Causes of small intestine cancer
Small intestine cancer is a malignant neoplasm of the small intestine: duodenum, jejunum or ileum. In most cases, small intestinal cancer develops against the background of chronic enzymatic or inflammatory diseases of the digestive system:
- Peptic ulcer;
- Celiac disease;
- Duodenitis;
- Enterita;
- Diverticulitis;
- Nonspecific ulcerative colitis;
- Crohn's disease.
Benign epithelial neoplasms of the intestine can transform into a cancerous tumor. Doctors explain the predominant damage to the duodenum by the irritating effect of bile and pancreatic juice on the initial part of the small intestine, its active contact with carcinogens that enter the digestive tract with food.
Increased risk factors for developing small intestinal cancer are sporadic or familial adenomatous polyposis. The likelihood of developing small intestinal cancer is higher for people exposed to radiation or suffering from alcohol addiction, smokers, people whose diet is dominated by canned foods, animal fats, and fried foods. There is a relationship between colon cancer and malignant neoplasms of the small intestine.
Risk factors
Cases of sporadic or familial adenomatous polyposis are increased risk factors for developing small intestinal cancer. The risk of developing small intestinal cancer is higher in:
- Smokers;
- Persons exposed to radiation;
- Suffering from alcohol addiction;
- People whose diet is dominated by animal fats, canned foods, and fried foods.
Based on the nature of the growth of tumor tissue, exophytic and endophytic cancer of the small intestine are distinguished.
- Exophytic tumors grow into the intestinal lumen, causing its narrowing and the development of intestinal obstruction; macroscopically may resemble a polyp or cauliflower;
- Endophytic forms of cancer infiltrate the wall of the small intestine in depth, accompanied by intestinal bleeding, perforation and peritonitis.
According to the histological structure, malignant tumors of the small intestine are more often represented by adenocarcinoma; sarcomas, carcinoids, and intestinal lymphoma are less common in oncological practice.
Symptoms and signs of small intestine cancer
Small intestinal cancer is characterized by polymorphism of manifestations. This is due to the variability of localization, histological structure and size of the tumor. In the initial stages of the disease, patients present the following complaints:
- Periodically recurring cramping pain in the abdomen;
- Stool instability (diarrhea alternates with constipation);
- Nausea and vomiting;
- Flatulence.
If the tumor process progresses, intoxication and weight loss are noted. When a malignant tumor of the small intestine is destroyed, symptoms of intestinal bleeding and perforation of the intestinal wall occur. The contents of the intestine enter the abdominal cavity and lead to peritonitis.
Exophytic growth of tumors may be accompanied by symptoms of obstructive intestinal obstruction. If the neoplasm compresses neighboring organs, intestinal ischemia, pancreatitis, jaundice, and ascites develop.
Sometimes the tumor fusions with the bladder, adjacent intestinal loops, large intestine, and omentum to form a single, sedentary conglomerate. When ulceration and decay of small intestinal cancer occurs, intestinal fistulas occur.
Clinical manifestations of ileal cancer develop gradually. The first symptoms are dyspeptic symptoms:
- Nausea;
- Vomit;
- Violation;
- Motor skills;
- Severe spasmodic colic.
Patients quickly experience a decrease in appetite, an aversion to food, and a decrease in body weight. With multiple tumors, intestinal obstruction occurs. It is characterized by abdominal pain, vomiting first of gastric and then intestinal contents, bloating, dry skin and dehydration. With sarcomas of the small intestine, intestinal bleeding is often observed.
Colon cancer (Colorectal cancer)
Clinical signs of colon cancer are represented by 5 leading syndromes: pain, intestinal disorders, intestinal obstruction, pathological discharge, and deterioration in the general condition of patients. Abdominal pain is the earliest and most consistent sign of colon cancer. Depending on the location of the tumor and the stage of the malignant process, they can be different in nature and intensity. Patients may characterize abdominal pain as pressing, aching, or cramping. If there is severe pain in the right hypochondrium, it is necessary to exclude cholecystitis and duodenal ulcer in the patient; in case of localization of pain in the right iliac region, the differential diagnosis is made with acute appendicitis.
