
From an endoscopic point of view, the small intestine is the most difficult organ of the gastrointestinal tract to access. Due to the considerable length of the small intestine, many parts of it are extremely difficult to examine. In 2002, the Japanese created
electronic enteroscopic double-balloon system. New exclusive technique
insertion of the endoscope using two air balloons ensures precise placement and safe fixation of the external tube in the small intestine. After this, the end of the endoscope can be easily brought to the area of interest. A specially designed air injection system will allow you to constantly maintain a stable level of pressure in the air cylinders, as well as increase and decrease this pressure to the desired level, which ensures safe and successful insertion of the epteroscope.
Indications for epteroscopy are intestinal bleeding of unknown etiology and small intestinal obstruction (when pathology from the
esophagus, stomach, duodenum and colon), Crohn's disease, chronic
diarrhea and abdominal pain. This is the preferred method for recognizing tumors in the small intestine, which allows us to identify the nature of the pathology and verify the diagnosis
using a morphological study of biopsy material, since the device allows for biopsy.
The lack of verification of the diagnosis, as well as the inability to exclude acute surgical pathology, are indications for performing diagnostic laparotomy.
Tumors of the major duodenal papilla
Stenosis of the major duodenal papilla was first described in 1884 by Laugenbueh, who recommended dissecting the papilla to remove impacted stones and, if
its cicatricial constrictions. However, for a long time, stenosis of the major duodenal papilla
found only in isolated observations. Stenosis of the major duodenal papilla often causes obstruction of the bile ducts and pancreatic ducts.
According to various authors, the incidence of stenosis of the major duodenal papilla during surgery ranges from 15 to 30%. The causes of stenosis are varied. In some cases, stenosis of the major duodenal papilla is a consequence of inflammatory changes in the papilla in diseases of the duodenum as a result of duodenitis and pancreatitis. In other cases, obstruction of the large duodenal papilla and its narrowing are caused by benign papillary adenomas.
Benign tumors of the major duodenal papilla are usually observed in young and middle-aged people, equally often in men and women. In the area of the ampulla of the large duodenal papilla and in the periampullary zone, adenomas manifest themselves clinically much earlier than in the small intestine, even if they are small in size. Patients are concerned about remitting jaundice, pain in the right hypochondrium and in the epigastric region, and bleeding.
Endoscopic semiotics. The orifice of the large duodenal papilla gapes, admission
there is no bile from it. In the area of the mouth of the large duodenal papilla, a polypoid-shaped tumor, soft consistency, and bright red color is determined. The size of the tumor ranges from a few millimeters to 1-2 cm.
With intrapapillary villous adenoma, the major duodenal papilla may bulge somewhat into the lumen of the duodenum. Adenoma emerges from the papilla
in the form of a fringe. In other cases, villous adenoma bulges into the lumen of the duodenum in the form of a nut, sometimes almost completely filling the lumen of the parafaternal diverticulum. On instrumental palpation, the papilla is dense; when taking a biopsy, there is pronounced contact bleeding.
Histological examination of biopsy material reveals mature epithelial elements of a glandular structure with a well-developed connective tissue stroma. These tumors develop from the mucous membrane of the large duodenal papilla or pancreatic duct (Fig. 6.27 B). The frequent detection of tumor cells and elements of the inflammatory process in the tissues of the major duodenal papilla gives grounds for some authors to consider the inflammatory reaction as the cause of the development of the tumor process in the major duodenal papilla. Endoscopic retrograde cholangiopancreatography clearly indicates the level of obstruction.
Benign tumors of the major duodenal papilla are precancerous
conditions, as they are prone to malignancy. Many researchers pay attention to the development of cancer of the major duodenal papilla from adenomas. The risk of malignancy for an ampullary or periampullary adenoma is much higher than for an adenoma located in the duodenum or the rest of the small intestine. According to P. Gcrtsch et al. (1987), a histological examination of cancerous tumors of the major duodenal papilla revealed that they all contained tissue of adenomatous polyps with epithelial dysplasia.
