For the city of ancient Crete, see Pylorus (Crete).
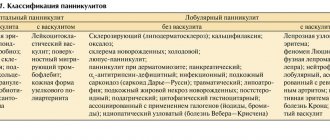
| Gatekeeper | |
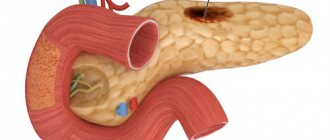
| Inside the stomach (pylorus labeled center left) | |
| Details | |
| Identifiers | |
| Latin | Gatekeeper |
| MeSH | D011708 |
| TA98 | A05.5.01.017 |
| TA2 | 2930 |
| F.M.A. | 14581 |
| Anatomical terminology [edit in Wikidata] | |
To the gatekeeper
(/paɪˈlɔːrəs/ or /pɪˈloʊpəs/), or
pyloric part
, connects the stomach to the duodenum.
The pylorus is believed to consist of two parts: the pyloric antrum
(opens to the body of the stomach) and
the pyloric canal
(opens to the duodenum).
The pyloric canal
ends as
the pyloric orifice
, which marks the connection between the stomach and duodenum.
The opening is surrounded by the sphincter, a group of muscles called the pyloric sphincter
.
The word pylorus
comes from the Greek πυλωρός, via Latin.
The word gatekeeper
in Greek means "gatekeeper", refers to a "gate" (Greek: Pyle) and is thus linguistically related to the word "pylon".[1]
Structure
Diagram from Cance.gov:
* 1. Body of the stomach * 2. Fundus * 3. Anterior wall * 4. Greater curvature * 5. Lesser curvature * 6. Cardia * 9. Pyloric sphincter * 10. Pyloric antrum * 11. Pyloric channel. * 12. Corner cut * 13. Gastric canal * 14. Rugal folds
The pylorus is the outermost part of the stomach that connects to the duodenum. It is divided into two parts: antrum
, which connects to the body of the stomach, and
the pyloric canal
, which connects to the duodenum.[2]
Antrum
Into the pyloric antrum
this is the initial part of the gatekeeper. It is located in the lower part of the stomach, proximal to the pyloric sphincter, which separates the stomach and duodenum. It may be temporarily partially or completely disconnected from the rest of the stomach during digestion by peristaltic contraction of the prepyloric sphincter; it is sometimes delimited from the pyloric canal by a small groove.
Channel
Into the channel
(Latin: canalis pyloricus) is the opening between the stomach and duodenum.[3] The thickness of the wall of the pyloric canal is up to 3 millimeters (mm) in children younger than 30 days.[4] and up to 8 mm in adults.[5]
Sphincter
In the pyloric sphincter
The valve, or valve, is a strong ring of smooth muscle at the end of the pyloric canal that allows food to pass from the stomach into the duodenum. It controls the flow of gastric contents into the duodenum.[6] It receives sympathetic innervation from the gluten ganglion.
Histology
Microscopic section of the pylorus.
Under microscopy, the pylorus contains numerous glands, including the gastric pits, which comprise approximately half the depth of the pyloric mucosa. They consist of two or three short, closed tubes opening into a common duct or orifice. These tubes have a wavy shape and make up approximately half the length of the duct. The air duct is lined with columnar cells, continues with the epithelium lining the surface of the gastric mucosa - tubes with shorter and cubic cells, fine-grained. The glands contain mucus cells and G cells that secrete gastrin.[7]
The pylorus also contains scattered parietal cells and neuroendocrine cells. These are endocrine cells, including D cells, that release somatostatin.[8] (Somatostatin is responsible for turning off acid secretion. There is a second hormone-sensitive population near the fundus of the eye. Smooth muscles, which are completely involuntary, are located at the pylorus.
Main reasons
It is believed that the disease can be caused by any factors affecting the regulatory processes of the central nervous system, spinal cord, and local gastric network. In other words, any damage to the nervous system can provoke gastric atony.
Signs of atrophic gastritis of the stomach
The triggering factor may be:
- severe infectious diseases with severe intoxication (especially typical for typhoid fever, botulism);
- excessive stressful situations;
- previous myocardial infarction, peritonitis, lobar pneumonia;
- spinal and brain injury.
Gastric atony is detected in patients against the background of:
- frequent excessive overeating (overstretching of the stomach walls);
- exposure to toxic substances (toxins) due to food poisoning;
- exhaustion of the body;
- thrombosis of the feeding arterial vessels of the stomach;
- endocrine pathology, hormonal imbalance;
- damage to nerve trunks during gastric surgery;
- congenital changes in the form of prolapse and lengthening of the organ.
