GastrituNet.ru » Stomach diseases » Structure » Anatomy » Sections of the stomach
Despite the simplicity of the anatomical structure, the stomach has several functional sections. Moving from department to department, the food bolus is ground, after which it enters the duodenum and large intestine. One of these segments is the pyloric section of the stomach, which performs not only a digestive function.
- 1 Features and anatomical characteristics
- 2 Pathologies of the pyloric part of the stomach
- 3 Useful video
- 4 Preventive measures
Features and anatomical characteristics
The pylorus or pylorus is conventionally the lower part of the stomach. From below, the pyloric section is connected to the duodenum by the pyloric sphincter or sphincter - a ring-shaped muscular septum, which is responsible for the entry of the semi-digested food bolus into the sections of the small intestine ahead of time.
In addition, the pyloric sphincter allows the required volume of gastric juice to pass through and separates solid food from semi-liquid food.
In its shape, the pyloric part of the gastric cavity resembles an expanded oval, which tapers towards the duodenum. Anatomy may vary slightly, repeating the individual physiological parameters of the human body. The pyloric section is otherwise called the bottom of the stomach, which is responsible not only for the digestive, but also for a number of other functions:
- accumulation, processing and further transport of the food bolus to the lower parts of the digestive system;
- processing the food bolus with special digestive enzymes (chymosin, lipase, pepsin) and hydrochloric acid;
- production of Castle factor - a special component that absorbs, combines and transports vitamin B12 throughout the body;
- absorption of certain types of salt compounds, glucose and water:
- the production of hormones responsible for the functionality of the entire digestive system.
An important aspect in the functional purpose of the pyloric part of the stomach is the compensatory possibility in case of chronic renal failure or severe intoxication. At the moment of pronounced dysfunction of these organs, the secretion and excretion of special enzymes begins in the pyloric region, responsible for the expulsion of toxins from the blood plasma.
Regulation of the release and distribution of hydrochloric acid contributes to the antibacterial treatment of the food bolus, killing conditionally active pathogenic microflora. In addition to digestive hormones, the pyloric segment of the stomach produces serotonin, gastrin, somatostatin, and endorphins. The pyloric glands are responsible for the endocrine function of the organ and influence metabolic processes in the body.
Note! Interaction with the entire digestive system leads to serious diseases only with minor functional failure of certain systems.
Anatomy
Compared to other parts of the stomach, the size of the pyloric part is small, its length ranges from 4 to 6 cm. It has the shape of a funnel or an expanded oval and tapers downward. Anatomical features may vary slightly depending on the individual physiological parameters of a particular person’s body.
WHERE IS
The pyloric section is located in the lower part of the stomach at the point of its transition to the duodenum (duodenum). In height it is at the level of the 12th thoracic and 1st lumbar vertebrae, displaced towards the vertebral column. It is separated from the body of the stomach on the inner side by a transverse groove, and from the duodenum by the pylorus.
STRUCTURE
The department is divided into two parts:
- cave - a wide part connected to the body of the stomach;
- the channel is a narrower part that connects to the duodenum and is approximately equal in width.
Structure of the stomach
The pyloric region has well-developed muscles, and the closer to the duodenum, the thicker the muscle layer. On the side of the greater curvature of the stomach it is slightly convex, and on the side of the lesser curvature it is concave. Inside, its mucous membrane is covered with folds that form peculiar paths to facilitate the movement of chyme.
Glands
In the lower section there are special glands. Their structure is tubular, the end sections are highly branched and convoluted, flowing into the gastric pits. They consist of cells that protect the mucous membrane from acidic gastric juice.
The pyloric glands produce digestive enzymes and hormones (serotonin, somatostatin, endorphins). The secretion they produce has an alkaline reaction.
Gatekeeper
The pyloric part ends with the pylorus. This is a sphincter, which is a ring-shaped muscle with an average diameter of 1–2 cm. It has a tortuous venous network that provides blood supply. In a relaxed state, the sphincter allows small portions of food digested in the stomach into the duodenum; in a compressed position, it is closed and does not prevent the premature passage of an insufficiently prepared food bolus into the lower parts of the digestive tract.
