It occurs in children against the background of a hereditary predisposition, with inferiority of the mucous membrane, insufficient production of immunoglobulins of class A. The onset is provoked by stress, dietary errors, excessive use of medications, and endocrine disorders.
Peptic ulcer disease occurs no earlier than 3 years of age; until then, the child is protected by maternal antibodies. If the mother is infected with Helicobacter, the bacteria enter the baby’s body very early. Infection of a child usually occurs after breastfeeding ends.
Children who subsequently develop peptic ulcers initially have high levels of hydrochloric acid and pepsin, and the protective properties of the mucous membrane are reduced.
The ulcerative defect ranges in size from 0.5 cm (small ulcer) to 2.0 cm (giant ulcer).
Peptic ulcer disease occurs in 4 stages:
- active process with the formation of fresh ulcers;
- initial epithelization;
- complete healing;
- remission stage.
Causes of ulcers in children
Gastric ulcer in children is a chronic disease characterized by a phased course of exacerbations and periods of remission. The clinical picture of peptic ulcer disease, which associates the external manifestations of the disease, is confirmed by endoscopy. The main causes of stomach ulcers in children:
- hydrochloric acid and pepsin juice;
- Helicobacter pylori;
- some non-steroidal drugs;
- Stomach ulcers in children can sometimes be caused by a foreign body entering the stomach.
Also, excessive consumption of carbonated drinks, burgers, chips by children, coupled with the lack of a routine, can be the cause of this disease. In addition, unstable functioning of the autonomic nervous system, decreased gastric secretion, and impaired mucosal regeneration gradually lead to the child developing a stomach ulcer. Therefore, when talking about the reasons for the development of pathology, special emphasis is placed on the individual characteristics of lifestyle, diet and the body itself.
Why does peptic ulcer occur?
Until recently, doctors believed that stress and poor nutrition were the main causes of ulcers in children. Later studies showed that most ulcers develop due to infection with the bacterium Helicobacter pylori. Helicobacter pylori lives and multiplies in the stomach and other organs of the gastrointestinal tract. It can enter the body if a person drinks dirty water, does not wash fruits and vegetables well, or does not follow hygiene rules.
But don't blame the ill-fated bacteria entirely. The reasons for the development of ulcers in children are a combination of factors. Experts divide them into two groups – external and internal.
External reasons
- the child eats food at long intervals;
- eats a lot of fast food;
- Children's diets contain a lot of fried, spicy, salty or smoked foods.
Internal reasons
- hereditary predisposition to peptic ulcer disease;
- there is stress and sleep disturbance;
- infection with the bacterium Helicobacter pylori was diagnosed;
- the child’s stomach intensively produces gastric juice;
- the stomach has impaired motility.
The internal causes of peptic ulcer are revealed after laboratory tests. Only a specialist doctor can prescribe them to a patient.
Symptoms of ulcers in children
In most cases, the symptoms of stomach ulcers in children are similar to those seen in other gastrointestinal disorders. Characteristic signs of an ulcer are burning and/or pain in the epigastrium (epigastric region - the upper and central part of the abdominal cavity), which is especially intense in the early hours and at night.
The pain may spread to the back of the chest. These symptoms may be associated with a feeling of heaviness in the epigastric region after eating (dyspepsia), nausea and/or vomiting. Often, an ulcer appears atypically with vague abdominal pain or even does not cause any symptoms.
The pain of an ulcer is intensified by pressure in the epigastrium. This is extremely important to note as it will help to distinguish the symptom from cardiac pain, which may be located “in the abdomen”, but which is not affected by deep palpation of the epigastrium, and which in any case should always be adequately excluded during the initial examination.
Symptoms of gastric ulcers in children vary depending on the location of the mucosal lesion. Epigastric pain is characteristic of gastric and duodenal ulcers, but sometimes there may be no symptoms or only minor signs (vague dyspepsia or aerogastria, or a feeling of heaviness after eating). However, in some cases, a peptic ulcer may be asymptomatic and suddenly lead to bleeding or another complication.
