Coxsackie virus: “who” it is and how dangerous it is
The signs, for example, of rotavirus infection are well known to everyone. But what if an intestinal infection, in addition to (or instead of) nausea, vomiting and diarrhea, “gives” herpetic sore throat, rash, damage to the nervous system and a number of other serious disorders? The disease is widespread and, at the same time, not “known” enough. So, meet the Coxsackie virus.
One “family” - one character
The Coxsackie virus got its name “in honor” of a small town located in New York state. Where in 1948, researchers Gilbert Dalldorf and Grace Sickles isolated it while examining the feces of a child with polio. Scientists were looking for a way to treat the latter and a new pathogen was “discovered” by accident.
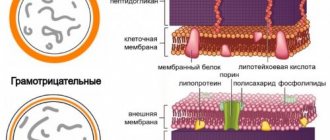
It was called “Coxsackievirus type A” and belongs to the group of enteroviruses. Type B was isolated a year later by Dr. Melnick and his colleagues. As a result of infection of mice with material from children suffering from serous meningitis. Today, serotypes A and B are also divided into subtypes. And the Coxsackie virus type A has at least 23 “variants”, and the serotype B has at least 6.
True, they all have common properties and features characteristic of all representatives of the large family of enteroviruses. And this is also: polio virus, ECHO viruses and a number of enteroviruses that have only an “ordinal” name (68-101).
A distinctive feature of the family is its stability in the external environment.
Enteroviruses:
- are not destroyed by 70% alcohol, 5% Lysol and 3% phenol,
- resistant to changes in acidity (pH from 3 to 10),
- when frozen, they remain active for several years,
- at a temperature of +4 + 6 – several weeks,
- at room temperature – several days.
They tolerate repeated freezing and thawing very well. But they are still sensitive to chlorine solutions (with some “reservation”), and absolutely cannot tolerate temperatures above 50C (death within 30 minutes) and direct ultraviolet irradiation.
Enteroviruses demonstrate a special “predilection” for the tissues of the respiratory, digestive, nervous and muscular systems. Due to which the corresponding symptoms are caused.
“Where” can you find the Coxsackie virus
The main mechanism of infection by the virus is fecal-oral. But for some types the airborne route is also characteristic. The source is always a sick person or an asymptomatic virus carrier.
The release of the pathogen into the environment (the period of “infectiousness”) lasts:
- 3-7 days (from the moment of infection) from the nasopharynx,
- and 3-4 or more weeks - with feces.
Infection most often occurs:
- when eating contaminated food (usually vegetables and fruits)
- water (drinking, when swallowing water from a swimming pool, natural sources),
- and also through “dirty hands”, in contact with household items contaminated with the virus.
The virus “prefers” warm, humid climates. Therefore, it circulates almost constantly in the tropical and subtropical regions. Which causes a high risk of infection at the “resort”. Whereas in temperate latitudes, the risk of the disease is observed mainly in summer and early autumn. Although, according to the latest data, amid the covid pandemic, the seasonality of Coxsackie infection has shifted. And now the “chance” of infection remains until November.
Children are more susceptible to infection than others due to frequent violations of personal hygiene rules and immune system characteristics. And also “overcrowding” in kindergartens and schools.
While adults more often experience the infection in a mild or asymptomatic form. However, there are frequent exceptions here.
How to suspect an infection
The entrance gates of infection, as already noted, are always the mucous membranes of the respiratory or digestive systems. During the incubation period (as the virus “accumulates”), which is an average of 4-6 days, the infected person does not experience any symptoms.
And only after the end of the “incubation” does Coxsackie begin to spread to other tissues of the body, simultaneously provoking the launch of immune mechanisms.
The onset of the disease, if it is not asymptomatic, is often accompanied by:
- a sharp rise in temperature to 39-40C,
- symptoms of intoxication (headache, body aches, etc.),
- abdominal pain,
- nausea and vomiting (including repeated),
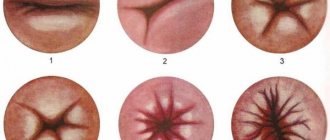
- the appearance of painful herpes-like rashes in the oropharynx (herpetic sore throat)
- as well as a pinpoint red rash on the palms and soles (mouth-palm-sole symptom).
Blisters and rashes may appear on other parts of the body. And the presence of bubbles is always accompanied by severe pain. The rash, at first glance, may resemble chickenpox. However, chickenpox is characterized by a special staged pattern of rashes: first, papules (convex formations on the skin) appear, then they turn into blisters, which eventually open to form ulcers. All “this” is accompanied by itching. And only then does healing occur.
The rash caused by Coxsackie infection is characterized by a dense surface and severe pain. The bubbles do not open. And over time they dry out, leaving dark spots. Patients often experience intense muscle pain. Conjunctivitis may also occur.
