Removing the gallbladder is a common operation. It is necessary for diseases of the biliary system, cholelithiasis, polyps, cholecystitis, and neoplasms. Surgical intervention can be performed using open access, laparoscopically or mini-access. Recovery after gallbladder removal directly depends on the method of cholecystectomy.
The main directions of rehabilitation are diet, drug therapy, wound treatment, and avoidance of excessive physical activity. After the intervention, the body needs time to learn to cope without the organ that stored bile.
During the operation, an incision is made in the abdominal wall, therefore, in the postoperative period, you need to carefully monitor the healing process. If recommendations regarding physical activity and nutrition are not followed, adhesions may form due to the proliferation of fibrous tissue.
Methods for organ removal
Cholecystectomy is performed using laparotomy, laparoscopy or mini-access. During laparotomy, an incision (about 15 cm) is made on the abdominal wall through which the gallbladder (GB) is removed. The method is used if an emergency operation is performed, there are contraindications to laparoscopy, acute inflammation with peritonitis or complex lesions of the ducts are diagnosed.
Since the operation is abdominal, a long period of recovery is required. If healing is normal, the sutures are removed after 7–10 days. The patient is in the hospital for 2 weeks. After 14–20 days, the patient returns to his usual lifestyle, but continues to adhere to a diet, avoids lifting heavy objects (for six months) and swimming in ponds and pools.
Laparoscopic cholecystectomy is considered a minimally invasive procedure. During the operation, 4 incisions of 2 centimeters each are made in the abdominal wall, through which equipment for manipulation is inserted. With laparoscopy, the patient recovers quickly and can be discharged from the hospital in 2-3 days and quickly return to normal life.
With a mini-access, the surgeon makes a 3-7 cm incision in the abdominal wall. This incision is less traumatic than with an open approach, but at the same time provides the necessary overview to determine the condition of the organs. This method is used for adhesions, inflammatory tissue infiltration, and when it is impossible to introduce carbon dioxide.
After surgery to remove the gallbladder, the patient remains in the hospital for 3 to 5 days. Rehabilitation is much faster than after open surgery.
The larger the incision in the anterior abdominal wall is made, the longer the recovery period
Why do you need to remove the gallbladder?
Total excision of an organ is carried out in the presence of one large or numerous small stones in the organ. Until now, no surgical methods have been created that would allow the removal of gallstones from the organ with minimal harm. Unlike the kidneys, pigments are not crushed in the organ. Remains of crushed stones can enter the bile ducts, causing a serious complication - inflammation of the pancreas and jaundice of the skin.
How long does rehabilitation last?
Depending on the cholecystectomy method chosen by the surgeon, the duration of rehabilitation will depend. After open surgery, ability to work is restored within 1–2 months, and after laparoscopy a person is on sick leave for no more than 20 days. The rehabilitation period can be divided into several stages:
Why does my stomach hurt when I lift something heavy?
- early (in hospital). Lasts two days after surgery. During this period, doctors monitor the patient’s condition: how he feels after anesthesia, and if there are any postoperative complications. If necessary, symptomatic therapy is carried out;
- late stage. The patient is still in the hospital. Doctors monitor how the body works without the gallbladder, whether intestinal function is disrupted, and how the wound is healing. This period is 3–6 days during laparoscopy and up to 14 days after laparotomy;
- outpatient rehabilitation. The body fully adapts to new conditions, digestion and well-being are restored. Depending on the type of intervention, it lasts 1–3 months.
For 4–6 hours after treatment, you are not allowed to eat or drink or get out of bed. After six hours you can get up, but only carefully, as you may feel dizzy after anesthesia. All patients experience pain in the incision area, but the intensity and duration of the pain varies.
So, after laparotomy, the patient is given narcotic painkillers (Promedol), and then non-narcotic analgesics (Tramadol, Paracetamol), and after laparoscopy, the pain is described as tolerable and the person does not need painkillers. The next day after removal of the organ, you are allowed to get up and walk around a little.
Upon discharge from the hospital, the doctor will tell you how to speed up recovery after cholecystectomy. Recommendations for diet, physical activity, medication, and suture care apply. Only by following the doctor’s instructions can you recover quickly and avoid postoperative complications.