Already in the initial stages of colon cancer, symptoms of intestinal discomfort are noted, including belching, nausea, vomiting, loss of appetite, a feeling of heaviness and fullness in the stomach. At the same time, intestinal disorders develop, indicating a violation of intestinal motility and the passage of intestinal contents: diarrhea, constipation (or their alternation), rumbling in the abdomen, flatulence. With exophytic growing colon cancer (most often left-sided localization), partial or complete obstructive intestinal obstruction may eventually develop.
The development of cancer of the distal parts of the sigmoid and rectum may be indicated by the appearance of pathological impurities (blood, mucus, pus) in the stool. Heavy intestinal bleeding rarely occurs, but prolonged blood loss leads to the development of chronic posthemorrhagic anemia. Violation of general health in case of colon cancer is associated with intoxication caused by the disintegration of the cancer tumor and stagnation of intestinal contents. Patients usually complain of malaise, fatigue, low-grade fever, weakness, and emaciation. Sometimes the first symptom of colon cancer is the presence of a palpable mass in the abdomen.
Depending on the clinical course, the following forms of colon cancer are distinguished:
- toxic-anemic
- general symptoms predominate in the clinic (fever, progressive hypochromic anemia). - enterocolitic
- the main manifestations are associated with intestinal disorders, which requires differentiation of colon cancer from enteritis, colitis, enterocolitis, dysentery. - dyspeptic
- the symptom complex is represented by gastrointestinal discomfort, reminiscent of the clinical picture of gastritis, gastric ulcer, cholecystitis. - obstructive
– accompanied by progressive intestinal obstruction. - pseudo-inflammatory
– characterized by signs of an inflammatory process in the abdominal cavity, occurring with fever, abdominal pain, leukocytosis, etc. This form of colon cancer can be disguised as adnexitis, appendiceal infiltrate, pyelonephritis. - atypical
(tumor) - a tumor in the abdominal cavity is detected by palpation against the background of visible clinical well-being.
Symptoms of duodenal cancer
The most characteristic and first symptom of duodenal cancer is pain. In the early stages of the disease, pain syndrome involves the nerve elements of the intestinal wall in the pathological process. During this period, the pain is constant, aching, and is not associated with food intake. When the process is locally widespread and the cancer tumor grows into the mesentery of the colon and small intestine, the pancreas, the pain becomes burning. Their intensity and duration increase, and a constant feeling of heaviness appears in the epigastric region.
The development of obstruction is manifested by increasing signs of narrowing of the duodenum. Pain from duodenal cancer radiates to the back. This is due to the common innervation of the duodenum with the pancreas, pylorus, liver and gall bladder, and bile ducts. Small bowel high obstruction may develop when small bowel carcinoid spreads to the mesentery. With exophytic growth, cancerous tumors often undergo decay. In this case, the first sign of the disease may be intraintestinal bleeding.
Cancer of the major duodenal papilla (ICD-10 code C24) causes increased pressure in the biliary zone and the development of obstructive jaundice. Small intestinal carcinoid is characterized by the development of paraneoplastic syndromes that are associated with the production of hormones. Their symptoms are hot flashes, arrhythmias and bronchospasm.
The first symptom of a malignant tumor of the major duodenal papilla is often obstructive jaundice, which occurs against the background of somatic well-being. Initially, the jaundice is intermittent. Normalization of biochemical blood parameters is due to a decrease in edema in the area of the stenotic bile duct. As cancer of the papilla of Vater progresses, jaundice becomes more persistent. After intense pain, accompanied by chills and heavy sweats, patients' skin color changes. Patients complain of severe itching. The transient nature of jaundice in the later stages of the disease is due to the disintegration of cancer of the major duodenal papilla, which is accompanied by a temporary restoration of the patency of the bile duct.
When palpating the abdomen, doctors determine an enlarged liver. In 60% of patients, an enlarged gallbladder is felt under the lower edge of the liver. With prolonged obstruction of the biliary tract, liver cirrhosis and chronic pancreatitis occur. If cancer of the major duodenal papilla grows into the intestinal wall, bleeding may occur with the subsequent disintegration of the tumor. With regional metastasis, the pain syndrome changes.