At the same time, this “classic” manifestation of infection is more typical for the Coxsackie virus type A. In some cases, the only symptom, for example, may be only a “strange”, prolonged fever or signs of acute respiratory viral infection with an unusually high temperature.
And Coxsackie type B infection, among other things, affects the liver, pancreas, heart and pleura (the lining of the lungs), causing corresponding symptoms and complications.
Dangerous complications
Fortunately, infections caused by the Coxsackie virus do not often cause complications. But at the same time there may be:
- meningitis,
- encephalitis,
- myocarditis (heart damage),
- pericarditis (inflammation of the lining of the heart),
- pleurisy (inflammation of the serous membrane of the lungs),
- organ failure due to severe dehydration,
- hepatitis,
- convulsions and paralysis
Complications are more often observed against the background of immune deficiency or general weakening of the body (due to chronic diseases or other factors). Which makes newborns, infants, the elderly, cancer patients, HIV-infected and some other groups of patients especially vulnerable.
Diagnosis of Coxsackie infection
Laboratory detection of the Coxsackie virus is based on only two tests:
- PCR test of feces to detect the virus itself (RNA)
- or a blood test for IgM antibodies to the virus.
In this case, the first option is used as the main one. Since, let us remember, the excretion of the pathogen in feces continues for about 3-4 weeks from the moment of infection.
Whereas antibody testing is often used as an additional test. When it is necessary to carry out differential diagnosis with other infections that provoke meningitis and other pathologies. And confirmation of the diagnosis is an increase in the level of antibodies by at least 4 times in the period between 4-5 and 14 days of illness.
And after an infection, persistent, and according to some data, lifelong immunity remains.
How to treat Coxsackie virus
As such, there are currently no drugs against the pathogen itself. And all therapeutic measures are aimed at eliminating symptoms.
Among the medicines used:
- "general" antiviral,
- antipyretics,
- antihistamines,
- sorbents,
- drugs that restore water and electrolyte balance (Regidron and others),
- local antiseptics
- and antibiotics, in case of bacterial infection.
At the same time, self-medication for Coxsackie infection is extremely undesirable. If you suspect an infection, and especially if you have a confirmatory PCR test, you must immediately consult a doctor.
A clinical case of a severe illness in patient L., 1 year 4 months, is of undoubted interest for pediatricians, allergists, infectious disease specialists, and dermatovenerologists. The disease arose acutely during the child's stay with his parents on vacation in Egypt and developed rapidly within 4 days. Initially, the patient had a burdened premorbid background: from the first months of life, the child suffered from atopic dermatitis, which was not treated, and there was an allergy to certain foods; vaccinated only with BCG (in the maternity hospital).
He became acutely ill on March 26, 2010 - a runny nose appeared and his body temperature rose to 39 °C. Received treatment with Panadol.
03/27/10 - vomiting 5-6 times, loose stools 7 times a day, body temperature remained at 39 °C. Treatment: Panadol, Efferalgan, suppositories with diclofenac, antibiotic (unknown).
03/28/10 - elevated body temperature and diarrhea persisted, at 21:00 on the plane (during the return to Moscow) the patient was intramuscularly injected with a lytic mixture - no-spa, suprastin, analgin, 0.2 ml each. After this, an infiltrate developed on the buttock at the injection site within 4 hours with necrosis in the center, which increased. Upon returning home, an emergency medical team was called and salt lotions were recommended.
On March 29, 2010, the child was referred by the local pediatrician to the Tushino Children's Hospital (Children's Hospital No. 7). The patient was hospitalized in the intensive care unit with the following diagnosis: acute respiratory viral infection, post-injection abscess, allergic reaction.
Anamnesis of life.
A child from the second pregnancy against the background of duphaston, stimulation of ovulation, with the threat of termination at all stages of pregnancy, the first term birth at the 39th week. Birth weight 3410 g, height 52 cm.
Upon admission to the hospital, the condition is serious. Consciousness is clear. Lethargic, drowsy, psychomotor agitation was periodically noted. The neurological status did not reveal any pathological symptoms.
The skin and visible mucous membranes are pale on a dark background (tan), dry. Mucous membranes are bright, dry. The pharynx is hyperemic. Microcirculation disorders are moderate. On the skin, manifestations of atopic dermatitis in the form of papular elements with excoriation. Tissue turgor is reduced. Body temperature 37.6 °C.
Status localis.
On the right buttock there is a massive widespread necrotic brown-gray lesion with a diameter of 7 cm on a hyperemic base, in its central part there is hemorrhagic impregnation, there are single hemorrhagic papules. Along the periphery of the lesion in the upper and lower sections there are bubbles with transparent contents (Figure, a, b).
