The intestines are the most important part of the digestive system. It is located in the abdominal cavity. Various processes related to the digestion of food and absorption of nutrients occur in it. This structure begins with the duodenum and ends with the anus.
The mucous membrane of the intestinal tract produces a number of biologically active substances that are simply necessary for the physiological breakdown of products. Knowledge of the location and structure of this important organ, as well as an understanding of how it works, helps to navigate when providing first aid.
Anatomy of the human gastrointestinal tract
The human gastrointestinal tract (its anatomy is a collection of organs designed to carry out the digestion process) has an average length of 8 to 10 m.
The gastrointestinal tract performs the following functions:
- Motor. Consists of moving food through the organs of the tract with the help of muscles.
- Secretory. It represents the production of juices by glandular cells.
- Suction function. It is the process of penetration of nutrients and fluids into the bloodstream.
- Excretory (excretory).
- Endocrine (formation of various hormones - gastrin, secretin).
What do "functional diseases" mean?
The sections of the gastrointestinal tract do not work in isolation “on their own.” They are connected by control from the nervous system and endocrine organs that secrete hormones. In addition, substances synthesized by the cells of the stomach (gastrin, secretin) and pancreas have hormonal activity. In the oral cavity there are endings of nerve fibers that transmit information to the center about the quantity and quality of food received.
Therefore, based on feedback signals, the stomach and intestines are prepared in advance. For example, an order is “formed” for the volume of bile and pancreatic juice required for digestion in the duodenum. The contractile function that pushes the food bolus to the next level is regulated by innervation, most often the vagus and sympathetic nerves are involved. They “take care” of sufficient strength of the peristalsis wave, alternate or simultaneous contraction of the longitudinal and circular muscles.
An important role is played by the correct functioning of the sphincters. These are muscle sphincter located on the border of the esophagus and stomach, stomach and duodenum. Inside the duodenum, the sphincter of Oddi acts as a passageway. It allows pancreatic juice and bile from the supply ducts into the small intestine. When passing into the cecum, the role of a valve is played by a fold of mucous membrane.
It only works if the intestine is located at a certain angle to the end of the small intestine. Powerful sphincters of the sigmoid colon allow the accumulation of feces and their removal into the rectal ampulla for defecation. Functional diseases are diseases that arise due to a mismatch of signal information and orders from the centers of the brain.
Due to impaired contractile activity, stagnation of contents occurs in the stomach, esophagus, and intestines. Or, conversely, excessive contractions remove undigested residues and prevent the absorption of nutrients and vitamins. Such disorders are called dyskinesias. Failure to compress and relax the sphincters causes spastic muscle contractions, expansion of the overlying part of the gastrointestinal tract, insufficient production of enzymes, and stagnation with the risk of infection.
This mechanism is often considered as the initial one in the formation of pathology. It is reversible when the causes of the violation are eliminated.
Diagnosis is carried out by a gastroenterologist
Most often, functional diseases arise under the influence of stressful situations, hard work, alternating periods of fasting and digestive overload, alcohol intake, and drugs. If measures are not taken at this stage, the pathology becomes organic, accompanied by anatomical changes in the structure of organs, and at the cellular level - gross deviations in composition and structure. For example, epithelial metaplasia is the transformation of stomach cells into intestinal cells during gastritis.
Structure and functions of the gastrointestinal tract
Different sections of the gastrointestinal tract have different structures and perform strictly defined functions.
Oral cavity
In front, the oral cavity is covered by the lips. On the sides it borders with the cheeks, and is separated from above by the hard palate. At the back is the pharynx, which leads to the pharynx.
The functions of the oral cavity are food grinding and enzymatic function.
Pharynx
This is an unpaired organ that looks like a funnel. The pharynx is located between the oral cavity and the esophagus. In front of the pharynx is the larynx, nasal cavity and oral cavity. It is attached superiorly to the occipital bone. The top of the pharynx is called the fornix. The pharynx is divided into the nasopharynx, oropharynx and laryngopharynx.
Esophagus
It is a thin muscular tube. In the cervical region it is narrowed, then gradually begins to expand, moving into the abdominal part. The wall of the esophagus is lined with mucous membrane, submucosal layer and muscles.
