The cecum is the initial section of the large intestine. It is located in the right iliac region (lower right in the abdominal cavity) and, due to its structure, is compared to a vertical sac. In the lower part of the cecum there is a vermiform appendix.
The Yusupov Hospital has created all the conditions for the treatment of patients with cancer of the cecum:
- The wards are equipped with forced-air ventilation and air conditioning to provide patients with a comfortable temperature;
- Doctors examine patients using the latest equipment from leading European and American manufacturers;
- For operations on the cecum, surgeons use modern instruments and equipment;
- Oncologists masterfully perform the entire range of surgical interventions known today;
- Medical staff provides professional care before and after surgery;
- Doctors provide antitumor therapy with the latest chemotherapy drugs registered in the Russian Federation.
Patients, as part of scientific research conducted at the clinic, have the opportunity to receive the latest medicines. The growth of a malignant neoplasm can begin in any part of the gastrointestinal tract. Cecal cancer accounts for approximately one fifth of all colorectal cancers.
Causes
The immediate cause of cecal cancer is a cellular mutation that is not recognized by the immune system and not destroyed in time, as a result of which an endless cycle of division and growth of tumor cells is started. Malignant neoplasms of the cecum, according to experts from the World Health Organization, can develop under the influence of the following provoking factors:
- Excessive consumption of red meat that has undergone culinary processing;
- Age-related changes in tissues and weakening of intestinal motility;
- Hereditary predisposition;
- Chronic diseases and pathological conditions of the gastrointestinal tract (inflammatory, ulcerative, dyskinetic, benign neoplastic processes);
- Environmental factors;
- The presence and activity of oncogenic viruses in the body (human papillomavirus and some subtypes of the herpes virus);
- Smoking.
Scientists have not yet established a single reason why a tumor of the cecum develops.
Kinds
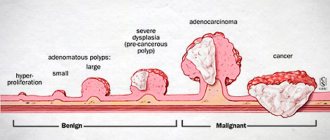
For cecal cancer, the TNM classification is used. In it, T denotes the size of the tumor, N – the presence of lymph node involvement, M – the presence of distant metastases. The disease occurs in 4 stages:
- Stage 0 is characterized by a very small tumor size, damage to only the upper layer of the wall of the cecum, and the absence of metastases in regional lymph nodes;
- In the first stage of cecal cancer, the pathological process spreads to the second and third layers of the colon, but does not grow to the outer side of the intestine, and there are no metastases in the lymph nodes;
- At stage II, the malignant tumor grows on the outer wall of the cecum, the lymph nodes are not affected and no metastases are observed;
- At the third stage of the disease, the tumor begins to grow into nearby organs and tissues, lymph nodes are affected, but doctors do not detect distant metastases;
- At the terminal, fourth, stage of cecal cancer, the malignant tumor begins to grow into adjacent tissues and organs, affecting the lymph nodes and revealing distant metastases.
The following histological types of cecal cancer are distinguished:
- Adenocarcinoma develops from epithelial cells of the intestinal mucosa;
- Signet ring cell carcinoma appears as blisters;
- Undifferentiated cancer is considered the most aggressive form of malignancy;
- Unclassified cancer is a malignant tumor that does not belong to any of the histological forms;
- Squamous cell carcinoma is a tumor of the cecum, which consists of squamous epithelial cells;
- Glandular squamous cell carcinoma is a neoplasm consisting of squamous and glandular epithelium.
Adenocarcinoma of the cecum can be an exophytic or endophytic tumor. It can grow into the lumen of the cecum or penetrate all layers of the intestinal wall. The tumor often grows into the bladder, uterus, appendages, prostate gland in men, small intestine, and abdominal wall. Adenocarcinoma metastasizes most often to the liver, rarely to the lungs, bone system, and brain. Adenocarcinoma can be highly differentiated and poorly differentiated. Cells of a highly differentiated tumor are close to healthy cells and are able to perform their functions. A poorly differentiated tumor consists of degenerated cells that are unable to perform their functions. Favorable prognosis in patients with well-differentiated tumors. Oncologists at the Yusupov Hospital make a diagnosis and prescribe treatment, taking into account the results of a histological examination of the biological material obtained during a biopsy.
Make an appointment
General information
The name intestinal cancer summarizes all types of malignant tumors that affect the human intestine along its entire length. colorectal cancer most often develops , that is, malignant nutrition of the large intestine.