A characteristic feature of cancer of the major duodenal papilla is early weight loss. The reason for weight loss is the narrowing or blocking of the lumen of the pancreatic ducts, due to which the enzymes that are so necessary for the breakdown of fats and proteins cease to flow into the digestive tract. Weight loss and vitamin deficiency cause muscle weakness.
Patients with cancer of the major duodenal papilla often experience diarrhea. They are accompanied by bloating and abdominal pain. The feces are clayey-gray and foul-smelling. In advanced cases, fatty stool may be detected. When regional metastases appear, the nature of the pain syndrome changes. In the later stages, depletion and dysfunction of organs that are affected by distant metastases are determined.
Colon cancer (colorectal cancer) - symptoms and treatment
Surgery
Surgery is the main method of radical tumor removal. In the early stages of the disease, only its implementation is sufficient. For common processes, treatment is always complex: in addition to surgery, radiation therapy, chemotherapy and targeted therapy may be required. For minimally invasive neoplasms, gentle organ-preserving interventions are performed, which are performed endoscopically [1]. In other cases, resection (removal) of the intestine in compliance with the rules of ablastics:
- the tumor is removed en bloc with the tissues involved in the process: regional lymph nodes are also subject to removal. In addition to the therapeutic purpose, removal of lymph nodes also has a valuable diagnostic value - their morphological study provides information about the presence of metastases and helps to accurately determine the stage of the process. This has an impact on further treatment tactics, in particular the need to prescribe postoperative chemotherapy or radiation therapy;
- there must be a sufficient distance from the visible edge of the tumor to the edge of resection - ideally, about 30-40 cm of intestine is removed. The resulting material is sent for urgent histological examination to determine the presence of tumor cells at the resection margins.
For rectal cancer, radical treatment involves chemoradiotherapy . In some cases, this allows you to save the rectum and anal sphincter.
Surgical treatment can be performed in one or two stages . In one-stage treatment, tumor removal and restoration of intestinal continuity are performed during one operation, when the resection edges are connected by anastomosis . This is possible if several conditions are met:
- the connected areas are sufficiently supplied with blood;
- there is no tension in the stitched areas;
- low risks of infectious complications.
If these conditions are not met, there is a high probability of developing anastomotic leakage, necrosis and infectious complications. To avoid this, two-stage interventions are performed. At the first stage, the tumor is removed, and the adducting end of the intestine is brought to the anterior abdominal wall in the form of a colostomy, through which the intestinal contents will be released.
After the patient completes antitumor treatment, the results of which are satisfactory, doctors carry out reconstructive interventions to restore intestinal continuity.
If there are distant metastases, it is recommended to remove them surgically at the same time as the primary tumor. Such operations are called simultaneous and are performed by a combined team involving surgeons of related specialties [5].
Endoscopic stenting
One of the common complications of colorectal cancer is intestinal obstruction. In addition, with metastasis to the liver, obstructive jaundice can develop. Both conditions are life-threatening and require immediate medical attention. One of the methods to solve the problem is stenting - installation of a special frame that ensures straightening of the pathologically narrowed area. In case of intestinal obstruction, the introduction of a stent into the site of obstruction straightens the tumor masses, allows you to expand the intestinal lumen and ensure the free passage of intestinal contents. Thus, intestinal obstruction is relieved, which makes it possible to more thoroughly prepare for surgery. This is especially important in oncology practice, since such patients, for example, have time to undergo neoadjuvant chemotherapy. In patients at high risk of surgical or anesthetic complications, stenting is the main method of correction of intestinal obstruction.
With the development of obstruction of the bile ducts, a similar intervention is performed on the hepatobiliary system . Using an endoscope, a stent is inserted into the narrowing site through the common bile duct, which is located in the duodenum. Alternatively, bougienage and balloon dilation may be used.
Chemotherapy
Chemotherapy for colon cancer is carried out after surgery (adjuvant) and is prescribed in the following cases:
- presence of regional metastases;
- involvement of the entire thickness of the intestinal wall in the process;
- poorly differentiated tumors;
- the presence of malignant cells at the resection margins.