Stomach
In its structure, it has 2 walls (back and front) and 2 holes. A greater and lesser curvature is formed along the posterior wall of the stomach. The stomach has a cardiac opening through which it communicates with the esophagus. The second exit is the gatekeeper area.
The convex opening of the stomach is represented by the fundus of the stomach. The body of the organ is located between the bottom and the pylorus.
The wall of the stomach is formed by the mucous membrane, which forms folds. On the mucous membrane there are pits in which the glands pass. The stomach is covered with mucous, submucosal, muscular layers and serous membrane.
Intestines
The human gastrointestinal tract (anatomy includes the entire intestine) is complex. The small intestine is represented by the cecum, colon, sigmoid and rectum. The small intestine consists of the duodenum, small intestine and jejunum.
Anal hole
The anus is the final anatomical formation of the digestive tract. It is surrounded by sphincters, which are formed from muscle fibers: the internal one, which is formed by smooth muscles, and the external one, consisting of striated muscles.
What is the gastrointestinal tract and how does it work?
The gastrointestinal tract can be represented schematically as a “tube” that begins in the oral cavity and ends in the anus. In this structure there are departments of the gastrointestinal tract, each of which is responsible for certain tasks. To understand what disorders cause diseases, we will “walk with food” along the tract and check which functions of the gastrointestinal tract are assigned to each department.
The better the food is chewed, the more accessible it enters the stomach; saliva disinfects the food, protecting the underlying parts of the system.
Oral cavity
In the oral cavity, food is met by teeth, which crush it into small pieces, saliva (the secretion of large and small glands), and the tongue. Enzymes in saliva break down starchy substances in foods, and as a liquid it moistens and makes it easier to swallow. Prolonged chewing can deceive the hunger center and cause a feeling of fullness, therefore it is recommended for obese patients to combat excess weight.
Lack of teeth in old age and problems with prosthetics significantly complicate the process. In a hurry, a person swallows pieces of food that are not prepared for digestion, which threatens the functional failure of the next stage in the stomach. Receptors on the tongue determine and transmit information about the amount and composition of enzymes that will be required for digestion.
Esophagus
In fact, it ensures the delivery of food mass to the stomach due to longitudinal and transverse contractions of the muscle layer. The further process is localized below the diaphragm, in the abdominal cavity. Violation of the act of swallowing due to structural anomalies or inflammation (achalasia, esophagitis) leads to delay and stagnation of the bolus. The delay in the entry of food into the stomach affects the activity of the glands of its inner lining.
Stomach
The stomach has an elastic folded structure that allows it to expand significantly. If necessary, the organ can hold up to 4 liters of liquid and food. Not all products are processed equally quickly: glucose, alcohol, salts, and water are absorbed into the blood first. The food residue is affected by gastric juice. The active substances in it are mucus, hydrochloric acid, enzymes (pepsin, gastrin).
The production of juice is carried out by parietal cells located between the epithelial cells. It is produced by the sight and smell of food. Maximum expenses are incurred on processing meat and spicy dishes. Changes in the form of atrophy disrupt the functioning of the organ.
Acidity decreases as it approaches the opening into the duodenum
The stomach muscles mix the mass to increase the area of contact with enzymes.
Duodenum
The initial part of the human intestinal tract is the duodenum. Its task is to obtain food mass from the pylorus of the stomach, convert the acidic reaction into an alkaline one (more suitable for the intestines) and continue the breakdown of proteins and carbohydrates. From the duodenum, minerals, vitamins, and excess fluid are absorbed into the blood.
Diseases of the duodenum
At this stage, the synthesized pancreatic secretion and bile are connected to digestion by joining the ducts through the common sphincter of Oddi.
Bile is produced by hepatocytes (liver cells), collected in the bladder, and contains, in addition to water, fatty acids, cholesterol and inorganic substances.
The composition allows you to emulsify the fatty components of food, break them down into amino acids, fatty acids, vitamins, and prevents rotting processes. Pancreatic juice flows through the pancreatic duct, containing more than 20 enzymes that affect all components of food. The final process of digestion occurs in the loops of the small and large intestines.