An esophageal ulcer deserves separate treatment due to the specific mechanisms of its occurrence, which are often associated with the presence of gastroesophageal reflux disease.
A duodenal ulcer mainly presents with burning pain and increased acidity, heartburn, usually after a certain period of time after eating (2-3 hours), nausea, aerogastria, and bad breath. The pain often subsides or is stopped by ingesting milk or food; sometimes pain in the epigastric region occurs on an empty stomach or at night.
With a gastric ulcer, the symptoms in a child include deep, dull pain in the epigastric region, sometimes radiating to the back of the back, as well as pain that occurs immediately after eating or is even aggravated by eating, loss of appetite, a feeling of heaviness, anemia, nausea and vomiting. Eating does not bring relief.
Peptic ulcer is a chronic recurrent disease accompanied by the formation of an ulcer in the stomach and/or duodenum, caused by an imbalance between the factors of aggression and protection of the gastroduodenal zone.
In recent years, cases of peptic ulcer disease in children have become more frequent; currently the disease is registered with a frequency of 1 case per 600 children. Also about diseases, an increase in the proportion of pathologies with severe course and a decrease in the effectiveness of therapy. In this regard, gastric and duodenal ulcers in children represent a serious problem in clinical medicine.
Etiology
The disease develops as a result of the influence of several unfavorable factors on the body, including hereditary predisposition and emotional overload in combination with constant nutritional errors (irregular nutrition, abuse of spicy foods, dry food, etc.). The main causes are considered to be a disorder of the nervous and hormonal mechanisms regulating the activity of the stomach and duodenum, an imbalance between aggressive factors (hydrochloric acid, pepsins, pancreatic enzymes, bile acids) and protective factors (mucus, bicarbonates, cellular regeneration, prostaglandin synthesis).
Ulceration is associated with prolonged hyperchlorhydria and peptic proteolysis, caused by vagotonia, hypergastrinemia and hyperplasia of the main glands of the stomach, as well as with gastroduodenal dysmotility and prolonged acidification of the antrobulbar zone.
An important role in the development of peptic ulcers is played by Helicobacter pylori, which is found in 90-100% of patients in the mucous membrane of the antrum of the stomach.
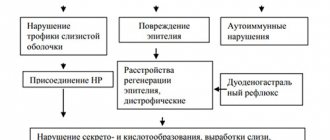
Pathogenesis of peptic ulcer
There are several mechanisms that lead to increased secretion of hydrochloric acid and pepsins, decreased production of mucous substances and impaired motor regulation of the gastroduodenal zone. An important role in this process is played by the central nervous system, which has a dual effect on the secretion and motility of the stomach and duodenum.
Pathological changes in the central and autonomic nervous system play an important role in disrupting the balance between protective and aggressive factors, contributing to the formation of a peptic ulcer.
Classification of peptic ulcer in children
| Ulcer localization | Clinical phase and endoscopic stage | Flow | Complications |
In the stomach:
In the duodenum:
In the stomach and duodenum | Exacerbation:
| Lung Moderate Heavy | Bleeding Perforation Penetration Stenosis |
Clinical picture
The clinical picture depends on the localization of the process and the clinical and endoscopic stage of the disease.
Stage I (fresh ulcer)
The leading clinical symptom is pain in the epigastric region and to the right of the midline, closer to the navel. Pain occurs on an empty stomach or 2-3 hours after eating (late pain). Half of the children report night pain. A clear “Moyniham” rhythm of pain is revealed: hunger - pain - eating - relief. Dyspeptic syndrome is pronounced: heartburn (the earliest and most common symptom), belching, nausea, constipation. Superficial palpation of the abdomen is painful, deep palpation is difficult due to the protective tension of the muscles of the anterior abdominal wall.
An endoscopic examination, against the background of pronounced inflammatory changes in the mucous membrane of the gastroduodenal zone, reveals a defect (defects) of a round or oval shape, surrounded by an inflammatory ridge, with a bottom covered with fibrin deposits of gray-yellow or white color.
