What are hemorrhoids?
The word “hemorrhoids” translated from Greek means “bleeding,” which is directly related to the main symptom of the disease – the discharge of blood from the anus. It is believed that 8 out of 10 people experience hemorrhoids in one form or another during their lives, which means few of us are immune from this scourge.
According to medical statistics, hemorrhoids most often affect men aged 30 to 50 years. 10% of the world's population consults doctors about this disease, and in developed countries hemorrhoids are found in 60% of citizens.
It would seem that all more or less educated people should have an idea about such a common disease and immediately consult a doctor at the first symptoms. Unfortunately, in life everything is different, and the reason is that hemorrhoids have long been recognized as an indecent disease. It is a shame to talk about it, and the unfortunate are sent to see a specialist only when they can no longer endure it. The most important rule of military science says: “You need to know the enemy by sight.” By shyly keeping silent about the problem of hemorrhoids, we only harm ourselves. But this disease is not much worse than gastritis, unless, of course, it is neglected.
Complications after hemorrhoids: postoperative period
Treatment of hemorrhoids is carried out using several methods depending on the stage of development of the disease. Acute hemorrhoids are treated by a proctologist using conservative treatment - phlebotropic drugs, ointments, gels, suppositories for hemorrhoids. The chronic form of hemorrhoids, accompanied by bleeding, is treated using minimally invasive techniques; the disease at a late stage is treated with surgery. At the Yusupov Hospital, all measures are taken to ensure that there is no relapse of the disease in the postoperative period. The main requirement for the patient is lifestyle correction.
Postoperative complications most often occur in older people and patients who do not follow doctor's recommendations. In 5% of elderly patients in the study group, complications developed after surgery:
- 3% of patients experience acute urinary retention (ischuria).
- 1% of elderly patients - bleeding develops.
- Less than 1% – vascular thrombosis, suppuration develops, and severe pain occurs.
Older patients undergo careful preparation for surgery and a full examination, which minimizes the risk of complications. At the Yusupov Hospital, patients are given a set of exercises involving the muscles of the buttocks, abdominals, anal sphincter, and a diet that regulates the consistency of intestinal contents and prevents the development of constipation. Hemorrhoids are often accompanied by other diseases, including cancer. In the hospital, patients will be able to receive not only effective care from a proctologist, but also undergo examinations by multidisciplinary doctors. You can make an appointment with a doctor by calling the hospital.
Symptoms of hemorrhoids
So, the first thing a person who has been struck by this disease may feel is discomfort. Discomfort, itching and a feeling of wetness and fullness in the anus. Typically, such signs are directly related to visiting the toilet. Here anyone can panic: what is happening to me? But there is no one to consult with, you won’t discuss the problem with friends and colleagues, and you don’t really want to go to the doctor.
After months and sometimes years, symptoms become even more severe. Discomfort and pain begin to bother you when walking, when sitting in one place for a long time, and going to the toilet simply turns into torture. In addition to all the already known troubles, a person is horrified to discover the release of scarlet blood (it’s clear where it comes from). It would seem that now you urgently need to run to the doctor. But only a small part of patients with hemorrhoids do this. And for the rest, the disease continues to progress.
Thrombosis of hemorrhoids
Thrombosed hemorrhoids are more common than other complications and make themselves known by pain that is not associated with bowel movements and in some cases can completely deprive a person of any activity. Thrombosis is often accompanied by local inflammation, which sometimes becomes widespread. The cause of the formation of a blood clot is a violation of blood circulation in the cavernous bodies, due to congestion associated with physical inactivity, pregnancy, diet disorders and other factors. The prognosis of thrombosed hemorrhoids is questionable. In most cases, after a few days, the thrombosed node is replaced by connective tissue, but a more severe outcome is also possible, associated with necrosis, that is, death of the node and involvement of surrounding tissues in the purulent-necrotic process.
How do hemorrhoids develop?
After about five years, the next stage of the disease begins. When a person pushes, hemorrhoids protrude from the anus. At first they are reduced independently, then this can be done with one’s own hand, but in the later stages of hemorrhoids, reduction becomes impossible. A completely logical continuation of an advanced disease. This is where the unfortunate people finally decide to seek medical help, there is nothing to lose, it can’t get any worse. Will. Hemorrhoids still have complications. Heavy bleeding may occur, and then patients develop anemia, and with it weakness, lethargy, dizziness, etc.
How is the rectum structured?
