The duodenum (DU) is the upper part of the small intestine. A piece of intestine 20-30 centimeters long. Responsible for changing the pH level to optimal values for the intestines. Regulates the acidity of juice coming from the stomach. The shape of this organ is different for each person. The most typical forms are observed, resembling loops, horseshoes, letters P or S.
Divided into four parts: upper, lower, ascending and descending. The upper part has the shape of an onion, the mucous membranes are folded in the horizontal direction. In other parts, the folds of the mucous membrane are transverse.
Concept of diverticular disease
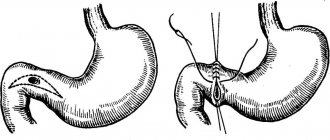
Diverticula are sac-like protrusions on the walls of an organ. The size of diverticula is 5-10 millimeters. Formations up to 5 mm usually do not cause patient complaints and are asymptomatic. Peripapillary and parafateral intestinal diverticulum are almost always false, since they consist only of a mucous layer with small vessels protruding between the muscle fibers.
Diverticula in the intestinal wall
Diverticular disease is divided into three main types: diverticulosis, diverticulitis, and diverticular bleeding.
Duodenal diverticula are hernia-like formations on the walls of the upper intestine. It often occurs in people over 60 years of age, mainly in obese people, equally in men and women. The intestine is prone to the formation of diverticula because it is a hollow organ.
Diverticular pouches are located along the entire length of the duodenum, but most often on the inner side in the middle part. They can also be located along the entire length and acquire enormous sizes. The danger of diverticula is that they compress the bile duct, causing icteric symptoms. Chronic pancreatitis is often a consequence of diverticular disease.
The duodenal diverticulum can be parapapillary or parafaterial in location.
Causes of development of duodenal diverticula
There is no medical consensus on the reasons for the formation of diverticula in this part of the intestine. It is a well-known fact that for diverticulosis to occur, one of three conditions must be met:
- Weakened tissues that form organs.
- High intraintestinal pressure.
- Pressure outside.
Factors causing diverticular diseases can be either congenital or acquired. In persons with congenital pathologies in the form of weak walls of the duodenum, the disease develops at a young age. But there are few such cases in medical practice. From this we can conclude that most cases of diverticula in the duodenum are caused by acquired factors. A large group of provocateurs belongs to the group of natural age-related changes.
Age-related changes leading to the formation of diverticula:
- Loss of tissue elasticity, stretched intestinal wall.
- Atrophy of the abdominal muscles.
- Muscle separation.
- Hernias in the groin and navel and others.
Diverticulosis can be congenital. As a rule, this is accompanied by other pathologies of the gastrointestinal tract.
Symptoms
Duodenal diverticulitis has few symptoms. In most cases, patients do not know about their disease. Identified by chance during the diagnosis of concomitant diseases. In some cases, symptoms are moderate or intense.
Symptoms are often simulated; complaints are similar to signs of the following diseases:
- Ulcer.
- Dyspepsia.
- Diseases of the liver and gall bladder.
- Pancreatic diseases with weight loss.
According to the severity of complaints, diverticula are divided into:
- Asymptomatic.
- Pancreatic.
- Ulcerous.
Common complaints of patients with diverticulosis:
- Abdominal pain in the area of the lower right rib is a characteristic symptom.
- Increased pain after eating and overeating.
- Nausea.
- Heartburn.
- Belching with an unpleasant odor.
- Diarrhea.
- Intestinal obstruction and diarrhea with complications.
Publications in the media
Gastric diverticula are a congenital defect in the development of the stomach. In 75% of cases, they occur on its posterior wall near the lesser curvature (usually at a distance of 2 cm from the esophagogastric junction). In the absence of bleeding or perforation, the course is asymptomatic. Clinical manifestations occur when the diverticulum becomes inflamed; the symptoms resemble the clinical picture of a gastric ulcer. Pseudodiverticula (usually localized in the antrum of the stomach) are the consequences of scarring of a peptic ulcer.