Gatekeeper location
FEATURES IN CHILDREN AND NEWBORNS
The structure of the digestive tract in newborns and young children differs from that of adults. By the time of birth, the fundus of the stomach and its cardiac part are not as well developed as the pyloric part, which explains frequent regurgitation and vomiting. The tone of its smooth muscles in infants is increased, which sometimes causes the development of pylorospasm. The gatekeeper is expanded.
Stomach of an adult and a child
The axis of the stomach in newborns is horizontal, and becomes vertical, like in an adult, only by the age of 7–10 years. A gradual change in the position of the axis begins from the moment the child begins to move.
Interesting: It becomes possible to detect the fetal stomach as a local expansion of the spindle-shaped foregut only in the third week of gestation. The formation of the pyloric sphincter begins from the 12th week.
Pathologies of the pyloric part of the stomach
Diseases of the pyloric region of the stomach are always difficult to tolerate, since the transport of the food bolus through the gastrointestinal tract is greatly impaired. Stagnation, accompanying processes of putrefaction and large secretion of gastric juice often provoke the following pathological conditions with a tendency to rapidly become chronic:
Ulcerative-erosive lesion
Ulcerative lesions of the stomach in the photo look like erosions. The main causes of the pathology are non-compliance with the rules of a normal healthy diet, infection by Helicobacter pylori, bad habits, in particular, alcohol abuse.
Regular aggressive effects on the mucous membranes provoke thinning of the mucous epithelium, up to perforation processes, perforation with multiple infectious consequences. The main symptoms of the pathology are:
- the appearance of night hunger pains;
- traces of blood in stool;
- pain when eating and after during active digestive processes;
- weight loss;
- vomiting, nausea;
- development of iron deficiency anemia;
- tarry unstable stool.
Perforation and perforation are the main complications of the ulcerative process. Without timely surgical care, the risks of death due to acute peritonitis and a generalized inflammatory process increase.
Important! Treatment of the pathology is usually surgical with long-term restorative treatment with antibiotics and adherence to a therapeutic diet in accordance with the acidity of gastric juice.
Pyloric narrowing or stenosis
Narrowing of the sphincteral sections of the pylorus or pyloric stenosis is a complicated course of peptic ulcer disease. Pathology can also be caused by the anatomical features of the gastric sections. The mechanism of development of stenosis is the formation of a peptic ulcer followed by scarring of the functioning mucous tissue. Symptoms are expressed in proportion to the dysfunction of the pylorus and are manifested by the following clinical manifestations:
- increased gas formation;
- flatulence;
- constipation, painful bowel movements;
- putrid belching and bad breath;
- nausea, vomiting;
- signs of chronic intoxication.
Stenosis can only be treated surgically. For pyloric stenosis, endoscopic or laparotomy surgery is performed. During the manipulation, scar tissue is excised, leading to a narrowing of the lumen of the sphincter of the lower stomach.
Oncological transformation of cells
The risks of stomach cancer are caused by polypous foci, regular active inflammatory processes, complicated by peptic ulcer disease and erosive lesions of the mucosa. Regular use of medications, as well as their inadequate use, bypassing medical prescriptions.
An important role in the malignancy of tumor cells is played by hereditary burden. If close relatives have a history of stomach cancer, the risk of cancer increases significantly. The main symptoms of oncology are:
- severe pain of unclear localization in the epigastrium, epigastric region;
- feeling of stagnation of the food bolus;
- putrefactive decomposition of food during stagnation;
- vomiting, nausea;
- general malaise;
- sudden weight loss;
- intragastric bleeding.
A common cause of precancer is the appearance of a parietal polypous lesion in the fundus of the stomach. Malignancy of a polyp under the influence of multiple factors often causes malignancy of tumor cells.
Typically, precancer includes chronic ulcerative gastritis with a high risk of perforation and perforation of the stomach walls. When the first symptoms appear, it is important to immediately consult a doctor.
Note! Treatment is only surgical; in the final stages, the organ cannot be preserved. Advanced cases of oncology with penetration of metastases into organs, the tumor is already inoperable.
Damage to the gastric parts of the stomach, including the pyloric one, can be caused by trauma (ruptures after a severe bruise, as a result of a fracture of the chest), chemical burn (accidental ingestion of alkali, poisons, household solutions), severe inflammatory process inside the body, chronic dysbiosis after poisoning, antibiotic therapy .