Modern scientists give hemorrhoids the following definition: “hemorrhoids are varicose dilation of the hemorrhoidal veins of the rectum, accompanied by bleeding, and sometimes thrombosis and inflammation, itching and other symptoms.” To understand the mechanism of this disease, you do not need to get into the anatomical jungle. The rectum, like all our organs, must be well supplied with blood. For this purpose, vessels are located in its walls: arteries, veins, capillaries. Unfortunately, for some unknown reason, nature gave us special veins of the rectum, which are scientifically called hemorrhoidal. In structure, they resemble the veins of the penis, that is, they are capable of strong stretching when filled with blood.
In case of blood flow disturbances, namely with increased blood flow to the pelvic organs, including the intestines, and deterioration of outflow, a situation occurs that resembles a school problem about a swimming pool. Water flows in from one pipe and flows out through another. The first one burst, and the second one became clogged. What will happen in the pool? That's right, a flood.
What happens to the hemorrhoidal veins of the intestine?
The hemorrhoidal veins of the intestine turn out to be an unfortunate swimming pool, only they can stretch. Prolonged stress leads to their irreversible expansion, the walls of the veins become thinner, arterial blood stagnates, and as a result, so-called hemorrhoids are formed. Modified and filled to capacity with blood, the veins begin to put pressure on the tissues covering the intestines from the inside. Those, in turn, also stretch, and tears and cracks appear on them. It becomes more and more difficult for them to keep hemorrhoids in the wall of the rectum. Fecal masses systematically move through the wounded intestines, further injuring it, causing bleeding and inflammation. In the last stages of the disease, the nodes protrude from the walls of the rectum, and when the intestinal muscles are tense, they can slide down and even protrude outward.
What causes hemorrhoids?
However, even if we did not inherit the disease from our parents, there are a number of factors that can provoke it.
Profession
This is, first of all, stagnation of blood in the pelvis due to a sedentary lifestyle. It is not for nothing that hemorrhoids are an occupational disease of motorists, programmers, accountants, secretaries and bosses. Bicyclists, motorcyclists and horse riders can also suffer from hemorrhoids. Anyone who spends all day on their feet is also a candidate for the disease; atmospheric pressure overloads the veins. People engaged in heavy physical labor are also not immune from the disease. For example, loaders and athletes, especially weightlifters.
Physical exercise
Excessive effort leads to increased intra-abdominal pressure and, accordingly, impaired blood flow. The situation is almost hopeless. It seems that only lying down work can protect a person from hemorrhoids. However, a reasonable alternation of exercise and gymnastics can, if not completely eliminate the disease, then at least significantly mitigate its symptoms.
Poor nutrition
Nutrition plays a big role in the development of hemorrhoids. Fans of hot and spicy foods, coffee, tea and alcohol should be prepared for unexpected problems in the rectum. The above products increase blood flow where it is least needed. Digestive disorders, especially frequent constipation and diarrhea, are the eternal companions of hemorrhoids. Sitting on the toilet for too long and straining during constipation are especially dangerous.
Stress
The next risk factor is stress; in emotionally unbalanced people it leads to prolonged spasms of the smooth muscles of the walls of blood vessels that drain blood from hemorrhoids. Liver and intestinal diseases, obesity and abuse of sex, including anal sex, increase the likelihood of getting hemorrhoids. But in women, the main cause of hemorrhoids is pregnancy and childbirth, an extreme load on the veins of the rectum.
Causes
The root cause of hemorrhoids is a violation of the inflow and outflow of blood in the cavernous bodies of the rectum. Normally, the corpora cavernosa (also called cavernous bodies) help control the urge to defecate: when filled with blood, they “swell” and help retain feces in the intestines, and after a successful bowel movement, blood flows out and the corpora cavernosa shrink.
If the inflow/outflow regulation is disrupted and the corpora cavernosa have been engorged with blood for a long time, this causes the vascular walls to dilate and thin, making them much more susceptible to rupture or erosive lesions, which in turn cause inflammation and can lead to blood clots.
Factors that provoke venous stagnation
The following predisposing factors can provoke long-term venous congestion in the corpora cavernosa:
- Physical inactivity.
A low level of physical activity (due to sedentary work or simple laziness) causes extensive disturbances of venous blood flow throughout the body - and in the rectum in particular.
- High loads.
Ultra-high physical activity associated with lifting weights causes excessive tension in the abdominal muscles and rectal area, which also leads to disturbances in the venous blood flow.
- Chronic constipation.
The presence of feces in the rectum causes a constant, permanent filling of the cavernous bodies with blood, as mentioned above.
- Venous pathologies.
Impaired blood flow in hemorrhoidal veins can be caused by various vascular diseases.
- Oncology.