Clinical significance
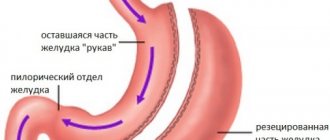
In conditions such as stomach cancer, tumors can partially block the pyloric duct. A special tube may be surgically implanted to connect the stomach to the duodenum to facilitate the passage of food from one to the other. The operation to install this tube is called gastroduodenoanastomosis.
Stenosis
Main article: Pyloric stenosis
Pyloric stenosis refers to a narrow pylorus. This is due to congenital hypertrophy of the pyloric sphincter. The pyloric lumen is narrower and less food passes through it. This problem is often discovered in the first weeks of life. When present, the newborn baby may vomit after eating but remain hungry despite vomiting. Pyloric stenosis can be treated by insertion of a stent or by surgical division of the pyloric sphincter and pyloromyotomy
.[9]
Another
- Tumors of the pyloric region Adenoma of the pyloric gland[10]
Course of the disease
Stomach atony is accompanied by severe pain
Gastric atony is characterized by the appearance of pain in the epigastric region, nausea and belching of air or food. Many patients complain of deterioration in health as a result of eating. Atony causes an increase in intra-abdominal pressure in patients and a feeling of fullness in the gastric zone. Against this background, severe pain in the abdominal area may appear. Gastric atony is accompanied by a feeling of heartburn, as well as the appearance of a specific odor from the oral cavity. In some cases, patients experience vomiting containing a certain amount of green liquid.
Patients experience a feeling of rapid satiety while eating. Externally, patients with gastric atony are quite pale and complain of cold sweat. Many of them experience attacks of tachycardia or arterial hypotension. Based on the manifestation of these symptoms of the disease, it is quite difficult to give the patient an accurate diagnosis of the existing disease.
Recommendations
- Harper, Douglas. "Gatekeeper". Etymology online
. Retrieved March 27, 2014. - Drake, Richard L.; Fogle, Wayne; Tibbits, Adam W. Mitchell; illustrations by Richard; Richardson, Paul (2005). Gray's Anatomy for Students
. Philadelphia: Elsevier/Churchill Livingston. p. 272. ISBN 978-0-8089-2306-0. - University of Illinois Medical Center: Health Library Archived 2012-04-26 at the Wayback Machine
- Rohrschneider, W.K.; Mittnacht, H; Darge, K; Traeger, J (June 1998). "The pyloric muscle in asymptomatic infants: sonographic evaluation and definition of idiopathic hypertrophic pyloric stenosis." Pediatric Radiology
.
28
(6): 429–34. Doi:10.1007/s002470050377. PMID 9634457. - Lin, Hsien-Ping; Lin Yu-Chan; Kuo, Chen-Yun (2015). "Idiopathic hypertrophic pyloric stenosis in adults." Journal of the Formosan Medical Association
.
114
(7):659–662. doi:10.1016/j.jfma.2012.07.001. ISSN 0929-6646. PMID 26154756. - Snell, Richard S. (2008). Clinical anatomy by region
. Lippincott Williams and Wilkins. p. 220. ISBN 978-0781764049. - Cardiac, ocular and pyloric regions of the stomach, pyloric region. Available from: https://histology.leeds.ac.uk/digestive/cardiac_pyloric.php (Last accessed 16 April 2022)
- Deakin, Barbara Young; and others. (2006). Wither's Functional Histology: Text and Color Atlas
(5th ed.). Churchill Livingston / Elsevier. p. 273. ISBN 978-0-443-068-508. - Clayden, Tom Lissauer, Graham (2007). Illustrated textbook of pediatrics
(3rd ed.). Edinburgh; New York: Mosby/Elsevier. pp. 207–208. ISBN 9780723433972. - Chen, Z.M. Scudiere, J. R.; Abraham, SC; Montgomery, E (2009). "Pyloric gland adenoma: an entity distinct from gastric foveal adenoma." Am J Surg Pathol
.
33
(2): 186–193. Doi:10.1097/PAS.0b013e31817d7ff4. PMID 18830123.
Diagnostics
Hardware methods help to identify gastric atony, but to determine the cause and prescribe optimal treatment, the attending physician will definitely prescribe a comprehensive examination.