Duodenal diverticula are the second most common after colon diverticula (10% of all gastrointestinal diverticula); most often congenital. Only 4–5% of diverticula are accompanied by clinical manifestations. Diverticula can be single or multiple (25–30% of cases). Duodenal diverticula are classified as so-called pulsatile diverticula; pulsation is caused by contractions of the smooth muscle layer of the intestine. Diverticula may be complicated by severe bleeding or perforation. For uncomplicated diverticula, no treatment is required.
• Approximately 70% of duodenal diverticula are localized in the area of the major duodenal papilla (usually at a distance of 1–2 cm); they are the ones that most often cause clinical symptoms (for example, pancreatitis, cholangitis, jaundice, bleeding).
• Sometimes the common bile duct opens directly into the diverticulum, which prevents normal emptying of the biliary tract with possible obstruction.
Clinical picture
• Clinical signs occur only in cases of complications.
• Diverticula of the upper horizontal section manifest clinical symptoms of peptic ulcer disease, which is associated with the entry of acidic contents into the diverticulum and the occurrence of erosion and ulcers in it.
• A diverticulum of the descending intestine, when an inflammatory process occurs, can cause compression of the major duodenal papilla (papilla of Vater) with the subsequent development of cholangitis, pancreatitis, obstructive jaundice. A direct transition of inflammation to the pancreas with the development of chronic pancreatitis is also possible.
• Diverticula of the lower horizontal part with the development of diverticulitis can cause compression of the duodenum and lead to its obstruction.
Diagnostics. The diagnosis is made on the basis of the clinical picture, contrast X-ray examination of the stomach and duodenum, and endoscopy.
TREATMENT
• Treatment is mainly conservative, aimed at curing and preventing diverticulitis.
• With frequent recurrences of complications, large sizes of the diverticulum, surgical treatment is indicated •• During surgery, to detect the diverticulum, air insufflation is carried out through a probe inserted into the duodenum, or endoscopy is performed on the operating table •• After the diverticulum is detected, it is immersed and the muscular membrane defect is sutured intestines. For large diverticula, gastric resection is sometimes performed using the Billroth II method.
The prognosis is favorable
ICD-10 • K31.4 Gastric diverticulum • K57 Diverticular disease of the intestine
Diagnostics
Instrumental and laboratory examination methods are used:
- Study of the clinical picture and collection of anamnesis. The patient's intense complaints, data on concomitant diagnoses and hereditary diseases are collected and diagnosed.
- Colonoscopy. Rarely used due to the risk of damaging the diverticulum.
- X-ray examination. Reliable and informative method. Before the invention of the X-ray machine, diverticular disease was diagnosed only at autopsy after the death of the patient, when the diseased organ could be examined. When diagnosing diverticulosis, the entire gastrointestinal tract and esophagus are examined by x-ray. Before making a final diagnosis, x-rays are prescribed 2-5 times to clarify the details of the disease.
- CT scan. The advantage of computed tomography is that the results of the study can be saved. Using a tomogram, it is possible to examine simple uncomplicated diverticulosis in cases where x-rays are powerless (especially complex diverticulum). Informs about complications and diseases of nearby organs.
- Colonography. They are used primarily when deciding on an operation.
Diagnosis of diverticula
The main methods used in the diagnosis of duodenitis are as follows:
- Gastroduodenoscopy is the most informative method that helps to determine or exclude the disease. This endoscopic procedure determines whether there are inflammatory processes on the mucous membrane, whether erosions, duodenal ulcers, or duodeno-gastric reflux have developed. The study is carried out on an empty stomach with possible preliminary sedation of the patient.
- Colonoscopy and irrigoscopy to examine the large intestine (usually performed under anesthesia).
- X-ray examination with contrast agent.
- Contrast computed tomography may be needed.
- When contacting a clinic for diagnostics, you must remember that most of the proposed procedures are performed on an empty stomach. A preliminary consultation with a gastroenterologist will allow you to properly prepare for the tests, which will significantly increase their information content.