Tumor formations in the rectum cause disturbances in the inflow/outflow of blood due to mechanical compression of the venous vessels or their deformation due to tumor growth (in later stages).
- Diarrhea.
Severe diarrhea, especially caused by poisoning or infectious diseases, causes congestion of the venous system of the rectum, which leads to dilation of blood vessels or even micro-ruptures, followed by an inflammatory process.
- Pregnancy and childbirth.
Bearing and giving birth to a child is often accompanied by multiple disturbances in the pelvic venous circulation system, which can (but not necessarily) lead to the appearance of hemorrhoids.
- Obesity.
The presence of excess weight, by analogy with physical inactivity, also leads to multiple disturbances of venous blood flow.
- Bad habits.
Chronic alcohol abuse or long-term tobacco smoking provokes varicose veins, which primarily affects the pelvic region and lower extremities.
- Heredity.
Low hereditary elasticity of the venous vessels of the rectal area creates a predisposition to hemorrhoidal disorders - although it is not considered as their direct cause.
History of hemorrhoid research
Hemorrhoids, like many other diseases, have bothered people at all times. Even 4 thousand years ago in Ancient Egypt and Babylon they already had an idea about it and even tried to treat it surgically, apparently by cutting off prolapsed hemorrhoids. Mentions of the symptoms of hemorrhoids are found in the works of Hippocrates, Galen and Avicenna. These great men quite correctly noted the connection of the disease with constipation, consumption of spicy food and alcohol.
Chinese healers went even further; they identified 24 types of hemorrhoids based on size, shape and location. The first scientific definition of hemorrhoids was given only in the 18th century, when pathologists discovered cavernous-like plexuses in the terminal part of the rectum not only in patients with hemorrhoids, but also in healthy people. However, doctors began to study the mechanisms of hemorrhoids only a century later.
Russian surgeons Nikolai Vasilyevich Sklifosovsky, Arseny Viktorovich Starkov, Pyotr Aleksandrovich Butkovsky made a great contribution to this research at the end of the 19th and beginning of the 20th centuries. Until the beginning of the 20th century, hemorrhoids were treated the old fashioned way. Lotions of nettle, rhubarb and cucumber were prescribed. Leeches were also applied to hemorrhoids so that they would suck out excess blood and thereby reduce the size of the nodes. It was also practiced to send patients under the knife, but the results of such treatment were not always satisfactory. Surgeries to remove hemorrhoids were extremely painful and bloody.
Only by the 1930s did the optimal technique for hemorrhoidectomy finally emerge. With some changes, it has survived to this day. Based on the names of the surgeons who created it, the operation is called Morgan-Milligan hemorrhoidectomy. In developed countries today it is performed in 17-21% of patients, usually with complicated hemorrhoids. In Russia, this operation is performed much more often - it is prescribed for 75% of patients.
Classification of hemorrhoids
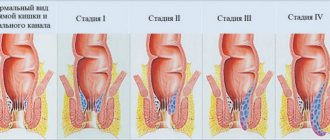
Over the past few decades, new trends have emerged in the treatment of hemorrhoids. Firstly, the classification of the disease has finally been established. Now hemorrhoids are divided into acute and chronic, and for chronic hemorrhoids there are four stages. The disease in the acute phase is characterized by transience and complications in the form of thrombosis, strangulation of hemorrhoids, etc.
Chronic hemorrhoids last for years, they are less painful, so patients see a doctor only in the last stages, when the veins can no longer be straightened. And, secondly, new methods of combating hemorrhoids have appeared, which are used in accordance with the stage of the disease.
In acute hemorrhoids and in the early stages of chronic hemorrhoids, conservative treatment is carried out. Its main goal is to relieve pain and inflammation, normalize blood circulation in the rectal area, and regulate digestion. Conservative treatment is common: tablets that increase the tone of the veins, improve blood flow through small vessels and hemorrhoidal veins; and local: wound healing, analgesic and antipruritic ointments, suppositories, microenemas and baths. At the same time, an anti-hemorrhoids diet is prescribed: vegetables, fruits, bran, but you will have to forget about spices, spicy foods and alcohol.
Classification features of pathology
Experts identify several options for dividing the disease. The clinical picture made it possible to separate the process:
- for an acute course - with severe symptoms;
- chronic - with periods of exacerbation and remission.
Proctologists attribute both conditions to phases of a single process - hemorrhoids. The acute phase is classified as complications of chronic pathology; it is further divided into three degrees of complexity:
- in the first case, thrombosis is observed (the formation of blood clots that prevent the free flow of blood through the veins) of external and internal hemorrhoids without the addition of inflammation;
- second – the pathology is complicated by an active inflammatory process;
- third - thrombosis becomes widespread, provokes inflammation in the subcutaneous tissue, swelling of the dermis near the anus, necrosis of the mucous membrane of the hemorrhoid.