Recovery in the first days after surgery
After laparoscopy, the person is under the supervision of medical staff for two days. If any unpleasant symptoms appear, they are easily relieved. The most common concerns:
- bitterness in the mouth;
- nausea;
- change in taste;
- feeling of heaviness in the right hypochondrium;
- bloating;
- diarrhea.
With strict adherence to the doctor’s recommendations, improvement in well-being is noted within a week, and full recovery takes six months. After some time, the entire body is rebuilt, but limitations still remain.
Diet during rehabilitation
The gallbladder stored bile synthesized by the liver, and it was released into the small intestine. After the organ is removed, bile enters the intestines gradually and therefore it takes longer to digest food. To speed up digestion, it is important to follow dietary guidelines.
When eating the “right” foods, food will be digested faster, which means there will be no reflux, increased gas formation, fermentation and putrefaction in the intestines. In the first days you can only eat porridge, non-rich soups, fermented milk products, lean boiled meat, pureed vegetables, bananas. After discharge from the hospital, the patient must also adhere to a diet.
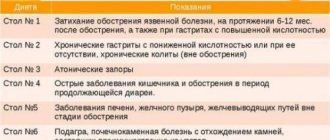
Recommended table No.5
It is forbidden to eat fried and fatty foods, smoked foods, spices, canned food, marinades, sweets, butter, eggs, and you cannot drink coffee or alcohol. Digestion will recover faster if you not only stick to a diet, but also follow a meal schedule. For a month after discharge from the hospital, it is necessary to organize 5-6 meals a day.
Food should be eaten in small portions every 3 hours. It is advisable to eat at the same time so that bile is produced at a certain time. Before eating (10-15 minutes before), it is recommended to drink a glass of water so that the gland starts working.
From 5-6 days you can eat:
- pureed soups in weak meat broth or water;
- boiled fish;
- egg white omelet;
- 100 g of crackers, biscuits or dry white bread;
- liquid mashed porridge with water and half and half milk;
- unsweetened cottage cheese;
- from meat - beef, veal, chicken and rabbit;
- dairy products.
It is recommended to consume 1.5-2 liters of liquid in fractional portions. It is allowed to switch to a gentle diet from the eighth to tenth day - you should stick to it for at least one and a half months. Until three months it is forbidden to lift more than 5-7 kg. These simple rules allow you to easily endure the postoperative and recovery period without complications.
Drug treatment
Since removal of the gallbladder is performed as a last resort, there is a high probability that the inflamed organ has affected the functions of other organs. Often in the postoperative period, the symptoms intensify because the body has not yet adapted to the new conditions. Depending on the complications, the doctor will prescribe the necessary medications.
So, when reflux occurs, anti-reflux drugs are prescribed; if erosions appear on the gastric mucosa, then drugs that reduce the acidity of gastric juice and the enveloping walls of the organ are indicated. Treatment with medications after gallbladder removal is usually not required. To normalize digestion, medications with enzymes (Mezim, Festal, Pancreatin) are usually prescribed.
Choleretic drugs may also be recommended. To improve the excretion of bile, choleretic herbs can be used in consultation with a doctor. Beetroot juice (first diluted with water), a decoction of corn silk and tansy, as well as immortelle, rhubarb and yarrow roots are useful. To stimulate bile secretion, you can use the following method. Before breakfast, drink a glass of warm mineral water without gas (Essentuki 17), lie on your right side and apply a warm heating pad to the liver for 30–40 minutes.
Hiking
The first walks should not last more than 30 minutes. Thirst will arise. Bring still or boiled mineral water with you. Boil water for at least 30 minutes. Drain the top third.
Wear linen T-shirts under warm clothes. Move slowly. If you have a bandage, sit down after 10 minutes. There should be no burden. The step is measured.
Dizziness, burning sensation in the operated area - reduce walks to 15-20 minutes. Don't go far from home. Once a month, go to the coniferous forest. Walk on flat ground. Avoid excessive sweating in the operated area.
Physical activity
During the healing period of the wound (for a month), you should limit physical activity, do not make sharp turns and do not lift weights over 2-3 kilograms, and do not perform exercises that involve the abdominal muscles. After the cut tissues have healed, you can begin to engage in physical therapy.