The small intestine is affected much less frequently. According to medical statistics, colorectal cancer is diagnosed in 89% of cases, malignant tumors of the small intestine - in 11% of cases. The ICD-10 code is C20 (Malignant neoplasm of the rectum). Most often, the disease is diagnosed in older people. According to statistics, about 36% of cases of this type of cancer occur in people over the age of 60. Colorectal cancer affects the lining of the colon or rectum. This is a dangerous disease, so people who have been diagnosed with this require immediate treatment.
Colon cancer (ICD-10 code - C18) can develop in different parts of the colon. It consists of the transverse colon, ascending colon, descending colon and sigmoid colon.
Duodenal cancer often develops as a process of metastasis of other types of malignant processes. Primary oncological lesion of the duodenum rarely develops.
When talking about the causes and pathogenesis of the disease, experts combine all types of malignant intestinal lesions. These diseases have similar symptoms and complications. But if the disease is diagnosed at an early stage, treatment is effective. This is why it is extremely important to pay attention to any warning signs and undergo all examinations in a timely manner.
How to recognize the disease, how quickly the pathological process develops and metastases , you can learn from this article. We will also talk about effective treatment regimens for the disease and the prognosis at one or another stage of intestinal cancer.
Symptoms and signs
Malignant tumors localized in the cecum are characterized by a long asymptomatic course. Rapidly progressing subjective discomfort is observed in the later stages of the disease and does not have pathognomonic specificity that would indicate the localization of the tumor in the cecum. Patients present the following complaints:
- Nausea, poor appetite, belching;
- Flatulence, apparently inexplicable alternation of diarrhea and constipation;
- Pain in the right side of the abdomen.
As the tumor increases in size and is damaged by stool, bleeding progresses. It can remain hidden for a certain period and manifest itself with increasing symptoms of anemia and asthenia:
- Apathy;
- Unsteadiness;
- Weakness, fatigue;
- Pale earthy skin color;
- Emaciation.
Frequent or regular discharge of red blood during bowel movements is one of the typical symptoms of colorectal cancer of any location. In the terminal stage of the disease, the following signs of cecal cancer are usually associated:
- Intense pain caused by tumor growth into surrounding structures and pressure on neighboring organs;
- Phenomena of partial intestinal obstruction or complete occlusion of the intestinal lumen;
- Jaundice and liver failure, since the structure of the intestinal system of lymph circulation and blood supply determines the metastasis of the tumor process to the liver.
Prevention of bowel cancer
Proper prevention makes it possible to reduce the likelihood of developing oncological processes in the intestines. However, all preventive measures should be practiced constantly. It is most important to follow these guidelines:
- Quit all bad habits. You should minimize your alcohol consumption and stop smoking.
- Introduce as much fiber into your diet as possible. Dietary fiber promotes intestinal motility and prevents stagnation. It is important to eat fresh vegetables and fruits every day.
- Eat right, minimizing the amount of junk food. It is important to limit the amount of fried foods and fast food.
- Practice physical exercise every day. Physical activity is important to improve peristalsis.
- When the first unpleasant signs appear, you should consult a doctor.
- Regularly undergo preventive examinations. This advice is especially relevant for those diagnosed with Crohn's disease , nonspecific colitis , and intestinal polyposis .
Diagnostics
The preliminary diagnosis of “cecal cancer” is established by specialists at the oncology clinic during the collection of complaints and anamnesis, and clinical examination. A large tumor can be detected during palpation of the abdomen. For the purpose of differential diagnosis, to clarify the location, shape and size of the tumor, and to identify metastases, additional research methods are carried out:
- Colonoscopy;
- Irrigoscopy;
- Computed tomography;
- Ultrasound screening;
- Diagnostic laparoscopy.
During an endoscopic or laparoscopic examination, doctors necessarily select material for histological analysis, which allows them to come to unambiguous diagnostic conclusions. The most informative method for diagnosing sigmoid colon cancer is rectoscopy. With sigmoidoscopy, up to 25 cm of the distal colon is examined.
The use of a flexible sigmoidoscope and colonoscope allows for more accurate preoperative diagnosis of cecal cancer. The X-ray method using a double contrast enema has great sensitivity. It allows you to detect small tumors. A malignant neoplasm manifests itself in the form of a characteristic narrowing or compaction, which is located in the contrast zone. In doubtful cases, doctors at the Yusupov Hospital repeat the examination or perform a colonoscopy.
Scanning computed tomography with air contrast is becoming increasingly widespread. This method is used when making a final decision about the need for surgical intervention. At the Yusupov Hospital, spiral computed tomography with a small slice thickness, the so-called “virtual colonoscopy,” is widely used to detect cancer of the cecum.