The secondary classification divides the pathological process into three types, depending on the location of the hemorrhoid. The list is presented:
- internal – with the location of pathological foci under the rectal mucosa;
- external – with localization under the skin;
- combined - including the characteristics of the two previous types.
As the pathological process develops, the disease passes through several stages. They are used by specialists to identify the degree of complexity of the disease. It is customary to distinguish 4 successive stages:
- It is determined by the protrusion of nodes into the intestinal lumen, without prolapse. The act of defecation is accompanied by bleeding from the anus.
- There is a loss of hemorrhoidal cones during the emptying of the intestines. They return to their original position on their own.
- The nodes fall out with little physical exertion. The patient can adjust them independently, without outside help.
- Formations that fall outside the rectum cannot be reduced and require professional help.
The stage is determined using laboratory diagnostic procedures, which determine the necessary therapy.
How are hemorrhoids treated?
Minimally invasive (or low-traumatic) treatment methods are prescribed for chronic hemorrhoids at stages I, II or III, as well as against the background of improved health in acute hemorrhoids. There are many such methods. The doctor chooses which one is best for the patient individually.
All methods involve the non-surgical removal of hemorrhoids or their fixation in the wall of the rectum.
Infrared coagulation
Most popular in the West. The nodes are removed by applying high temperature to them, which is created by infrared rays. This is the fastest, painless and effective method of treating hemorrhoids. After the intervention, patients can begin work on the same day or the next day.
Ligation of nodes with latex rings
The second most popular procedure. The hemorrhoidal node at the base is tied with rubber (latex), as a result it is left without nutrition and soon dies. Final release occurs approximately 3 weeks after medical manipulation. The procedure itself is painless, but the death of the node can cause pain.
Sclerotherapy
Requires special professionalism of the doctor. A substance is injected into the cavity of the node with a thin needle, which will lead to the formation of connective tissue in the hemorrhoidal node, as a result of which the nodes become smaller.
Cryotherapy
The node is removed with liquid nitrogen under local anesthesia. It is difficult to control the depth of exposure, so patients are not immune from postoperative complications.
Laser therapy
Secures the hemorrhoid in the wall of the colon using a laser. An effective, albeit expensive procedure. Unfortunately, complications in the form of bleeding are often observed.
Electrocoagulation: mono- and bipolar
Getting rid of hemorrhoids using current. It is preferable to carry out bipolar, it is less painful and has almost no complications.
Full operation
The third treatment option for hemorrhoids is a full-fledged operation. The same one when hemorrhoids are excised and their vascular pedicles are ligated. It is performed under general anesthesia at any stage of the disease. After surgery, the patient spends almost a week in the hospital, swallowing analgesics. But after discharge, he may forget about hemorrhoids forever.
Ingenious operation
In 1993, Italian surgeon Antonio Longo came up with a completely new and ingenious operation to combat hemorrhoids. Unlike other surgeons, he did not remove hemorrhoids, but part of the stretched mucous membrane that lines the inside of the rectum and covers the nodes. As a result of the operation, the mucous membrane pressed the hemorrhoids to the intestinal walls, while the blood flow to them decreased. This operation takes 10-15 minutes. Patients spend 2-3 days in the hospital, and after 3-5 days they forget about the operation and the annoying hemorrhoids. The only disadvantage of the technique is its novelty. No one knows yet what the long-term consequences of the operation may be. So now we can say with confidence that hemorrhoids are curable, the main thing is not to let them get worse.
According to historians, Emperor Napoleon suffered from an acute attack of hemorrhoids before the Battle of Waterloo. The illness of the famous commander was one of the reasons why the battle was lost. But if Napoleon had been able to use the services of proctologists of the 21st century, it is possible that history would have taken a completely different path.
Natalia Klim, Paradox Magazine (Rodionov Publishing House)
How to deal with the disease at different stages
The expansion of hemorrhoidal veins requires an immediate response already at the initial stage of its development. In this case, it is necessary to clearly establish why hemorrhoids occurred in a particular situation, and try to reduce the negative influence of factors to a minimum. In addition, it is important to begin eliminating the consequences of changes as early as possible in accordance with the stage of the disease:
- At the first stage of hemorrhoids, drug treatment with topical drugs with anti-inflammatory, regenerating, analgesic and venotonic effects is recommended. Sclerosis of hemorrhoidal veins can also be used. Patients are also advised to follow a diet and increase physical activity.