The load on the abdominal muscles should increase gradually; it is recommended to do the “scissors” and “bicycle” exercises. Long walking at a fast pace is beneficial. Adequate physical activity will help improve intestinal motility and increase the supply of oxygen to tissues. If you ignore the restriction and lift weights, the stitches may come apart or a hernia may form.
After six months after surgery, any restrictions associated with physical activity are removed
Breathing exercises
Start performing on the 5th day:
- Position lying on your back; slow breath; hold your breath for 1-3 seconds; exhale very slowly – 1-3 repetitions.
- Short inhalations and exhalations: start from day 5-7 for 30-60 seconds – increase to 2-3 minutes.
- Position, standing; when inhaling, rise on your toes, raise your arms up, stretch your whole body up; exhale – starting position; inhale – 15-30 – exhale 10-15 seconds; start on the 10th day after surgery.
Attention! Stop breathing exercises at the slightest dizziness.
Wound care
Inflammation and swelling appear at the site of tissue dissection. In the absence of proper care of the suture, suppuration may begin or a hypertrophic scar or keloid may form. One of the important factors that influence wound healing is the number of bacterial flora in the wound (the wound takes longer to heal due to the action of bacterial proteases).
There may be redness and induration around the wound. Wound infection occurs in 1–2% of patients. In case of severe inflammation, you should consult a doctor, because if the wound becomes suppurated, surgical intervention for debridement and antibiotic administration may be required.
You can take a shower two days after the operation. Water will not penetrate the wound, but you should not rub it with a washcloth or soap it. After water procedures, the wound should be lubricated with iodine or brilliant green. Bathing is allowed only 5 days after the stitches are removed.
Possible consequences
Bloating and flatulence may be symptoms of complications after surgery
The main complication is postcholecystectomy syndrome - digestive disorders due to uneven redistribution of the load between the organs that secrete secretions in the gastrointestinal tract - the stomach, pancreas, liver, as well as the microflora of the large intestine.
The syndrome may appear 4-7 years after surgery. The type of surgery does not matter. With the development of the syndrome: constant heartburn, flatulence, dysbacteriosis, dyspepsia.
Other complications.
- Suppuration in the operated area with possible blood sepsis.
- Immune diseases.
- Autoimmune manifestations - allergies, inflammatory diseases throughout the body.
What do experts recommend?
- After removal of the gallbladder, permanently exclude beer and pork fat from the diet, regardless of heat treatment; meat, fish, eggs that have undergone improper heat treatment; give preference to plant foods - carrots and beets daily.
- Avoid hunger – satisfy hunger even at night; meals are fractional.
- Gradually accustom the body to physical activity - this also applies to athletes.
- Any medications only as prescribed by a doctor; folk remedies - only pharmacy preparations or a prescription drawn up by the attending physician.
- Take general and biochemical blood tests, and do an ultrasound of the abdominal cavity 2 times a year.
- Do not sunbathe for more than 2 hours a day; Avoid midday sunlight.
Indications and contraindications for cholecystectomy
Cholecystectomy is the surgical removal of the gallbladder; it is performed for various forms of cholecystitis and the development of atrophic processes in the organ. The main reasons for the development of pathologies are errors in nutrition, sedentary lifestyle, helminthic infestations, hormonal imbalance, gastrointestinal diseases, obesity.
When surgery is required:
- blockage of bile ducts and excretory tracts with stones;
- cholecystitis in the acute stage;
- cholelithiasis;
- severe dysfunction, rupture of the gallbladder;
- the presence of polyps on the mucous membrane of the organ.
Important! Most doctors recommend resection if the size of the stones exceeds 2 cm; conservative treatment methods do not improve a person’s well-being.
Contraindications
Cholecystectomy is a necessary surgical intervention that helps to avoid the development of severe complications, but in some cases it cannot be performed.
Main contraindications:
- cholelithiasis without obvious signs in elderly patients;
- serious problems with the respiratory system, heart, kidneys;
- III trimester of pregnancy;
- peritonitis;
- adhesions in the organs of the digestive tract, the presence of malignant neoplasms in the body;
- cirrhosis, pancreatitis in the acute stage;
- problems with blood clotting.
The operation is not performed if the attack of acute cholecystitis lasts more than 72 hours; first, the main symptoms are relieved, then the affected organ is removed.