Colon carcinoma cells produce carcinoembryonic antigen (CEA), a tumor marker for cancer. However, it is not specific enough to serve as a reliable indicator of the existence of a tumor. Carcinoembryonic antigen is also found in pancreatitis, inflammatory bowel processes, in smokers and in people who abuse alcohol. The CEA test is used in patients with initially high levels of this tumor marker after surgery. Its level decreases after successful surgery, and an increase in CEA concentration in the postoperative period may be the first sign of tumor relapse.
Doctors at the Yusupov Hospital carry out differential diagnosis of cecal cancer with the following diseases:
- Diverticulosis of the colon;
- Ulcerative and ischemic colitis;
- Irritable bowel syndrome.
Other diseases manifested by rectal bleeding (hemorrhoids, polyposis) make diagnosis difficult. Pain in the right half of the abdomen may indicate the development of acute appendicitis. If the patient has positive symptoms of an “acute abdomen,” he undergoes urgent surgery, during which the true cause of the pain syndrome is determined.
Tubular adenoma of the cecum is a benign neoplasm. It may present with symptoms that resemble those of a cancerous tumor.
Make an appointment
Treatment
One of the key features of cecal cancer is that it is completely and relapse-free in almost 93-97% of cases. This applies only to the initial stages of the disease. Early diagnosis of a malignant tumor is a vital issue. For this reason, doctors at the Yusupov Hospital, if there are symptoms of intestinal diseases, first of all exclude cancer.
Treatment of a tumor of the cecum is always intensive and combined. Oncologists at the Yusupov Hospital use all three main areas of modern oncology - surgery, radiation treatment and chemotherapy.
The priority treatment for this type of cancer is surgical removal of the tumor. Laparoscopy is used to perform surgeries in the initial stages of tumors. During endoscopic operations, surrounding tissues are minimally damaged.
For growing tumors, a wide resection of the affected cecum and mesentery is performed, and the lymphatic apparatus is removed. A right hemicolectomy is performed: the surgeon removes up to 20 cm of the terminal ileum, the right half of the colon, including the ascending colon, the cecum, the right third of the transverse colon and the hepatic curvature.
In case of multiple damage to organs and tissues by metastases, surgery to remove tumors is not performed; severe symptoms - intestinal obstruction - are eliminated; antibiotic therapy, chemotherapy and palliative treatment are prescribed. Good prognosis for patients with no metastases in regional lymph nodes.
Conservative therapy for cecal cancer at the Yusupov Hospital is carried out if surgical intervention is not possible. Doctors at the Oncology Clinic use the latest equipment from leading global manufacturers for radiation therapy and the latest generation of antitumor drugs. They are effective and have a minimal range of side effects.
Exposure to cytostatic drugs can reduce the size of the tumor, which increases the chances of its successful removal. Systemic chemotherapy destroys the smallest cancerous foci and prevents tumor recurrence after surgery. Depending on the histological nature of the tumor, the patient’s response to chemotherapy drugs, doctors at the Yusupov Hospital use monochemotherapy (prescribe one cytostatic drug that effectively affects a given type of cancer cell) or polychemotherapy - a combination of several different types of drugs that have a destructive effect on the tumor.
Radiation techniques are used in preparation for surgery as a way to reduce tumor mass. At the Yusupov Hospital, radiotherapy is performed using modern equipment. Linear accelerators generate radiation that, with extreme precision, only affects mutated tissue without affecting healthy cells. The power of the equipment allows you to reduce the time of the session, thereby the effect on the entire body is more gentle.
Treatment of cecal cancer includes radiosurgical methods, in particular, the use of a Cyber Knife. The installation allows you to focus 150-300 thin rays at one point. They hit the desired target from different angles, without having a detrimental effect on healthy tissue. Where the rays intersect (in the tumor of the cecum) a high level of radiation is created. Thanks to high-dose precision irradiation, the number of sessions can be reduced to 2-5.
In some cases, doctors use specialized radiation therapy methods: intraoperative radiation therapy or brachytherapy. These types of radiation treatments help get rid of small tumors that cannot be removed with surgery. Intraoperative radiation therapy is performed during surgery. In this case, a high single dose of radiation therapy is used to destroy a hard-to-reach tumor of the cecum.
Brachytherapy is carried out using tiny SIR spheres containing a radioactive substance called yttrium-90. It is used for secondary liver cancer arising from a malignant tumor of the cecum, when surgery is not an option. The method allows you to slow down the growth of cancer cells.
If cecal cancer is at the first stage of development, there is no tumor growth into neighboring organs or metastases, laparoscopic tumor removal is performed at the Yusupov Hospital. This is a minimally invasive method that is most gentle for the patient. The surgeon does not need to make extensive incisions. Surgical intervention is carried out through several punctures of the anterior abdominal wall.