Major duodenal papilla cancer
Cancerous tumors of the major duodenal papilla develop from the epithelium of the mucous membrane of the duodenum in the area of the papilla, the epithelium of the mucous membrane of its ampulla or the epithelium of the final sections of the common bile and pancreatic ducts. Despite these differences in histogenesis, from a practical point of view, all such neoplasms are usually united under the general concept of “cancer of the major duodenal papilla,” as proposed by Carnot in 1908.
The incidence of cancer of the major duodenal papilla is about 2% of tumors of the gastrointestinal tract (Natyutko Yu.I., 1998; Schenlke K.Li., 1986). The proportion of cancer of the major duodenal papilla among neoplasms of the hepatobiliary and pancreaticoduodenal zone ranges from 10.1 to 18.3% (Rusakov V.I. et al. 1986; Frosali P. et al., 1990).
Clinical classification of carcinoma of the major duodenal papilla according to the TNM system:
TX—the primary tumor is not determined
TO - no signs of primary tumor
Tis - carcinoma in situ
Ti - tumor is limited to the ampulla of Vater's papilla or sphincter of Oddi
T2 - tumor invades the wall of the duodenum
TZ - the tumor invades the pancreas
T4 - tumor invades peripancreatic tissue or other adjacent organs or structures
NX - regional lymph nodes are not detected
N0 - no metastases in regional lymph nodes
N1 - metastases in regional lymph nodes
MX - distant metastases are not detected
MO - no distant metastases
Ml - distant metastases
Cancer of the major duodenal papilla affects middle-aged and elderly people and is more common in men than in women.
Cancer of the major duodenal papilla (polypoid form)
Cancer of the major duodenal papilla has a number of characteristic clinical features, which makes it possible to suspect the presence of this disease. The most common signs of the disease are jaundice, pain in the upper abdomen, dyspeptic disorders and general disorders of the patient's condition. Jaundice without prodromal signs - “silent jaundice” (Nicdcrt V.. 1982) - is a consequence of obstruction of the bile ducts. This is the most constant symptom of cancer of the major duodenal papilla.
The pain in the upper abdomen is dull, constant, aching in nature. The cause of pain is cholangiostasis, as well as tumor growth into the pancreas or duodenum.
Often in the pre-icteric period of the disease, general weakness, fatigue, irritability, apathy, decreased appetite, weight loss, and anemia appear.
Macroscopically, a cancerous tumor of the major duodenal papilla occurs in the form of a polyp, ulcer or infiltrate.
Endoscopic semiotics of polyposis cancer. Tumor of the large duodenal
the papilla has the appearance of a mushroom-shaped formation or resembles a cauliflower. Tumor
protrudes into the lumen of the duodenum, reaches a size of 3-5 cm.
Endoscopic semiotics of ulcerative cancer. Major duodenal papilla cancer
looks like an irregularly shaped ulcer, ranging in size from 1 to 4 cm, with dense, undermined
edges and bleeding bottom, covered with purulent deposits.
Endoscopic semiotics of infiltrative cancer. In the area of the large duodenal papilla, a tumor is visible, infiltrating neighboring tissues and spreading to the duodenum.
The diagnosis of carcinoma of the major duodenal papilla is not difficult with polyp-like growing papillary adenocarcinoma or with an ulcerated tumor.
However, even in these cases, diagnostic difficulties may arise due to the large spread of the tumor to surrounding tissues. The condition of the longitudinal fold of the duodenum, namely its bulging, is important. This may be caused by a tumor of the terminal part of the common bile duct or strangulation of a stone in the papilla.