- The second stage of hemorrhoids involves the same treatment as in the first stage, but with the use of oral medications (local ones are also included in the treatment regimen). In addition, radical methods for eliminating hemorrhoids are used: sclerotherapy, ligation, laser removal of nodes, cryotherapy or coagulation of nodes.
- The third stage of hemorrhoids requires more radical measures, and therefore conservative therapy gives way to surgical treatment - hemorrhoidectomy and vein disarterization and the use of various technologies (laser, radio waves). Latex ligation of nodes is also used at this stage.
- The fourth stage of hemorrhoids is complicated by complete prolapse of the nodes and a high probability of thrombosis and heavy bleeding. Effective methods of treating hemorrhoids at this stage are laser coagulation and hemorrhoidectomy (laser or radio wave). For vein thrombosis, thrombectomy is performed. Conservative therapy for this degree of disease is ineffective.
Regardless of what stage of hemorrhoids occurs, in parallel with the methods described above, it is necessary to apply preventive measures. They are most often aimed at eliminating the causes of hemorrhoids. This allows you to lengthen the relapse-free period and avoid further progression of the disease.
Sources
- Khivantsev K., Jaegers NR., Kwak JH., Szanyi J., Kovarik L. Precise identification and characterization of catalytically active sites on the surface of γ-alumina. // Angew Chem Int Ed Engl - 2021 - Vol - NNULL - p.; PMID:33904227
- Nayar G., Seabolt EE., Kunitomi M., Agarwal A., Beck KL., Mukherjee V., Kaufman JH. Analysis and forecasting of global real time RT-PCR primers and probes for SARS-CoV-2. // Sci Rep - 2022 - Vol11 - N1 - p.8988; PMID:33903676
- Zhang YF., Luo HN., Shi R., Zhang YJ., Tai XM., Hu XY., Ma JF., Wang XY., Zhang YS., Qu PP. . // Zhonghua Fu Chan Ke Za Zhi - 2021 - Vol56 - N4 - p.257-263; PMID:33902237
- Quinn MH., Bauer AM., Fox EN., Hatzell J., Randle T., Purnell J., Rogers T., Stevens N., Leone F., Achenbach C., Wileyto EP., Josephson S., Gollan J ., Asare R., Hitsman B., Schnoll R., Gross R. Rationale and design of a randomized factorial clinical trial of pharmacogenetic and adherence optimization strategies to promote tobacco cessation among persons with HIV. // Contemp Clin Trials - 2021 - Vol - NNULL - p.106410; PMID:33901574
- Mulholland MM., Sherwood CC., Schapiro SJ., Raghanti MA., Hopkins WD. Age- and cognition-related differences in the gray matter volume of the chimpanzee brain (Pan troglodytes): A voxel-based morphometry and conjunction analysis. // Am J Primatol - 2022 - Vol - NNULL - p.e23264; PMID:33899958
- Boeri J., Meunier C., Le Corronc H., Branchereau P., Timofeeva Y., Lejeune FX., Mouffle C., Arulkandarajah H., Mangin JM., Legendre P., Czarnecki A. Two opposite voltage-dependent currents control the unusual early development pattern of embryonic Renshaw cell electrical activity. // Elife - 2022 - Vol10 - NNULL - p.; PMID:33899737
- Ke L., Wu QYS., Zhang N., Yang Z., Teo EPW., Mehta JS., Liu YC. Terahertz spectroscopy analysis of human corneal sublayers. // J Biomed Opt - 2022 - Vol26 - N4 - p.; PMID:33899380
- Wang K., Chen Y., Ahn S., Zheng M., Landoni E., Dotti G., Savoldo B., Han Z. GD2-specific CAR T cells encapsulated in an injectable hydrogel control retinoblastoma and preserve vision. // Nat Cancer - 2022 - Vol1 - N10 - p.990-997; PMID:33898999
- Oh S., Tsujimoto T., Kim B., Uchida F., Suzuki H., Iizumi S., Isobe T., Sakae T., Tanaka K., Shoda J. Weight-loss-independent benefits of exercise on liver steatosis and stiffness in Japanese men with NAFLD. // JHEP Rep - 2022 - Vol3 - N3 - p.100253; PMID:33898958
- Castor-Praga C., Lopez-Walle JM., Sanchez-Lopez J. Multilevel Evaluation of Rapid Weight Loss in Wrestling and Taekwondo. // Front Sociol - 2022 - Vol6 - NNULL - p.637671; PMID:33898554