For more extensive lesions, oncologists excise the damaged area of the intestine with adjacent tissues and perform an anastomosis - restoring the integrity of the intestine, creating a bypass for food, suturing the two sections of the intestine. In some cases of cecal cancer, in order to avoid tumor spread to neighboring organs, surgeons perform resection of regional lymphatic vessels and nodes along with the tumor, en bloc. If it is not possible to save the organ, surgeons remove not only the cecum, but also a section of the small or large intestine. Next, a colostomy is formed - an opening for the removal of intestinal contents. Through it, feces enter the colostomy bag, which the patient wears.
In some cases, a colostomy is performed for a short period of time to optimize the bowel healing process. It can also be permanent. With modern surgical methods used by oncologists at the Yusupov Hospital, and the use of radiation therapy, treatment with modern chemotherapy drugs before surgery, most patients with cecal cancer do not require a permanent colostomy. The competent use of antiblastic techniques by surgeons at the oncology clinic, cleaning the tumor removal site from the slightest remaining atypical cells, significantly reduces the risk of relapse in patients at the Yusupov Hospital.
Probability of relapse
In the first 2 years after achieving remission, 40-60% of patients experience relapses of the oncological process. By the end of the 3rd year, the number of patients with relapses reaches 70%. The prognosis for treatment of liver metastases and the likelihood of relapse are influenced by the malignancy of the primary tumor and metastases, their location, size and effectiveness of the treatment regimen.
The presence of metastases significantly worsens the course of the oncological process, but modern medicine allows us to achieve positive results in such difficult cases. For us at SM-Clinic there are no hopeless patients. We always fight for the patient - to either completely defeat the disease, or to prolong the patient’s life and improve its quality.
We treat liver metastases with a multidisciplinary team of specialists. Every year new technologies and drugs appear, which we are intensively mastering, that is, the capabilities of our doctors are constantly growing. To consult a specialist, please contact us.
Information verified by an expert
Mikhailov Alexey Gennadievich operating oncologist, doctor of the highest qualification category, Ph.D. experience: 21 years
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Prognosis for cecal cancer
The prognosis for malignant neoplasms of the cecum depends on the depth of germination of the primary tumor, the presence of regional and distant metastases. The five-year survival rate directly depends on the stage of cecal cancer. This figure has increased over the past few decades. This is due to careful diagnosis and modern treatment methods used by oncologists at the Yusupov Hospital.
The patient's prognosis after tumor excision depends not simply on the presence or absence of metastases to regional lymph nodes, but on the number of affected lymph nodes. Unfavorable factors that worsen the prognosis for cancer of the cecum include tumor growth into fatty tissue, perforation of the colon, low degree of differentiation of cancer cells, spread of cancer to adjacent tissues and organs, and spread of the tumor into the lumen of large veins.
The five-year survival rate for stage II cecal cancer is 85%. If a diagnosis of stage 3 cecal cancer is established, the prognosis for five-year survival is 74%, and with the fourth stage of the tumor process, 6% of patients survive up to five years. For this reason, oncologists at the Yusupov Hospital do not recommend postponing a visit to the doctor if signs of intestinal discomfort appear. Call at any time of the day. The contact center of the Yusupov Hospital is open seven days a week and without a lunch break.
Make an appointment
1.General information
There are several main sections in the human large intestine: colon, the longest intestine; the sigmoid colon as the lower continuation of the colon and the transition to the rectum; the rectum ending in the anus. The cecum refers to the initial section of the large intestine. It is located on the right and, due to its structure, is most often compared to a vertical bag. In the lower part of the cecum there is a vermiform appendix (literally “appendage”), which for a long time - and, as later studies showed, erroneously - was considered a functionally useless rudiment.
Colon cancer today is an acute, globally significant problem, occupying a leading position in the overall volume of oncopathology and in the lists of causes of mortality; Moreover, mortality in a given localization of the tumor process tends to increase. Even the most developed countries of the world, forced to expend enormous resources and efforts on implementing national screening programs for early diagnosis (which is critically important in this case), are with great difficulty and so far only slightly restraining this alarming trend, due to a number of factors of modern civilization.
It is known that the growth of a malignant neoplasm can begin in any part of the gastrointestinal tract (as, in fact, in any zone of the body in general), however, due to anatomical and functional features, this probability, etiopathogenesis and risk factors for different localizations are not the same. Cecal cancer accounts for approximately one fifth of all colon cancers.
A must read! Help with treatment and hospitalization!