Detection of a malignant tumor is difficult during endoscopic examination
in cases where the primary carcinoma is located in the thickness of the large duodenal papilla. In this case, the examination data will be inconclusive, and a histological examination of the biopsy material is necessary to clarify the diagnosis. Large lesions with ulceration or obstruction usually show malignant changes on histological examination. A small biopsy fragment can be used to diagnose malignant changes if the cancerous focus is located in the biopsy fragment. According to DP Ryan et al. (1986), if cancer cells are found in five out of nine biopsy fragments, false negative results occur in 56% of cases. If cancer is not detected in several biopsy fragments, then partial excision of the tumor is performed. If an invasive focus is detected in the biopsy fragment, then the histological diagnosis of carcinoma is beyond doubt.
According to their histological structure, cancerous tumors of the major duodenal papilla, despite their different origins, most often represent adenocarcinomas. The tumor parenchyma usually consists of atypical cells of cylindrical or cuboidal epithelium, forming poly round, oblong or irregular shapes. In some cases, the tumor consists of polymorphic cellular elements, creating a picture of solid or mucinous cancer. Depending on the degree of development of the connective tissue stroma, the tumor may have the appearance of scirrus or, less commonly, simple and brain cancer.
N.N. Blokhin et al. (1982), W. C. Kimura et al. (1994) based on histological studies of tumors of the major duodenal papilla, intestinal and pancreatobiliary types of cancer of the major duodenal papilla are distinguished. The pancreatobiliary type of cancer is characterized by papillary growths with scanty fibrous cores. The spread of cancer of the major duodenal papilla occurs through the lymphatic gaps, interstitial spaces and connective tissue spaces surrounding the ducts, vessels and nerves. In this case, the tumor first grows into the submucosal and muscular layers of the papilla, and then can infiltrate the wall of the bile duct, pancreatic tissue and adjacent parts of the duodenum. According to N.N. Blokhin et al. (1982), cancer of the major duodenal papilla grows more slowly than tumors of other organs of the biliary system, rarely reaches large sizes and metastasizes in the later stages of its development. Therefore, the pathological process for a long time may not extend beyond the papilla itself. As a result, cancer of the major duodenal papilla has a more favorable clinical course, and early surgical treatment gives a lasting result.
Epidemiology of duodenal cancer
In Russia, several thousand cases of duodenal cancer are registered annually, and this form of cancer is less common among women. About a quarter of those infected eventually die.
The prognosis of the disease indicates a five-year survival rate of 30-35%. Unfortunately, this form of cancer spreads quickly throughout the gastrointestinal tract and metastasizes almost immediately after its occurrence.
Malignant tumors of neuroendocrine origin, apudoms
Neuroendocrine tumors (NT) account for no more than 5% of all malignant neoplasms of the duodenum.
The following malignant neuroendocrine tumors are found in the duodenum:
- Gastrinoma - Zollinger-Ellison syndrome (pancreatic adenoma - a tumor of the islet apparatus of the pancreas, characterized by increased secretion of gastrin, which activates the secretion of large amounts of hydrochloric acid by the stomach);
- Insulinoma is a benign (less often malignant) neoplasm (usually from the beta cells of the pancreatic islets), which uncontrollably secretes insulin into the bloodstream, which leads to the development of a hypoglycemic symptom complex;
- Glucagonoma is a tumor (usually malignant) of the alpha cells of the islets of Langerhans that secretes glucagon. A complex symptom complex develops, most often including dermatitis, diabetes, anemia and weight loss. Diarrhea, damage to mucous membranes, thrombosis and embolism are less common.
- Carcinoid is a malignant tumor of neuroendocrine nature. Some tumors are characterized by active secretion and produce serotonin, kallekrein, and prostaglandins. The release of serotonin causes clinical carcinoid syndrome (carcinoid syndrome is characterized by symptoms that are accompanied by rapid redness of the skin of the face and neck, sometimes facial swelling. Often accompanied by tachycardia, hypotension, sometimes attacks of bronchial asthma, gastrointestinal disorders (abdominal pain, diarrhea, severe tenesmus , nausea and vomiting). Attacks can occur under the influence of food intake, alcohol consumption, significant physical activity, emotional reactions.)