Diagnosis of pyloric diseases
If you experience abdominal pain, heartburn, belching, or nausea, you should visit a gastroenterologist. After an examination and medical history, the doctor will prescribe the necessary research methods.
How to differentiate pyloric pathologies:
- X-ray of the stomach;
- Ultrasound of the abdominal organs;
- gastroscopy;
- studying the electrical activity of muscles using enterography.
To assess the general condition of the body, a clinical blood and urine test is prescribed.
Preventive actions
The main prevention of inflammatory diseases comes down to following a general protective regime, as well as following a special diet for the entire period of remission between exacerbations.
There is no other specific prevention against diseases of the pyloric stomach, but the following measures will help reduce the risk of developing pathologies:
- maintaining a healthy lifestyle;
- exclusion of tobacco, alcohol;
- timely response to the appearance of any atypical symptoms;
- use of medications only as prescribed by a doctor;
- compliance with the protective regime during exacerbation of chronic pathologies;
- therapeutic diet for exacerbation or severe inflammatory diseases;
- reducing the stress load on the body.
Regular disruptions in the function of the digestive system over the years lead to chronic diseases. The lack of adequate timely assistance often becomes the cause of pathology, even life-threatening conditions. Advanced gastric pathologies are usually eliminated surgically.
The prognosis for the disease depends on the severity of the pathological process, timely diagnosis and spread of inflammatory foci.
Prevention
To prevent the development of diseases of the digestive system, it is necessary to follow simple preventive measures.
How to avoid problems with the pylorus:
- eat healthy and regularly;
- maintain a daily routine;
- give up addictions;
- wear comfortable, loose clothing;
- do not starve, avoid strict diets.
Periodic examination and diagnosis will help prevent the development of complications and avoid surgical intervention.
When the functions of the pylorus are impaired, various pathologies of the digestive system develop; the diseases have different causes of origin, differ in symptoms and treatment methods. But prevention and diet are the same for all sphincter diseases.
Pathologies
Common pathologies in the pyloric region are stenosis, ulcers, erosion, and polyp formation. They are much more severe than the same diseases in the body of the stomach, which is associated with disruption of the movement of food, the development of stagnant and putrefactive processes. Most often, these diseases immediately become chronic.
STENOSIS
Stenosis is a narrowing of the pyloric lumen. The cause of its development is often gastric ulcer, when muscle tissue is replaced by connective tissue due to scarring of the ulcer. Clinical symptoms depend on the degree of obstruction of the food bolus. If the function of the pylorus is preserved, then a feeling of heaviness occurs after eating, which passes over time.
Pyloric stenosis
In severe cases, when complete obstruction forms, stagnation and putrefactive processes begin, leading to stomach fullness, gas formation, belching with an unpleasant taste, nausea, and vomiting after eating. Due to the lack of nutrients, the body is depleted, the person feels weak, and symptoms of intoxication are present. Treatment in this situation is carried out only by surgery.
POLYPOID HYPERTROPHY
Polypoid hypertrophy of the mucosa is said to occur when, during gastroscopy, multiple growths of a glandular structure of a benign nature are revealed. As a rule, they are discovered by chance, since if the size of the growths is small, then the disease is asymptomatic.
With large pathological formations, the risk of gastric bleeding increases, which is manifested by vomiting with blood or tarry feces. There are pain attacks in the abdomen, and the evacuation of food into the small intestine is disrupted. A severe complication of the disease is malignant degeneration of polyps, which leads to the need for surgical treatment.
ULCER
An ulcer is a defect of the mucous membrane with trophic disorders. Its development most often results from infection with the bacterium Helicobacter pylori. However, other reasons are also possible. Peptic ulcer disease manifests itself in the form of pain that disappears after eating, and after a while appears again. A dangerous complication of an ulcer is its perforation and perforation of the stomach, which can be fatal.
Introduction
Surgical treatment of pyloroduodenal ulcers has remained an extremely important, interesting and largely controversial section of surgical gastroenterology for many years. Some success achieved thanks to the capabilities of modern pharmacotherapy has made it possible to significantly reduce the number of planned surgical interventions, but still, like a quarter of a century ago, the number of emergency operations for complicated forms of peptic ulcer disease remains at the same level, and according to some reports, even increased [2, 6-8].