Diagram of the flow of the pancreatic and bile ducts into the intestine
Intestines
The length of the small intestine is up to 6 m. In addition to the duodenum, it includes the jejunum and ileum. The wall must ensure the absorption of necessary substances into the blood vessels. To do this, it is covered from the inside with folds and tiny fibers. Large molecules do not pass through the dense shell.
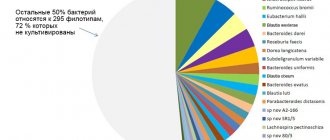
About 200 species of bacteria live in the intestines. The maximum amount is made up of beneficial bifidobacteria and lactobacilli. The remaining opportunistic pathogens are normally included in 1–2% of the structure. Maintaining the correct composition of intestinal flora is very important for digestion. It is these tiny microorganisms, together with intestinal juice, that ensure the breakdown of food debris into molecules to be absorbed (amino acids, polysaccharides, fatty acids).
Imbalance of microflora is sensitive to the influence of various factors, of which special attention is paid to medicinal substances (antibiotics). Therefore, after treating the gastrointestinal tract with antibacterial agents, it is necessary to restore the required ratio of bacteria.
All substances from the intestine do not enter the general bloodstream, but into the portal vein of the liver. The fact is that in the form in which they are presented in the intestines, chemicals can cause death because they form poisons and toxins. The liver disinfects poisons into non-toxic compounds. The ileum “passes” leftover food to the large intestine.
Auxiliary organs
In addition to the main ones that are directly part of the digestive system, auxiliary organs also play an important role.
Liver
The liver is the largest gland in the human body. It is located in the right hypochondrium, in the abdominal cavity. It is divided into 2 lobes, which are separated from each other by the falciform ligament.
The liver is covered with peritoneum and a fibrous membrane. It is formed by hepatocytes (cells) that participate in the formation of bile. The liver contains large nerves and blood vessels.
Gallbladder
The gallbladder is located on the back of the liver and is connected by a duct. In its shape, this organ resembles a pear. The gallbladder performs the function of producing bile.
Glands
The entire group is formed by the glands of the intestines, stomach, salivary glands, liver and pancreas. The largest are the pancreas and liver. Small ones are located in the mucous layer of the intestines and stomach. They are involved in the digestion and absorption of food elements.
Channels
The gastrointestinal ducts are intrahepatic and extrahepatic bile ducts that merge into one hepatic duct. Subsequently, it connects with the cystic duct and they form the common bile duct.
With the help of ducts, bile is able to circulate throughout the body. The sphincter of Oddi is responsible for regulating its supply.
Walls of the gastrointestinal tract
The walls of the gastrointestinal tract are represented by 3 layers. From the inside they are covered with a mucous membrane, the middle layer is muscle fibers, and on the outside the tract is lined with a serous layer.
- The mucous membrane is formed by epithelium.
- The muscular coat is represented by striated muscles and smooth muscle fibers.
- The serous layer consists of connective tissue. It performs a protective function.
How does digestion and excretion occur?
When food enters the mouth, the process of digestion begins. With the teeth, food is crushed to the smallest particles, moistened with saliva, which contains enzymes. Next, food moves through swallowing into the esophagus and then into the stomach.
In the stomach, food begins to break down under the influence of hydrochloric acid and enzymes. Having broken down into proteins, it moves further into the intestines in a liquid state. The breakdown process continues in the small intestine with the help of enzymes.
Everything else goes to the large intestine. The process of absorption of fluid and the formation of feces occurs in it. They are subsequently eliminated from the body during bowel movements.
Physiology
Digestion of food begins in the mouth. Chewing thoroughly helps make this process easier. Next, the food bolus enters the esophagus, stomach and duodenum. In the initial part of the organ, food combines with bile secretions and pancreatic enzymes. Under the influence of these excreta, the food bolus is broken down.
The muscle layer ensures uniform distribution of nutrients along the inner wall. In addition to digestive function, the human intestine is responsible for endocrine and immune processes. Special microflora improves digestion processes and is responsible for the secretion of vitamins.
The intestines are responsible for the flow of hydrochloric acid into the stomach, due to which the primary processing of food occurs. Next, the eaten foods are broken down into individual components. From them the body takes for itself the necessary microelements and water. Then the formation of feces and their further evacuation occurs.
