The cardia, or cardiac part of the stomach, is a cylindrical segment covering the esophagogastric junction and the space 2 cm above and below it. Cancer of the gastric cardia (cardioesophageal cancer, CER) differs in anatomical and clinical features, and requires a special approach to treatment. Many experts even identify it as a separate nosology, and there are several reasons for this:
- Tumors of this location tend to spread to the esophagus much more often than cancer of the underlying parts of the stomach.
- Such tumors metastasize to the abdominal and mediastinal lymph nodes.
- In addition, they have a poorer prognosis than gastric or esophageal cancer.
Cardioesophageal cancer is characterized by aggressive growth and a tendency to metastasize to the mediastinal lymph nodes.
- Causes
- Symptoms of gastric cardia cancer
- Classification
- Diagnostics
- Treatment of gastric cardia cancer
- Complications and relapses
- Prognosis and prevention
Causes
The causes of cardiac cancer are not reliably known. Currently, it is customary to talk about risk factors - circumstances under which the likelihood of developing a particular pathology increases. For stomach cancer they are as follows:
- Helicobacter pylori infection.
- The presence of atrophic gastritis of the proximal stomach.
- Hereditary predisposition.
- Smoking and alcohol abuse.
As for gastroesophageal reflux and Barrett's esophagus, these conditions are the main predisposing factors for the development of esophageal cancer, but they do not affect the incidence of cardia cancer.
Symptoms of gastric cardia cancer
Cardia cancer is most characterized by weight loss, food aversion, pain and dysphagia. The pain is usually localized in the epigastric region, is constant, pressing in nature and does not depend on food intake. Sometimes it radiates to the lumbar region or behind the sternum. In the latter case, the disease can simulate heart pathology, such as angina.
The severity of dysphagia depends on the size of the tumor and obstruction of the digestive tract. It is mainly manifested by malnutrition, which leads to hypovolemia and changes in electrolyte balance.
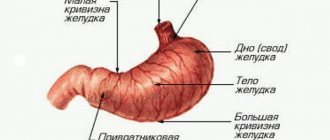
Lots of food - big belly!
The size of the stomach changes when food enters it.
When food enters the stomach, its size increases and the walls stretch. After the stomach has completed its function of processing food, it returns to its form. An empty stomach constantly moves, and at this time a person experiences a feeling of hunger. The shape of the stomach depends on the height and size of the person.
For example, in short and overweight people, the shape of the stomach resembles a horn. In tall and slender people, the shape of the stomach can be compared to a stocking. In people of standard build, the stomach is shaped like a hook. The size of the stomach can be easily adjusted. It depends on the amount of food a person consumes at one time. The walls of the stomach stretch and more and more food will be needed each time to become full (feeling of a full stomach). This can lead to an increase in the size of the stomach.
Healthy stomach size
The size of an adult's stomach when empty is no more than 500 ml; when full it can reach four liters. The average length of a healthy stomach is 25 cm, height is about 13 cm. The distance between the surfaces of the stomach (anterior and posterior) is about 8.5 cm. The distance between the lesser and greater curvature is 11 cm, in an empty stomach - 7.5 cm. In a hungry person The length of the stomach is 19 cm, while its walls touch each other.
Classification
The classification of cardia cancer is based on the location of the center of the tumor. The anatomical reference point is the Z-line - the line of the esophagogastric junction.
- Type I cancer - the center of the tumor is located at a distance of 1-5 cm above the Z-line towards the esophagus.
- Type II cancer - the center of the tumor is located within 1 cm orally and 2 cm below the Z-line.
- Type III cancer - the center of the tumor is located at a distance of 2-5 cm below the Z-line.
Diagnostics
- Endoscopic examination of the stomach and esophagus. Allows you to examine the tumor and take a biopsy for morphological examination.
- Endoscopic ultrasound. It is carried out to determine the degree of tumor invasion, its growth into neighboring organs and structures, as well as to search for regional metastases.
- Abdominal ultrasound. It is carried out to search for metastases.
- X-ray contrast study. Allows you to determine the extent of the tumor and assess the degree of stenosis of the cardia and esophagus. The method is especially relevant for diffuse-infiltrative forms of cancer, when false-negative biopsy results can be obtained due to submucosal localization.
- CT scan is used to look for distant metastases.
- Diagnostic laparoscopy. Allows you to detect the spread of the tumor to the serous membranes, as well as diagnose intraperitoneal dissemination.
- Determination of tumor markers - CEA, CA 19-9, CA 72-4.
Tumor heterogeneity
Most tumors are monoclonal in origin, but at the time of detection they consist of genetically, epigenetically and phenotypically heterogeneous clones. Two main concepts attempt to explain this heterogeneity: the cancer stem cell hypothesis and the clonal (stochastic) evolution model (Fig. 1).
The clonal evolution model assumes that each tumor cell has the ability to initiate tumor formation. Progression is directed by rare stochastic events occurring in all cells. Cells with mutations that confer a growth advantage will predominate over other tumor cells and may form a new clone containing cells of different phenotypes that have different proliferative potential [4–6].