In elucidating the essence of pyloroduodenal ulcers, features of etiology, pathogenesis and diagnosis, fibrogastroduodenoscopy (FGDS) methods, as well as light-optical and electron microscopic studies of biopsy specimens, play an important role [2-5].
The use of intravital morphological research methods makes it possible to connect changes in structures with the state of their functions, i.e. obtain a structural and functional characteristic of the process, judge its dynamics under the influence of surgical treatment. In this case, the issue of treatment tactics is successfully resolved [3, 4]. This would implement the final provisions of the concept of preemptive surgical treatment, allowing to prevent the development of life-threatening complications of pyloroduodenal ulcers [6, 8]. However, to date, despite existing research, this issue cannot be considered finally resolved. The reason is that pathological changes in the mucous membrane of the stomach and duodenum in the immediate and long-term period after selective proximal vagotomy (SPV) and gastrectomy are incomplete and contradictory.
The purpose of the study was to study the results of PPV and gastrectomy, taking into account morphofunctional changes in the gastric mucosa in patients with pyloroduodenal ulcers before and after surgical treatment.
Material and methods
Over the past two decades, in the department of surgical gastroenterology of the Scientific Center for Surgery named after. M.A. Topchibashev operated on 743 patients aged 16 to 80 years with uncomplicated pyloroduodenal ulcers. In 477 (64.2%) patients, the ulcer was localized in the duodenum, in 266 (35.8%) - in the pyloric part of the stomach. All patients underwent esophagofibrogastroduodenoscopy (EFGDS) before surgery.
At the same time, in the pyloric part of the stomach or duodenal bulb, mucosal defects were found in the form of ulcers of various shapes (round, oval, polygonal) and sizes (from 0.3 × 0.5 to 1.0 × 1.5 cm). The bottom of the ulcers is smooth, sometimes fine-grained, the edges are unevenly thickened in the form of a roller. Around them, the mucous membrane was sharply hyperemic and edematous; there were areas of a grayish color. In some places, the mucous membrane became thinner, its vascular pattern was clearly visible, and when touched with the device, these areas bled easily. As you move away from the ulcer, these changes disappear. In 137 (18.4%) patients an ulcer was found in the acute stage. The inflammatory shaft around the ulcer and fibrosis of the deep layers of the wall often changed the normal anatomy of the pyloroduodenal canal. The therapeutic treatment of these patients carried out before surgery gave a partial effect - the inflammatory infiltration around the ulcer significantly decreased.
Based on endoscopic examination data before surgery, it was found that in 539 (72.5%) patients the ulcers were chronic, in the remaining 67 (9%) patients - in the scarring stage.
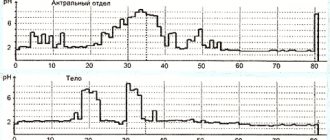
When examining the gastric mucosa before surgery, the majority of patients (585, or 78.7%) had various forms of chronic gastritis with erosion of the mucosa in the body and antrum of the stomach. Morphological changes were manifested by a combination of dystrophic changes in glandular elements and impaired secretion of mucus in the surface epithelium, as well as hyperplastic and atrophic processes with inflammatory infiltration of interstitial tissue and restructuring of glands (chronic hypertrophic gastritis). In 158 (27%) patients, gastroscopy revealed thickening, swelling and hyperemia of the gastric mucosa with minor hemorrhages (superficial gastritis). When examined under a microscope, changes were found mainly in the surface epithelium.
After examining the mucous membrane of the stomach and duodenum, an endoscopic biopsy was performed. To do this, we used the forceps included in the gastrofibroscope kit. The biopsy was taken from the cardiac, fundic, pyloric parts of the stomach and around the ulcerative defect. Paraffin sections stained with hematoxylin and eosin in combination with toluidine blue were light-optically examined, Schiff's reagent in combination with Van Gieson's reagent in combination with Romanovsky's azure-eosin, and the sections were impregnated with silver according to Gomori.
Considering that visual studies of the mucosa with concomitant gastritis do not always correspond to morphological data, histological and histochemical studies of gastrobiopsy material were performed in 159 (21.4%) patients.
The morphological state of the gastric mucosa was studied in 80 (50.3%) patients with pyloroduodenal ulcers before and at various times after PPV with and without stomach drainage operations (pyloroplasty according to Heineke-Mikulich, Finney and gastroduodenostomy according to Zhabula) and in 79 (49, 7%) patients before and after gastrectomy.