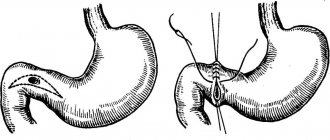
- In the stomach, ulcers are located mainly in the pyloroantral region (found more often in boys).
- In the duodenum, ulcers are localized on the anterior wall of the bulb, as well as in the area of the bulboduodenal junction. Motor-evacuation disorders include duodenogastric reflux and spastic deformation of the bulb.
Stage II (beginning of epithelization of the ulcerative defect)
In most children, late pain in the epigastric region persists, but it occurs mainly during the day, and persistent relief occurs after eating. The pain becomes more dull and aching. The abdomen is easily accessible to superficial palpation, but with deep palpation, muscle protection is preserved. Dyspeptic symptoms are less pronounced.
During endoscopic examination, hyperemia of the mucous membrane is less pronounced, swelling around the ulcerative defect is reduced, and the inflammatory shaft disappears. The bottom of the defect begins to clear of fibrin, convergence of folds towards the ulcer is noted, which reflects the healing process.
Stage III (ulcer healing)
Pain at this stage persists only on an empty stomach; at night, its equivalent may be a feeling of hunger. The abdomen becomes accessible to deep palpation, pain is preserved. Dyspeptic disorders are practically not expressed.
During endoscopy, traces of repair are determined at the site of the defect in the form of red scars of various shapes - linear, circular, stellate. Deformation of the wall of the stomach or duodenum is possible. Signs of the inflammatory process of the mucous membrane of the stomach and duodenum, as well as motor-evacuation disorders, remain.
Stage IV (remission)
General condition is satisfactory. No complaints. Palpation of the abdomen is painless. Endoscopically, the mucous membrane of the stomach and duodenum is not changed. However, in 70-80% of cases, a persistent increase in the acid-forming function of the stomach is detected.
Complications
Complications of peptic ulcer disease are recorded in 8-9% of children. Complications occur 2 times more often in boys than in girls.
- The structure of complications is dominated by bleeding, and with duodenal ulcers they develop much more often than with gastric ulcers.
- Perforation of an ulcer in children often occurs with a stomach ulcer. This complication is accompanied by acute “dagger” pain in the epigastric region, and a state of shock often develops. Characteristic is the disappearance of hepatic dullness upon percussion of the abdomen due to the entry of air into the abdominal cavity.
- Penetration (penetration of an ulcer into neighboring organs) occurs rarely, against the background of a long, difficult process and inadequate therapy. Clinically, penetration is characterized by sudden pain radiating to the back and repeated vomiting. The diagnosis is clarified using FEGDS.
Diagnostics
The diagnosis of peptic ulcer, in addition to the clinical and endoscopic justification outlined above, is confirmed by the following methods.
- Fractional intubation of the stomach with determination of the acidity of gastric juice, flow-hour of hydrochloric acid and pepsin. Characterized by an increase in the pH of gastric juice on an empty stomach and with the use of specific irritants, an increase in the content of pepsins.
- X-ray examination of the stomach and duodenum with barium contrast. Direct signs of an ulcer are a symptom of a “niche” and a typical deformation of the duodenal bulb, indirect signs are pyloric spasm, dyskinesia of the duodenal bulb, gastric hypersecretion, etc.
- Detection of Helicobacter pylori.
- Repeated determination of occult blood in the stool (Gregersen reaction).
Treatment
Treatment of patients with gastric and duodenal ulcers should be comprehensive; it is carried out in stages, taking into account the clinical and endoscopic phase of the disease.
- Stage I - exacerbation phase. Treatment in a hospital.
- Stage II is the phase of subsiding of manifestations, the beginning of clinical remission. Clinical observation and seasonal prevention.
- Stage III is the phase of complete clinical and endoscopic remission. Sanatorium treatment.
Stage I
Conservative treatment of peptic ulcer begins immediately after diagnosis. In many patients, the ulcer heals within 12-15 weeks.
- Bed rest for 2-3 weeks.