Important! The structure of the human intestine begins with the pylorus of the stomach and ends with the anus.
The job of the intestines is to absorb nutrients from food digested by the stomach. All these processes are supported by bacteria that form microflora. In addition, the intestine is an organ of the immune system. It serves as a barrier to pathogens trying to attack the human body.
[node:field_field_doprekl2]
Development of the digestive organs
The development of the digestive organs begins in the embryonic period, at 4 weeks of intrauterine development. The future digestive system develops from the intestinal tube. It is attached on one side to the yolk sac.
Gastrointestinal tract. Anatomy
Subsequently, it develops and is divided into the following sections:
- Primary intestinal tube.
- Anterior section.
- Middle department.
- Posterior section.
Gastrointestinal diseases and their symptoms
The human gastrointestinal tract is highly susceptible to the development of pathological changes. Both adults and children are susceptible to them. The latter suffer more often from inflammatory diseases, since their anatomy contributes to this.
Stomatitis
One type of gastrointestinal disease is stomatitis. It is an inflammatory disease of the oral mucosa.
There are several types of stomatitis:
- Viral. The main cause is various viral diseases. For example, “childhood infections” (measles, rubella, scarlet fever), herpes viruses, including varicella zoster virus, herpes virus, and cytomegalovirus. If stomatitis is caused by the herpes virus, it will be called herpetic.
- Bacterial. This type of stomatitis is caused by staphylococci and streptococci. Most often it occurs in people with chronic foci of infection in the oral cavity and pharynx (caries, chronic tonsillitis), as well as in children, mainly due to poor hygiene.
- Aphthous. The etiological factors of this type of stomatitis have not been fully studied.
- Allergic. Is a manifestation of any allergic reaction.
- Candidal stomatitis. The cause of its development is a fungus. Most often it occurs against the background of immunodeficiency (with chronic diseases or after previous illnesses). There is a frequent occurrence of stomatitis in people undergoing chemotherapy.
Clinical symptoms of stomatitis include the following:
- Pain in the mouth. The pain may be so severe that the person cannot speak, drink, or eat. Infants refuse the breast and any liquid. Children may also develop fever with a temperature up to 38°C and enlarged submandibular lymph nodes.
- Rashes. With the development of herpetic stomatitis, a papular rash filled with serous contents is observed; after a while it opens and ulcers form on the mucous membrane. With aphthous stomatitis, ulcers (aphthae) are found on the mucous membrane, which after some time scar and disappear. With other types of stomatitis (bacterial and allergic), rashes in the form of red spots are possible.
- Hyperemia of the oral mucosa. On examination, the mucous membrane is hyperemic and edematous.
- White coating on the mucous membrane. With candidal stomatitis, a white coating is observed on the inner surface of the cheeks, gums, and hard palate.
- Fever (mainly in children).
- Profuse salivation.
Esophagitis
Esophagitis is an inflammation of the mucous membrane of the esophagus. It can be acute or chronic. More often, esophagitis is a manifestation of other diseases of the gastrointestinal tract.
Symptoms of the pathology include:
- Pain behind the sternum. The patient complains of a burning sensation in the esophagus. The pain intensifies when swallowing food and goes away with rest.
- Heartburn. Occurs when hydrochloric acid refluxes into the esophagus due to reflux.
- Nausea and vomiting. When the esophagus is injured, vomiting mixed with fresh blood occurs.
- Increased body temperature.
- Dysphagia. The patient has difficulty swallowing food or liquid.
Gastritis
Gastritis is an inflammation of the gastric mucosa. It arises against the background of a variety of reasons. The development of the disease may be associated with dietary disorders, the bacterium Helicobacter pylori, and taking medications. Gastritis often occurs in people undergoing chemotherapy or radiation therapy. In this case, the disease is called “radiation gastritis”.
According to the course, acute and chronic forms of the disease are distinguished. There are also erosive and non-erosive gastritis, with high or low acidity. Depending on the type of pathology, clinical manifestations will differ.
In the acute course, the symptoms occur vividly, causing the patient serious discomfort. With a chronic disease, the patient will experience only minor disturbances in well-being.
Erosive gastritis occurs with the appearance of erosions on the wall of the stomach. This condition very often turns into a peptic ulcer, which is fraught with the development of complications, including gastric bleeding.