The CSC theory, formulated in 1997 [7], is based on the assertion that in the structure of tumor cell populations there is a clear hierarchy, at the top of which there is a population of transformed cells that have properties similar to normal stem cells. CSCs are called tumor-initiating cells (TIC) or tumor-propagating cells (TPC) [8,9]. According to the concept, the RSC population:
- Makes up a small proportion of the total tumor cell population;
- Expresses a specific set of surface markers;
- Selectively supports the ability for tumorigenesis in contrast to other populations of tumor cells;
- Supports the growth of a heterogeneous mass containing a full complement of partially (or fully) differentiated cancer cells;
- Forms a separate pool of cells, identified by biological and physicochemical methods (at least two pools of cells in the tumor: CSCs and their derivatives - cells differentiated to varying degrees);
- Shows the ability, like normal stem cells, for unlimited self-renewal and differentiation in many directions [9];
- Shows high resistance to standard therapy [2].
Rice. 1 | Models of tumor heterogeneity. A - evolutionary stochastic model; B – hierarchical model of cancer stem cells [5].
Treatment of gastric cardia cancer
Treatment of cardia cancer requires a combined approach and includes chemotherapy and surgery. For unresectable tumors, the main treatment method is chemotherapy, and operations are performed for life-threatening indications.
Surgical treatment
The choice of the extent of the operation and surgical approach is determined based on the type of cancer and its local prevalence. For type I CER, proximal gastrectomy is performed
| KER type I Proximal gastrectomy, subtotal esophageal resection. | KER type II Gastrectomy (the entire stomach is removed), resection of the lower thoracic esophagus | KER type III Gastrectomy, resection of the lower thoracic esophagus. |
The minimum volume of lymph node dissection involves the removal of 1st and 2nd order lymph nodes (extended lymph node dissection is performed in the volume of D2). In CER I, bilateral mediastinal lymph node dissection is performed.
Chemotherapy
Chemotherapy is carried out using one of the following options:
- Perioperative chemotherapy. Performed in CF or ECF mode for 8-9 weeks before and after surgery.
- Adjuvant chemotherapy. It begins 4-6 weeks after surgery, if there are no severe complications, and is carried out for 6 months. XELOX or CAPOX schemes are used.
- Adjuvant chemoradiotherapy. Currently, it is rarely used and only in case of non-radical surgery.
Treatment of unresectable and disseminated tumors is carried out using chemotherapy according to the CF, CX, XELOX regimens in 6-8 three-week courses, or 9-12 two-week courses. After this, treatment is stopped and observation is carried out until the disease progresses. For HER2-positive gastric cancer, treatment with trastuzumab is possible.
After disease progression, chemotherapy is resumed, and the treatment regimen is selected taking into account the existing medical history.
Metastasis
With CER types I and II, metastasis mainly occurs in the lymphatic collectors of the paracardial zone, celiac trunk and lesser curvature of the stomach. In type I CER, the mediastinal nodes may also be involved in the process. Such features of metastasis are taken into account when planning surgery and lymph node dissection.
Preparing for the study
Proper preparation is an important factor in effective research.
The study is carried out strictly on an empty stomach. The last meal should be no later than seven or eight o'clock in the evening.
For 3-4 days before the test, you should follow a diet that excludes foods that cause gas formation - black bread, legumes, carbonated drinks, cabbage, fresh vegetables and fruits, strong coffee, smoked meats, sweets, etc. If there are no individual contraindications, baked, boiled or steamed poultry or lean meats, boiled potatoes, water porridge, rice, and low-fat cheese are best. At the same time, you need to take food 4-5 times a day.
If you have flatulence or constipation, then 3-4 days before the study you need to take espumisan 2 capsules per day before the study (if there are no contraindications).
The day before you need to empty your bowels. You can use a laxative, but not an enema.
Complications and relapses
The main complications of cardioesophageal cancer:
- Tumor disintegration and bleeding. In this case, urgent endoscopic examination and bleeding control are required. If the problem cannot be solved endoscopically, surgical intervention is performed.
- Tumor stenosis. This complication leads to dysphagia and, as a consequence, to the development of nutritional disorders. To eliminate it, recanalization, balloon dilatation, and stenting are used. In severe cases, bypass anastomosis or gastrostomy removal is indicated.
- Pain. To reduce pain, radiation therapy, drug treatment and, in some cases, locoregional anesthesia are used.
- Ascites is an accumulation of fluid in the abdominal cavity. To eliminate it, diuretics and intracavitary chemotherapy are prescribed. When large volumes of fluid accumulate, laparocentesis is indicated - evacuation of the contents through puncture.
Advantages
The study is carried out transabdominally, that is, through the abdominal wall and does not cause any discomfort.
The technique allows you to control the progress of other diagnostic and therapeutic procedures, since the image is constantly broadcast on the screen, in real time.
Ultrasound diagnostics does not create radiation exposure for the patient, and therefore can be performed regardless of age, even for children, pregnant women and during breastfeeding.
Prognosis and prevention
The 5-year survival rate for any type of CER averages 23.6%. Type III tumors have the most unfavorable course, since they are predominantly represented by poorly or undifferentiated neoplasms. The 5-year survival rate for this location is about 14%. The prognosis is significantly worsened by the presence of metastases in the mediastinal lymph nodes.
Euroonko employs doctors with extensive experience in treating stomach cancer. We are guided by current European standards. For this, the clinic has everything necessary - from the latest medications to modern equipment, thanks to which we are ready to provide assistance in the most severe cases.
Book a consultation 24 hours a day
+7+7+78