Figure 1. Necrotic focus similar to the Arthus phenomenon, which developed at the site of injection of the lytic mixture.
a — close-up, b — general view. Breathing is spontaneous and adequate. No shortness of breath, tachypnea. On auscultation, breathing is carried out on both sides, it is hard, and wheezing of a wire-like nature is heard. The respiratory rate is 30-35 per minute. The cough is productive and infrequent. Hemodynamics are compensated, heart sounds are muffled and rhythmic. Heart rate - 140-145 per minute, blood pressure - 109/60 mm Hg.
The abdomen is soft, not tense, swollen, and sensitive to palpation. Intestinal peristalsis is enhanced. The liver is +2 cm, elastic in consistency, the spleen is not palpable. The stool is copious, watery, greenish in color. Urine is rich and clear. Diuresis is reduced.
Laboratory examination.
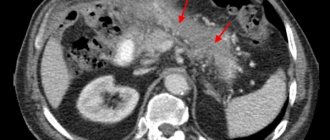
A general blood and urine test was performed (Tables 1, 2),
The blood coagulation system was examined (Table 3).
Acid-base balance, blood gases and electrolytes are normal
Stool test for rotavirus
from 30.03.10 - positive.
Klebsiela pneumonie
was cultured from stool .
Throat culture - Candida albicans
.
The child received the following treatment
:
1) infusion therapy with saline solutions, correction of electrolyte disturbances;
2) antibiotic therapy (claforan 100 mg/kg/day with a trial administration - 25% of the single dose);
3) vascular therapy, antihistamines;
4) hormone therapy (prednisolone 5 mg/kg/day);
5) sorbents, probiotics, enzymes;
6) immunotherapy (kipferon);
7) local therapy (2% aqueous solution of methylene blue, oxycort spray or polcortolone 2 times a day for 3 days).
During treatment, the child's condition improved. On 04/01/10, the patient was transferred from the intensive care unit to the 1st infectious diseases department.
04/07/10 - the child’s condition is satisfactory. The skin of the right buttock has an eroded surface in the stage of epithelization. The child was discharged home under the supervision of a local pediatrician with a diagnosis of moderate rotavirus gastroenteritis, toxicosis with exicosis of I-II degree, toxic-allergic dermatitis.
The severity of the condition of a child with a burdened premorbid background (atopic dermatitis) is due to water and electrolyte disturbances, intoxication against the background of current acute infectious gastroenteritis.
Gastroenteritis in young children is often caused by certain small viruses that do not multiply in cell culture. Rotaviruses also belong to this group. The clinical picture of gastroenteritis depends little on the pathogen and is rather determined by the age of the patient. In infants and young children, gastroenteritis quickly leads to dehydration and electrolyte disturbances; mortality is significant. Fever and vomiting usually appear 2 days before the onset of diarrhea. 40% of patients show signs of respiratory tract damage. In the acute period of the disease, the virus can be detected in feces by electron microscopy [1].
Toxicoderma, or toxic-allergic dermatitis, is caused by toxicoallergic development mechanisms. A common cause of its occurrence is medications (antibiotics, analgesics, etc.), and in young children - often food products.
An acute inflammatory reaction develops on the skin and mucous membranes with a pronounced polymorphism of erythematous, urticarial, papular, vesiculobullous and hemorrhagic efflorescence. Sometimes erythroderma develops. In severe forms of the disease, the child’s general condition is disrupted (malaise, lethargy, increased body temperature to 39 ° C or more).
In fact, Lyell's syndrome is the most severe type of toxicoderma with a possible serious outcome, so this nosology must be included in the range of differential diagnosis.
Lyell's syndrome (toxic epidermal necrolysis) is a severe toxicoallergic, drug-induced disease that threatens the patient's life and is characterized by extensive epidermal detachment and necrosis of the epidermis with the formation of many blisters and erosions on the skin and mucous membranes [1-3]. The disease is similar to scalded skin syndrome (they are caused by the same strains of Staphylococcus aureus). The acute onset of the disease quickly leads to a serious condition (body temperature 39-40 oC, drowsiness, profuse disseminated rash throughout the skin and mucous membrane - red swollen spots, blisters of various sizes with a thin flabby covering, bleeding erosions, hemorrhagic crusts and cracks, excruciating thirst ).
Massive necrosis in the area of the right buttock can be regarded as a development of the Arthus phenomenon (i.e., it is a local hyperergic inflammatory reaction with allergic necrosis of sensitized tissues), as a complication when administering certain medications (most likely, a lytic mixture). The basis of the Arthus phenomenon is the precipitation of the “allergen-antibody” complex in the vascular wall and tissues.
Among the laboratory findings are Klebsiela pneumonie, which is one of the “classical” pathogens of nosocomial infections [4]. Its significance in the pathogenetic aspect is small.
Thus, the presented complex clinical case had a favorable outcome thanks to timely diagnosis and adequate therapy.