- VIPoma – Werner-Morrison syndrome or pancreatic cholera (a neoplasm that produces a large amount of vasoactive interstitial peptide (VIP). The main clinical manifestation of VIPoma is massive prolonged diarrhea), etc.
The functional (hormonal) activity of neuroendocrine tumors is primarily assessed by clinical manifestations. However, clinical manifestations of tumor hormonal activity require laboratory confirmation, i.e. detection of hormones and other biologically active substances in the blood or their metabolites in the urine.
Apudomas may not extend beyond the submucosal layer of the duodenum for a long time. As the size of the tumor increases, features of infiltrating growth and clinical symptoms appear.
Symptoms of duodenal cancer
Sharp abdominal pain may be a symptom of duodenal cancer.
Duodenal cancer is usually asymptomatic in the early stages, but in nine out of ten patients acute symptoms develop as the tumor progresses. This fact indicates the great danger of this form of cancer. Features of symptoms:
- Due to the nonspecific nature of the symptoms, there is a significant delay between the onset of symptoms and diagnosis, on average 7-9 months.
- Nausea, vomiting and intestinal obstruction are typical symptoms of the disease. In half of the patients, the tumor is an incidental finding during surgery for intestinal obstruction.
- Severe abdominal pain and weight loss complicate the clinical manifestations of the disease.
- Sometimes patients with duodenal cancer have traces of blood in their stool.
- Certain types of duodenal cancer present with different symptoms. For example, adenocarcinomas are more often associated with pain and obstruction, while sarcomas and carcinomas are less severe.
- Patients with this disease often experience acid reflux, accompanied by heartburn.
- There may be a sensation of a foreign mass in the abdominal cavity.
- Manifestations of malignant neoplasms of the small intestine are quite subtle during physical examination due to the lack of specific manifestations.
- A soft, distended abdomen may indicate intestinal obstruction.
- Peritoneal signs indicate perforation.
- Jaundice from biliary obstruction or liver metastases is rare.
- Finding blood in the stool is more common in people with benign tumors of the small intestine.
Treatment of small intestine cancer
The issue of choosing a treatment method for patients with malignant tumors of the small intestine is decided collectively at a meeting of the expert council with the participation of professors and doctors of the highest category. If small intestinal cancer is operable, surgeons perform a wide resection of the affected area of the intestine and lymph nodes, and excise the mesentery. The length of the small intestine allows radical removal of the tumor within the boundaries of healthy tissue. The integrity of the digestive tract is restored by performing enterocoloanastomosis (small intestine into large intestine) or enteroenteroanastomosis (small intestine into small intestine).
If duodenal cancer is detected, duodenectomy is performed, sometimes with distal gastrectomy or pancreatic resection. In case of advanced small intestinal cancer, where radical resection is not possible, a bypass anastomosis is performed between unaffected loops of intestine. The surgical stage of treatment of small intestine cancer is supplemented with chemotherapy. The same method in some cases is the only way to treat inoperable malignant tumors.
The long-term prognosis for small intestine cancer is determined by the stage of the cancer process and the histological structure of the tumor. In the presence of localized tumor processes without regional and distant metastases, the five-year survival rate after radical resection is 35-40%.
How to check the small intestine for a tumor? Call the Yusupov Hospital and doctors will conduct a comprehensive examination. Once the diagnosis is confirmed, multidisciplinary treatment will be selected for you. When small intestinal cancer is detected in the early stages during a screening examination, when there are no symptoms of the disease, oncologists have the opportunity to perform radical surgery. After it, the prognosis improves.
Causes of duodenal cancer
Bad habits can cause duodenal ulcers.
First of all, there are the following genetic factors:
- Family history of adenomatous polyposis. Patients with this pathology develop multiple adenomas in all parts of the small and large intestine, which can lead to the formation of adenocarcinoma. After the colon, the duodenum is the most common site of adenocarcinoma.