Neoadjuvant chemotherapy treatment of primary unresectable tumors is also possible. In this case, several courses of chemotherapy are prescribed, and after their completion, the possibility of radical surgery is re-evaluated.
Chemotherapy is recommended to be prescribed no later than 28 days from the date of surgery (in the absence of contraindications). In this case, the main therapy lasts 3-4 months, after which maintenance therapy is carried out.
Treatment can be supplemented with targeted drugs - bevacizumab, cetuximab, panitumumab. These drugs act on specific processes that determine the vital activity of tumor cells. They are prescribed after molecular genetic testing. Some drugs are used only with chemotherapy, others can be used both in monotherapy and as part of combination therapy [2][5].
Targeted therapy
Targeted drugs act on cellular mechanisms that ensure carcinogenesis - the process of formation and development of a malignant tumor. They cannot completely destroy cancer, but they significantly slow down its growth and progression. Due to their highly specialized action, these drugs are prescribed only after special tests are carried out that reveal the presence of mutations for which targeted therapy is indicated or, conversely, is ineffective.
For example, adding bevacizumab, cetuximab, or panitumumab to standard chemotherapy regimens for the treatment of metastatic colon cancer increases overall survival from 18 months to 29 months. Bevacizumab inhibits the activity of endothelial growth factor, which reduces tumor vascularization. Cetuximab and panitumumab act on the epidermal growth factor receptor (EGFR), which is responsible for the differentiation, proliferation and survival of malignant cells.
Radiation therapy
Radiation therapy is mainly used in the treatment of rectal cancer, since other parts of the intestine have pronounced physiological mobility, which makes it impossible to clearly position the tumor for planning radiation fields [3]. In other cases, it is used for palliative purposes for the treatment of distant metastases.
For rectal cancer, radiation therapy is used as part of a combination treatment together with chemotherapy. In some cases, this makes it possible to carry out organ-preserving treatment without removing a colostomy [3].
Dispensary observation
Once treatment for colon cancer has been successfully completed, there is still a risk of recurrence. It is highest during the first three years, so all patients require regular follow-up. Typically, doctor's examinations, ultrasounds and blood tests for carcinoembryonic antigen (CEA) are carried out at the following frequency:
- in the first 2 years - every 2-3 months;
- over the next 3 years - every six months;
- then - annually.
In addition, it is necessary to undergo a colonoscopy every two years. If pathological changes are detected during these examinations, the doctor will prescribe a computed tomography scan, bone scan and other diagnostic methods.
Features of rehabilitation
After surgery for colon cancer, the doctor gives standard recommendations regarding nutrition and return to physical activity. The recovery time depends on the type of surgery and the method of performing it (endoscopic, laparoscopic or open through an incision). If the patient has a permanent colostomy, they will be told how to properly care for it before discharge.
Some chemotherapy side effects persist after treatment is completed. In this case, the doctor will prescribe the necessary treatment to relieve them and give the patient recommendations on lifestyle. Many people who have recovered from cancer experience psycho-emotional problems and are constantly afraid of relapse. In such cases, the help of a psychologist is required.
Diagnosis of small intestine cancer
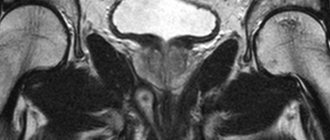
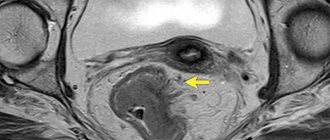
For a malignant tumor of the duodenum, doctors at the Yusupov Hospital perform fibrogastroduodenoscopy and contrast fluoroscopy. Colonoscopy and irrigoscopy are informative for diagnosing cancer of the terminal ileum.
Barium passage X-ray allows you to identify obstacles to the advancement of the contrast agent, areas of narrowing and suprastenotic expansion of the intestine. During an endoscopic examination, the doctor performs a biopsy for subsequent morphological verification of the diagnosis. In cases that are difficult to diagnose, selective angiography of the abdominal cavity is performed.