All clinical material was divided into the following groups:
1) biopsies taken from patients with pyloroduodenal ulcers before PPV - 160 out of 40 patients;
2) biopsies taken from patients with pyloroduodenal ulcers before resection - 100 out of 25 patients;
3) biopsies taken from patients after PPV with and without gastric drainage surgery - 160 from 40 patients and with complications - 40 from 10 patients;
4) biopsies taken from patients after gastrectomy - 216 from 54 patients and with their complications - 32 from 8 patients.
Results and discussion
In a morphological study of the gastric mucosa before PPV, in 40 (25.1%) patients with pyloroduodenal ulcers, in biopsy samples from the fundus, the gastric pits were smoothed. The integumentary epithelium is in a state of moderate protein degeneration. Substances of mucopolysaccharide nature are localized mainly in the apical parts of cells. The mucous membrane itself is hyperemic, edematous, with diffuse polymorphic cellular infiltration with a predominance of lymphoid elements.
The bodies and terminal sections of the glands have different shapes and sizes, are closely adjacent to each other, and are braided with thin collagen and elastic fibers. Mucous (accessory) cells contain a significant amount of mucoid secretion granules and have a flattened nucleus in the basal part of the cells. There are mitotic figures. In the main glandular cells, the nuclei are located in the center, the protein secretion (pepsinogen) is in the apical part.
Parietal cells were located in the upper parts of the fundic glands, their number was 48.36±1.47 (a comparison of various mucosal parameters before and after surgery is presented in Tables 1 and 2).
In biopsy specimens taken from the body of the stomach before PPV, the mucosa has unevenly distributed gastric pits. The prismatic epithelium is desquamated in places, individual cells are in a state of dystrophy, they show a decrease in mucus secretion, and granules of the secretory substance are located only in the most apical parts of the cells. In the secretory sections of the glands, mucus-forming cells predominate, the cytoplasm of which is filled with granules of PAS-positive material, and in the lumens of the glands there are granules of secretory material. The terminal sections of the glands are formed by chief cells with areas of large, swollen parietal cells.
In gastrobiopsy specimens from the antrum of the stomach to the SPV, there are fragments of the mucosa with shallow gastric pits with no mucus on their surface, and sharp degenerative changes in the integumentary ethipelium are noted.
Secretion granules in some epithelial cells occupy the entire apical part, while in others a small number of granules are located along the apical membrane. The mucous membrane itself is sclerotic, swollen, saturated with fresh red blood cells against the background of severe vascular congestion. The inflammatory cell infiltrate is composed of lymphocytes, histiocytes with a significant admixture of plasma cells. Most of the secretory cells show signs of dystrophy. The cytoplasm of mucus-forming cells is loaded with grains and granules of PHIK-positive material.
Thus, these patients exhibit pathomorphological changes in the gastric mucosa, characteristic of superficial gastritis.
The morphological picture in 20 (50%) patients before PWS was characterized by the development of various forms of hypertrophic gastritis. The integumentary epithelium is tall, prismatic with a large number of granules of CHIC-positive material. There is marked proliferation of the epithelium of the fundus, body and pyloric glands of the stomach. In certain areas of the mucous membrane of the fundus and body of the stomach, phenomena of pylorization of the glands are observed. In some observations, against the background of hypertrophic gastritis, the phenomena of micropolyposis with focal proliferation of the mucous membrane are noted.
It should be noted that out of 40 patients examined before PWS, 7 (7.5%) had normal mucosa. In these patients, the ulcer was located on the anterior wall of the duodenum and had a diameter of about 0.3 cm.
In biopsy samples from the area of the ulcerative defect, in most cases, the duodenal mucosa has high funnels lined with single-layer cylindrical epithelium in a state of dystrophy and necrobiosis (the brush border is not expressed), within which a small number of goblet cells are found, which indicates a decrease in the secretory function of the integumentary epithelium. In the crypt area there are single Paneth cells, the secretory material of which gives a weak PAS-positive reaction. Thus, in biopsy samples from the duodenal mucosa, a picture of chronic inflammation is observed with a decrease in the secretory and impaired absorption function of the integumentary epithelium and a slight reduction of the duodenal glands.
In 40 patients with pyloroduodenal ulcers, biopsy samples taken before gastrectomy showed a picture characteristic of various forms of chronic gastritis (Table 3).