Complications
Dverticulitis can become acute. In this case, we talk about complications. These are inflamed diseases of the sac-like formation. A prerequisite for the development of diverticulitis is the presence of perforations of various sizes in the walls of the neoplasm. When the diverticulum fills with food and mucus, the pressure inside increases and perforation occurs. Diverticulitis can be simple or complicated. Simple ones account for 75% of all cases.
If the pain radiates to other parts of the abdomen, an infection not only of the duodenum, but also of other organs is suspected. Inflammation is characterized primarily by increased body temperature.
When conducting diagnostics, the following diagnoses are excluded:
- Carcinoma.
- Appendicitis.
- Colitis.
- Inflammation of the pelvic organs.
Detected using X-ray examination, computed tomography, ultrasound, irrigoscopy and endoscopy. Diverticulitis is often accompanied by an abscess.
Obstruction
Obstruction is the complete obstruction of a hollow organ. Duodenal obstruction is rare. More often there is partial obstruction due to swelling and spasms of the intestinal muscles.
Abscess
When the intestinal tissues are unable to limit inflammation (reduced immunity), an abscess begins. This is an inflammation of the tissues surrounding the intestine with the formation of pus. In this case, the infected tissues dissolve, exfoliate and change their structure. Even the stomach is involved in the process.
Symptoms of an incipient abscess: increased body temperature that does not respond to antibiotics and antipyretics and formations that are painful on palpation.
Almost all intestinal abscesses are treated with antibiotics. Drainage through a puncture in the skin is also used as one of the most effective tools.
Fistula
Fistula occurs in 2% of cases, but affects the quality of life of patients. Can be single or multiple. Colovaginal or colovasical fistulas occur.
Perforation
Perforation of the peritoneum occurs rarely with severe immunosuppression. The complication gives an extremely high mortality rate of 35%. Urgent surgery is inevitable!
Bleeding
When bleeding occurs, cancer is suspected, since 90% of all rectal bleeding is associated with cancer. It begins suddenly, very profusely, requiring urgent hospitalization and blood transfusion.
In 40% of cases, diverticular bleeding recurs.
When diagnosing and treating it is necessary to establish the source of bleeding, this is often not possible to do.
Symptoms of intestinal diverticulum
Symptoms of diverticulosis are similar to those of other intestinal pathologies and consist of changes in stool and discomfort in the abdomen. Pain is the most common symptom that causes complaints to go to the doctor. It may differ in intensity, localization and other characteristics. The following signs indicate colonic diverticulosis:
- the pain is not constant, but recurs regularly;
- worsens after eating, especially if food provokes gas formation;
- discomfort goes away on its own after a few hours;
- complete disappearance of pain is observed after defecation or passage of gas.
The pain is often localized in the left side of the abdomen, sometimes radiating to the anus, lower back, groin area or gluteal area. However, it is most often felt in the left iliac region.
When the right part of the colon is affected, patients experience thickening of the stool, as a result of which they are bothered by regular constipation, which is periodically replaced by diarrhea. If diverticulosis of the left half of the colon occurs, patients experience persistent constipation with bloating and the release of a large amount of foul-smelling gases. At the same time, there may be a false urge to defecate, and mucus discharge with feces.
Sometimes diverticulosis is mistaken for dysbiosis, chronic colitis or colon dyskinesia, since the disease does not have specific symptoms.
Treatment
Conservative therapy is outpatient treatment. Correction of nutrition in order to exclude foods that produce large amounts of feces. If obesity is present, weight is adjusted. After eating, it is recommended to take a special position depending on the location of the diverticula to prevent food stagnation.
Antibiotic therapy. Antibiotics are used for a course of 7-10 days. Improvement occurs after 2-3 days. If therapy is ineffective, a study is carried out for complications.
Antispasmodics are prescribed to relieve pain and tension.
Hospital treatment
Hospitalization is rarely required in severe cases. It is mandatory to prescribe a strict diet with a gentle menu, meals in small portions, with dinner no later than 4 hours before bedtime. Enemas, gastric cleansing, intravenous antibiotics and fluids are recommended, and analgesics are recommended to relieve symptoms. 30% of hospitalizations require surgery.