In order to identify metastases and germination of small intestinal cancer into the abdominal organs, a comprehensive examination of patients is carried out at the Yusupov Hospital:
- Ultrasound examination of the liver, pancreas, kidneys, adrenal glands;
- Multislice computed tomography of the abdominal organs;
- Chest X-ray;
- Bone scintigraphy.
Small intestinal cancer is differentiated from benign tumors, intestinal tuberculosis, occlusion of mesenteric vessels, and Crohn's disease. In women, differential diagnosis is carried out with neoplasms of the uterus and appendages.
Perforation of the colon (Colon perforation)
Perforation of the colon is characterized by clinical symptoms of acute abdomen. Patients complain of intense pain, hold their stomach with their hands, spare it when breathing, try to remain motionless, taking a forced position on their side or on their back with bent legs. The body temperature of patients with intestinal perforation is increased first to subfebrile and then to febrile levels. Weakness, pale skin, nausea, vomiting, decreased amount of urine, tachycardia and breathing problems are noted. The abdomen is distended, the anterior abdominal wall is tense. The pain intensifies with palpation, especially severe pain is detected in the perforation area.
Some time after colon perforation, the intensity of the pain syndrome decreases as the peritoneal receptors adapt to pathological changes in the abdominal cavity. With the development of peritonitis, pain and tension in the abdominal wall intensify, become diffuse, spreading to all parts of the abdomen. When percussing the liver in patients with colon perforation, the disappearance of hepatic dullness is determined, indicating the presence of gas in the abdominal cavity. In sloping areas of the abdomen, dullness of sound may be detected due to the presence of fluid. Auscultation determines the weakening or disappearance of intestinal sounds due to disturbances in peristalsis.
In the presence of diverticulitis, complicated by an abscess with subsequent perforation of the colon, an infiltrate may be detected during digital examination of the rectum or palpation of the abdominal area. In some cases (usually with malignant tumors or the formation of adhesions), perforation of the colon does not occur in the abdominal cavity, but in a nearby organ, for example, in the vagina or bladder. In such cases, an enterovaginal or enterovesical fistula is formed, accompanied by the release of gases and intestinal contents from the urethra or vagina.
Features of the clinical picture of colon perforation depend on the level of perforation, the size of the perforation hole, and the presence or absence of colon obstruction. As a rule, proximal damage to the colon is more severe due to the rapid dissemination of liquid intestinal contents throughout the abdominal cavity. The exception is when colonic perforation is caused by intestinal obstruction. In such cases, periods of false well-being, caused by a decrease in the pressure of the contents on the intestinal wall, are more pronounced than usual. Sometimes perforation of the colon occurs with vaguely defined symptoms due to the small size of the perforation hole or the proximity of the omentum, which prevents the contents from exiting into the abdominal cavity.
Treatment of small intestine cancer
The issue of choosing a treatment method for patients with malignant tumors of the small intestine is decided collectively at a meeting of the expert council with the participation of professors and doctors of the highest category. If small intestinal cancer is operable, surgeons perform a wide resection of the affected area of the intestine and lymph nodes, and excise the mesentery. The length of the small intestine allows radical removal of the tumor within the boundaries of healthy tissue. The integrity of the digestive tract is restored by performing enterocoloanastomosis (small intestine into large intestine) or enteroenteroanastomosis (small intestine into small intestine).
If duodenal cancer is detected, duodenectomy is performed, sometimes with distal gastrectomy or pancreatic resection. In case of advanced small intestinal cancer, where radical resection is not possible, a bypass anastomosis is performed between unaffected loops of intestine. The surgical stage of treatment of small intestine cancer is supplemented with chemotherapy. The same method in some cases is the only way to treat inoperable malignant tumors.
The long-term prognosis for small intestine cancer is determined by the stage of the cancer process and the histological structure of the tumor. In the presence of localized tumor processes without regional and distant metastases, the five-year survival rate after radical resection is 35-40%.
How to check the small intestine for a tumor? Call the Yusupov Hospital and doctors will conduct a comprehensive examination. Once the diagnosis is confirmed, multidisciplinary treatment will be selected for you. When small intestinal cancer is detected in the early stages during a screening examination, when there are no symptoms of the disease, oncologists have the opportunity to perform radical surgery. After it, the prognosis improves.