The table shows that before gastrectomy, 3 (12.5%) patients had normal mucous membrane, with the exception of the ulcer area; 5 (20%) had chronic superficial gastritis; 6 (25%) had chronic diffuse gastritis; 6 (25%) had moderate atrophic gastritis; and 4 (17.5%) had severe atrophic gastritis. According to our data, chronic gastritis in the immediate vicinity of the ulcer is detected in 78 (93.4%) patients. As for the localization of changes in the mucosa in patients with ulcers of the pyloric part of the stomach outside the ulcer zone, based on our material we can talk about the predominance of damage to the mucous membrane in the form of either antral or diffuse gastritis. Antral gastritis was detected in 20 (50%), diffuse gastritis - in 16 (40%) patients. It is characteristic that isolated lesions of the fundus mucosa in gastric ulcers are very rare (3.5% of cases).
In 3 (8.3%) patients with ulcers of the pyloric part of the stomach before surgery, small accumulations of intestinal-type epithelium (intestinal-type metaplasia) were found in biopsies taken from the antrum.
Thus, before gastrectomy, chronic gastritis was observed without atrophy of the glands of all parts of the stomach, mainly the antrum (50% of cases), with atrophy of the glands in this area of the stomach (20%) and enterolization of the integumentary pit epithelium (8.3%).
2-3 weeks after the operation, all 30 examined patients showed signs of superficial and deep gastritis. Gastritis after PPV does not have specific features and occurs with the same morphological signs as gastritis during peptic ulcer disease, however, the changes indicate pronounced inflammation. The thickness of the mucosa after PPV, supplemented by gastric drainage surgery, increased to 1131+62.53 µm, the thickness of the glandular layer - to 219+8.7 µm.
After isolated PPV, the number of cells in one gland was 116.74 + l.07, the ratio of chief and parietal cells (CHC) was 1.45, after PPV with Finney pyloroplasty - 120.56 + 1.13 and 1.10, respectively. after PPV with gastroduodenostomy according to Zhabula - 112.33+0.43 and 1.6. In patients in whom PPV was supplemented with pyloroplasty according to Heineke-Mikulich, a significant increase in the number of mucus-forming cells in the glands was detected (OGPC was 0.6).
3-6 months after PPV with and without drainage surgery, it was revealed that in 15.7% of those examined the gastric mucosa was hypertrophied, in the rest it was close to normal. The morphological picture was characterized by mildly expressed phenomena of lymphoid cell infiltration in the surface epithelium.
In the peptic (chief) cells of the fundus and body of the stomach, a significant content of RNP was noted. Parietal (parietal) cells without visible changes. The pyloric glands contain a moderate amount of PAS-positive mucus, which fills the apical parts of the gland cells.
1-2 years after PPV without drainage, gastrobiopsy specimens of 10 patients showed an uneven alternation of gastric pits covered with high columnar epithelium. In some places, focal proliferation of the integumentary epithelium was detected. Moderately pronounced lymphoid-histiocytic infiltration is detected in the mucosa. The glands of the pyloric part of the stomach are of a normal configuration, the cells are in some places expanded like “goblet-shaped” and contain a large amount of CHIC-positive mucus.
The structure of the gastric mucosa 1-2 years after PPV with stomach drainage operations changed ambiguously. In general, there are positive dynamics compared to the picture before surgery and in the early postoperative period, however, sometimes changes in the body of the stomach progress and lead to the development of moderate atrophy. The thickness of the mucous membrane of the body of the stomach after all types of operations decreased compared to that in the early postoperative period, and the thickness of the glandular layer and the depth of the gastric pits also decreased. Atrophic changes in the gastric body mucosa 1-3 years after surgery were noted in patients with delayed initial or complete evacuation of gastric contents. After PPV with pyloroplasty according to Finney, atrophic changes were observed only in single fields of vision, while after pyloroplasty according to Heineke-Mikulich and gastroduodenostomy according to Zhabula - up to the development of moderate atrophic gastritis. In addition, a close connection between changes in the mucous membrane and disorders of the motor-evacuation function of the stomach is obvious. The choice of the optimal gastric drainage operation that ensures adequate emptying of the stomach has a significant impact on the positive dynamics of morphological changes in the gastric mucosa.