- Hereditary nonpolyposis colorectal cancer. In addition to colorectal carcinoma, patients with this genetic syndrome also develop neoplasms of the stomach, small intestine, urinary tract, ovaries, and endometrium of the uterus. The risk of developing small bowel adenocarcinoma in patients with this syndrome is 1-4%, which is more than a hundred times the risk in the general population. However, researchers note that genetically determined adenocarcinoma of the small intestine has less aggressive clinical manifestations than those that arise accidentally.
Environmental factors:
- Diet. A 1977 study found that eating animal fat was associated with small intestinal cancer. Another study conducted in 1993 found that eating red meat and smoked meats increases the risk of developing this form of cancer by 2-3 times.
- Tobacco and alcohol. A 1994 study found a link between these bad habits and the occurrence of duodenal cancer.
Predisposing diseases:
- Crohn's disease. In patients with this disease, the risk of developing small bowel cancer increases from 20% to 90%.
- Celiac disease. An increased risk of this form of cancer has been identified in patients with this disease.
Prognosis and survival
If you undergo an examination by a doctor every year, you can detect a tumor already at the first stage. With timely treatment, 90-98% of all patients survive. They are completely cured of the disease. The prognosis for life is favorable.
In the second stage, survival rate for the next 5 years is 70-90%. At the third stage, the rate drops to 40-70%. The forecasts are no longer so favorable. The patient becomes disabled. At the fourth stage, survival rate in the next 4 years is no more than 30%. The disease is difficult to treat.
Diagnosis of duodenal cancer
Detecting the disease in time is very important!
Laboratory research:
- Blood count tests can detect mild anemia associated with chronic blood loss.
- Liver function tests may show hyperbilirubinemia associated with biliary obstruction from periampullary tumors.
- An increase in the level of transaminases in the blood may indicate metastases in the liver.
- Carcinoembryonic antigen levels may be increased.
X-ray signs:
- Plain x-rays of the abdomen may show complete or partial bowel obstruction.
- The overlying gastrointestinal tract has imaging abnormalities in 55-85% of patients with duodenal cancer.
- The image can reveal the localization of the disease and the presence of metastases in the liver.
- Lateral imaging may demonstrate small malignant bowel tumors that are not usually accessible by endoscopy.
- Histological studies are also used.
Classification and stages of development
Oncologists assess the severity of the disease according to certain criteria, which are classified by the international TNM system. A breakdown of the indicators is given below.
T – primary tumor:
- T1 – the formation has not reached 2 cm and has begun to grow into the wall of the duodenum.
- T2 – a node from 2 to 5 cm, affects the muscular layer of the organ.
- T3 – neoplasm exceeds 5 cm, grows beyond the borders of the intestine.
- T4 – tumor cells actively penetrate into neighboring tissues, covering the entire abdominal cavity.
N – damage to peripheral organs of the lymphatic system:
- N0 – not available.
- N1 – isolated manifestations.
- N2 – multiple lesions.
M – distant metastases:
- M0 – not identified.
- M1 – determined.
The development of an oncological tumor goes through 4 stages:
- Stage 1 – the cancerous node is small, has clear boundaries from unchanged cells. Found in mucous and submucosal tissues. Regional lymph nodes are not affected, and there is no distant metastasis.
- Stage 2 – nodular formation up to 5 cm. Malignant development is detected in the muscle layer, myometrium, without affecting the cellular structure of other organs. Single metastases in the lymph nodes begin to occur.
- Stage 3 – the node grows, extends beyond the boundaries of the duodenum and begins to affect the tissues of nearby organs. The size exceeds 5 cm, multiple metastases of the lymphatic system are determined.
- Stage 4 – the neoplasm reaches significant volumes. The stage is incurable, life expectancy is short. Metastases are observed in all systems.