- Diet: chemically, thermally and mechanically gentle food. Treatment tables according to Pevzner No. 1a (1-2 weeks), No. 16 (3-4 weeks), No. 1 (during remission). Meals should be fractional (5-6 times a day).
- Reducing the damaging effects of hydrochloric acid and pepsins. non-adsorbable antacids: algeldrate + magnesium hydroxide, aluminum phosphate, simaldrate, etc.;
- antisecretory drugs: histamine H2 receptor antagonists (for example, ranitidine) for 2-3 weeks, H+,K+-ATPase inhibitor omeprazole for 40 days.
Stage II
Treatment is carried out by a local pediatrician. He examines the child once every 2 months and carries out anti-relapse treatment in the autumn-winter and spring-winter periods (table No. 16, antacid therapy, vitamins for 1-2 weeks).
Stage III
Sanatorium treatment is indicated 3-4 months after discharge from the hospital in local gastroenterological sanatoriums and drinking balneological resorts (Zheleznovodsk, Essentuki).
Prevention
Exacerbations of peptic ulcer disease are usually seasonal, so secondary prevention requires regular examination by a pediatrician and the prescription of preventive therapy (antacids), if necessary, diet, limitation of school load (1-2 fasting days per week in the form of home schooling). Providing a favorable psycho-emotional environment at home and at school is of great importance.
Forecast
The course of peptic ulcer disease and long-term prognosis depend on the timing of primary diagnosis, timely and adequate therapy. To a large extent, the success of treatment depends on the position of the parents and their understanding of the seriousness of the situation. Constant monitoring of the patient by a pediatric gastroenterologist, compliance with the rules of seasonal prevention of exacerbations, hospitalization in a specialized department during exacerbation significantly improves the prognosis of the disease.
Source: Children's diseases. Baranov A.A. // 2002.
Complications of ulcers in children
With peptic ulcers, complications occur very rarely, but in any case they can lead to a fatal result:
- internal bleeding;
- perforation;
- formation of scars on the mucous membrane.
When should you see a doctor?
Stomach ulcers in children are not a disorder that can be treated with medication on their own, so if in doubt about the presence of one, you should consult a doctor. We recommend the specialists of our clinic. Our multidisciplinary medical center is located at: Moscow, 2nd Tverskoy-Yamskoy lane, 1.
You should immediately consult a doctor if your child experiences the following symptoms:
- vomiting (especially if it contains blood);
- dark, tarry stools (there may be internal bleeding);
- severe abdominal pain that gets worse;
- unexplained fatigue;
- labored breathing;
- sharp and sudden pain in the abdomen.
You can make an appointment either by phone or by writing in the feedback form on our website. We have pediatric doctors who provide consultations in the center of Moscow.
Diagnosis of ulcers
To find out whether the symptoms indicate the presence of a stomach ulcer in a child, it is necessary to conduct an examination, first collecting an anamnesis and identifying accompanying signs (pain on palpation, swelling, sounds on auscultation). For these purposes the following is assigned:
- Helicobacter pylori:
- Blood analysis.
- Breath test.
- Examination of stool.
- Biopsy.
Ulcer treatment
Treatment of gastric ulcers in children is interconnected with the factors that cause them. Therapy is usually carried out in a comprehensive manner. Its main methods:
- anti-inflammatory therapy;
- proton pump inhibitors;
- antihistamine therapy;
- cytoprotectors.
Ulcer prevention
Before understanding the true causes of peptic ulcers, a scrupulous diet was considered a mandatory step towards healing, but now this fact has not been confirmed by research in modern medicine.
Several years ago, stomach ulcers in children were relieved by systematic consumption of milk, but the relief was short-lived and symptoms recurred after a short time.
For prevention it is advisable to:
- avoid excessive stress;
- avoid sour or spicy foods, which may worsen symptoms;
- do not smoke in the room where the child is;
- Avoid non-steroidal anti-inflammatory drugs, evaluating suitable alternatives with the pediatrician to adjust the child's treatment regimen.