The morphological picture of the gastric mucosa by the 4th year after PPV in 15 patients is characterized by a decrease in the intensity of inflammation. The surface epithelium retains a cylindrical shape, and cell boundaries are more clearly defined. The glands of the fundus and body of the stomach are located in even parallel rows without signs of deformation. There are no dystrophic changes observed in the main glandular cells that produce pepsinogen and in the parietal (lining) cells. The glands of the pyloric region showed no visible changes compared to the previous observation period.
In patients with hypertrophic gastritis before surgery, by the 4th year after PWS, the changes were generally identical to those observed after 2 years. However, the severity of inflammatory cellular changes tends to decrease. Mainly at the border of the pyloric and fundic sections there are focal accumulations of lymphoid-histiocytic elements.
A study of the condition of the gastric mucosa in the long term after surgery (from 1 to 4 years) showed that progression of concomitant gastritis does not occur.
It is extremely important that, by causing a decrease in excess mucus secretion, PWS maintains the secretion of protective mucins at a certain level, which are sufficient to provide a protective effect on the mucosa. In not a single observation did we identify acute erosive-ulcerative lesions, indicating a decrease in the protective properties of the mucosa.
As evidenced by the data of our morphological studies, in patients after PPV, the activity of acid and enzyme formation in the cells of their own glands decreases, as well as the intensity of inflammatory cell infiltration of the mucosal stroma, the proliferative processes of the glandular elements are inhibited and excessive mucus formation is reduced.
A pathomorphological study over time was carried out in 54 patients who underwent gastric resection for pyloric ulcers (24) and duodenal ulcers (30). 44 patients were operated on using the Billroth-II method, and 10 patients were operated on using the Billroth-I method.
The most common result of studies of the gastric stump mucosa was the frequent exacerbation of its atrophy over time, regardless of the method of gastric resection (Table 4).
From the table 4 it follows that in the long term after gastrectomy, changes in the structure of the mucous membrane of its stump are found in most patients. As a rule, this is chronic gastritis. A combination of dystrophic and inflammatory changes is often observed. Atrophic processes are detected only in 18.5% of cases. After 3-6 months, as well as the first years after the Billroth-II operation, gastritis develops relatively quickly in the mucous stump of the stomach or the preoperative mild degrees of gastritis worsen; after 3-4 years these changes turn into severe ones. Thus, gastritis of the gastric stump is primarily a consequence of the operation. The abrupt and complete cessation of gastrin secretion due to anthrumectomy appears to be the direct cause of such rapid occurrence of gastritis of the gastric stump. It should be noted that changes in the mucous stump after operations performed by the Billroth-II and Billroth-I methods are the same. This is manifested by the rather frequent and rapid occurrence of gastritis in both cases. Based on this, it is unlikely that bile reflux was the cause of gastritis of the mucous stump, since after operations using the above methods, the conditions for bile reflux are not the same.
In conclusion, it should be noted that the data from a morphological study of the mucous stump of the stomach indicate a relatively rapid onset of gastritis in the postoperative period or aggravation of inflammatory changes, which after 3-4 years turn into severe ones. The intensification of the inflammatory process in the gastric stump appears to be a consequence of the operation itself. 1 year after PPV, with or without gastric drainage surgery, the normal structure of the gastric mucosa is restored. After gastrectomy, as a rule, chronic gastritis of the gastric stump occurs with pronounced symptoms of dystrophy, as well as intestinal and pseudopyloric metaplasia.
Thus, in conditions of a local ulcerative defect, the entire wall of the duodenum is involved in the pathological process. Changes in the mucosa consist of two components: inflammatory-sclerotic and compensatory-adaptive. The latter concerns mainly glandular structures, which undergo a number of stages in the process of compensatory restructuring. It is likely that it is the stage of compensatory restructuring of the epithelium that largely determines the prognosis of the disease. Peptic ulcer disease is characterized by the development of the most pronounced process of enterolization in the pyloric antrum of the stomach. Selective proximal vagotomy does not lead to atrophy of the glandular apparatus of the stomach. It helps to reduce pathomorphological changes in the gastric mucosa that were present before surgery. Moderate or mild inflammation of the gastric mucosa persists for a year after selective proximal vagotomy. After this operation there are no significant changes in the secretory cells of the pyloric glands.