Differential diagnosis
Differential diagnosis is the exclusion of other diseases with similar manifestations when making a diagnosis. Duodenal cancer can hide its manifestations under the symptoms of many diseases of the gastrointestinal tract. Diseases to exclude:
- Ampullary carcinoma.
- Benign tumor of the small intestine.
- Tumors of the bile ducts.
- Chronic gastritis.
- Colon cancer.
- Crohn's disease.
- Stomach cancer.
- Intestinal leiomyosarcoma.
- Intestinal polypoid adenomas.
- Irritable bowel syndrome.
- Pancreas cancer.
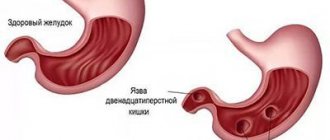
- Peptic ulcer disease.
The symptoms of duodenal cancer are not specific enough for an accurate diagnosis.
A biopsy of duodenal tissue most accurately excludes other diseases.
Types of duodenal cancer
Histopathological subtypes of duodenal adenocarcinoma, depending on the type, may resemble cancers of adjacent organs.
| Phenotype | Histological characteristics | Histologically similar types | Immunophenotypic markers | Forecast |
| Intestinal | Tubular/crib-forming glands lined with columnar tumor cells | Colon adenocarcinoma | MUC2, CD10, CDX2 | + |
| Gastric | Tubular/papillary proliferation with foveal or pyloric differentiation | Gastric adenocarcinoma | MUC5AC, MUC6 | — |
| Pancreatobillar | Simple glands are cuboidal/columnar cells with rounded pleomorphic nuclei; pronounced desmoplastic stroma | Adenocarcinoma of the pancreas and extrahepatic bile ducts | MUC1 | — |
| Uncertain | Low differentiation | No | MUC1 | — |
Consultation with a specialist
Before applying one or another treatment regimen for duodenal cancer, consultation with the following specialists is necessary:
- Gastroenterologist. This specialist clarifies the diagnosis with endoscopy and colonoscopy of the upper gastrointestinal tract.
- Oncologist. This specialist will not only clarify the type of tumor, but will also be able to prescribe radiation therapy. Radiation therapy can also be effective for chronic blood loss associated with tumor growth.
Oncology of the gastrointestinal tract is always associated with the most painful symptoms and rapid spread. Unfortunately, duodenal cancer fits this description perfectly.
Symptoms
Diagnosing an oncological tumor in the initial stages of development is difficult. The person does not experience discomfort or pain. At this time, the node begins to grow, affecting nearby parts of the organ. The disease is discovered by chance during medical examinations using ultrasound.
As the cancer node enlarges, the first signs appear:
- anemia develops;
- there is a decrease or complete absence of appetite, weight loss;
- performance deteriorates.
A growing tumor node is localized on the surface of the small intestine. This leads to a narrowing of the duodenal ducts, the lumen of the organ, due to which bile fluid enters the digestive system, which provokes the following signs of oncology:
- dull pain under the ribs on the right, in the epigastric region;
- attacks of nausea, loss of appetite;
- jaundice.
The pancreas suffers from an enlarged tumor. Inflammatory processes occur in the organ, the structure of the gland becomes loose, its size progresses, and its performance decreases. A doctor may diagnose acute pancreatitis, which leads to severe symptoms and complications. Against this background, pancreatic necrosis occurs with the possible occurrence of peritonitis. Symptoms of oncology with inflammation of the gland are characterized by the following signs:
- feeling of heaviness, pain in the stomach;
- nausea, vomiting;
- feeling of discomfort in the solar plexus area;
- gas formation, flatulence;
- increased acidity with belching and heartburn.
Clinical signs are suitable for various gastrointestinal diseases. The doctor must rule out ulcerative manifestations of the duodenum, stomach and cancerous formations of the large intestine, colon, which are located next to the small intestine. It is also necessary to exclude diseases of the gallbladder and liver. To diagnose a malignant process, additional examinations of the patient are carried out. You should not delay contacting a doctor if you have these symptoms.