An important point is that it is difficult for the patient to prepare for research. Even with special fasting, it is difficult to achieve a state of complete emptying of the stomach and intestines. Therefore, vomit is often released during fibrogastroscopy. After cleansing, the doctor sees a distended stomach with no signs of inflammation or congestion with irritation of the mucous membrane.
An X-ray examination with contrast material (barium suspension) can detect an enlarged stomach cavity, an elongated shape, a “fall” and accumulation of barium in the pylorus area. Images are taken in different projections in order to exclude as accurately as possible a mechanical obstacle in the form of a tumor.
Treatment requirements
Treatment for gastric atony requires an integrated approach. Through questioning and examination, it is often possible to find out the underlying causes. To eliminate them, you will need to change your lifestyle, habits, special physical exercises, diet, and follow the recommendations of specialists: gastroenterologist, therapist, neurologist, psychiatrist.
Surgical treatment is practically not used. It is not difficult to assist the patient by lavaging the stomach with a probe. The problem is to normalize the natural path of digestion and support other organs and systems.
The treatment regimen is selected for each patient individually
Diet
The patient is assigned to table No. 2 according to Pevzner. It includes mandatory compliance with the following conditions:
- frequent meals (7–10 times a day) in small portions;
- excluding everything fried, spicy, smoked and switching only to cooked dishes;
- preference for liquid and semi-liquid foods;
- getting used to drinking drinks in small sips;
- the need for breaks between eating solid and liquid foods;
- exclusion of dishes with contrasting temperatures.
With all restrictions, the patient must receive sufficient amounts of vitamins and protein. To stimulate peristalsis, the following are indicated: rye bread, fermented milk products, prunes, honey. Protein is compensated by dishes made from lean boiled meat, chicken, fish, buckwheat porridge, oatmeal, and milk soups. You can include eggs in your diet.
Physiotherapy
Physical exercises are aimed at strengthening the abdominal muscles. In this way, restoration of lost innervation of the stomach is achieved. Increased muscle tone is promoted by:
- “bicycles” with legs lowered as low as possible to the floor;
- lifting the legs in a lying position to an angle of 90 degrees and slowly lowering them;
- throwing your legs behind your head;
- performing a “birch” on the shoulder blades;
- static standing in a hand plank for a minute;
- swing your legs forward, backward and to the sides;
- twisting the spine forward with the legs pressed to the floor.
Patients are advised to consult a specialist about therapeutic exercises and perform them daily. At the same time, they advise you to master a course of breathing exercises, swim in the pool, and walk more. After classes in the morning, a contrast shower is shown. It helps strengthen the nervous system.
If the main damaging factor is stress, then you need to do yoga, relaxation exercises, and auto-training.
Classes in groups are considered the most effective
For mild atony, the use of a gastric band has a good effect. It is worn in a lying position. Wear it all day. Dense tissue supports the abdominal wall and increases muscle tone. To purchase, you need to know your size and consult your doctor.
Treatment with medications
For gastric atony, the following medications are used:
- improving gastric motility (Motilium, Proserin);
- stimulating the process of restoration of impaired innervation (Solcoseryl);
- vitamins - especially group B, are necessary to ensure nervous regulation;
- antiemetics;
- containing calcium and potassium necessary for muscle fibers.
Patients with general asthenia and sudden weight loss are prescribed anabolic hormones, immunomodulators, and protein solutions are administered intravenously. Some experts advocate a course of subcutaneous insulin treatment. In any case, therapy requires an individual approach. You cannot choose treatment on your own.
Traditional methods
Folk advice helps strengthen gastric peristalsis. Decoctions of the following plants are suitable for this: chamomile, dandelion root, rose hips, oregano, coltsfoot leaves, yarrow.
You need to brew them like tea and drink them half an hour before meals.
If left untreated, the most common complications of gastric atony are gastritis with possible progression to peptic ulcer, acute gastric rupture, and intestinal atony. It should be remembered that any congestion causes the risk of developing tumors.
Prognosis and prevention
If the pathology is under the control of a doctor and the patient is aware of his problem, then one has to make efforts and gradually cope with it, achieving stable periods of remission.
But with a person’s connivance and unwillingness to follow the doctor’s advice and follow the regimen, the disease progresses and causes complications.
Prevention consists of constantly complying with diet requirements, physical exercise, courses of therapy, taking vitamins, and changing your attitude towards stressful situations. Human inaction only worsens the prognosis and contributes to the accumulation of various diseases.