Symptoms of gastritis:
- Pain in the epigastric region. Usually has a dimly expressed character. In chronic cases, periodic dull pain is possible.
- Nausea.
- Heartburn, sour belching.
- Dyspeptic disorders. There is diarrhea. The stool may be watery with an unpleasant odor, but there is no increase in body temperature.
- Loss of appetite and feeling of fullness in the stomach.
Duodenitis
Duodenitis manifests itself in inflammatory processes that involve the mucous membrane of the duodenum. It rarely occurs as a separate disease. Most often, the pathology manifests itself in conjunction with peptic ulcer disease, as well as with the development of intestinal infections.
The sources of duodenitis are many factors:
- Intestinal toxic infections.
- Acute and chronic gastrointestinal diseases.
- Alcohol abuse.
- Eating fatty foods.
There are catarrhal, phlegmonous and ulcerative duodenitis. The most dangerous is phlegmonous, it can lead to the development of serious complications, including peritonitis (inflammation of the peritoneum).
Duodenitis manifests itself as vomiting, abdominal pain, and possible pain on palpation. Weakness, lethargy, fever, and pale skin are observed.
Cholecystitis
Cholecystitis is an inflammation of the gallbladder due to blockage of its ducts by a stone. This pathology is a consequence of cholelithiasis, but can also be an independent disease in various infections, immunodeficiency conditions, and tumors. This kind of cholecystitis is called non-calculous.
Clinical manifestations are:
- Pain syndrome in the area of the right hypochondrium. The pain is similar to the condition of biliary colic, but lasts much longer. Plus, after a few hours Murphy's syndrome develops (during inhalation, palpation in the right hypochondrium causes spontaneous cessation of breathing).
- Attacks of nausea and vomiting.
- Bitter taste in the mouth.
- Increase in body temperature to 38°C.
- Loss of appetite.
- Diarrhea.
How severe the clinical manifestations of the disease will be depends on the course of cholecystitis and its type. Thus, with phlegmonous or gangrenous cholecystitis, severe fever (up to 40°C), irritation of the peritoneum, and severe intoxication of the body are possible. With this development of the disease, complications may arise.
In the chronic course of cholecystitis, short-term pain in the right hypochondrium, loss of appetite, weight loss, yellowness of the skin and mucous membranes are possible.
Biliary dyskinesia
Biliary dyskinesia is a violation of motility in the gallbladder, which manifests itself in a violation of the outflow of bile. The causes are disorders of the autonomic nervous system and pathological changes in the gallbladder.
There are hypokinetic and hyperkinetic forms of the disease. In the first type, motor function is reduced, and in the second, on the contrary, it is increased.
Clinical manifestations are:
- Pain syndrome in the epigastric region with irradiation to the right hypochondrium. An attack of pain occurs after eating or increasing physical activity. It is characterized by dull periodic pain.
- Nausea, sometimes vomiting, bitterness in the mouth.
- Jaundice discoloration of the skin. This symptom is not observed in all cases of pathology.
Pancreatitis
Pancreatitis is inflammation of the pancreas. Often a relapse of acute pancreatitis occurs from foods with high fat content. The development of inflammation of the pancreas can also be caused by injuries, cancer and poisoning.
Clinical manifestations are:
- Pain syndrome. The pain is localized at the beginning of the attack in the epigastric region, then takes on a girdling character.
- Increased body temperature.
- Vomiting of bile without relief.
- Yellowness of the skin (may or may not be present).
Pancreatitis is dangerous due to its complications, namely peritonitis. With peritonitis, there is a sharp deterioration in the patient’s well-being and an increase in the symptoms of intoxication of the body. If such a patient is not provided with medical assistance within 24 hours, death is possible.
Enteritis
Enteritis consists of inflammation of the mucous membrane of the small intestine. There are acute and chronic courses of the disease. Acute occurs in infectious diseases (salmonellosis, typhoid, cholera), food poisoning.
Chronic enteritis occurs with certain intestinal diseases (Crohn's disease, irritable bowel syndrome), tumors, poor diet, taking certain medications, as well as infection with Giardia and other parasites.
Clinical picture:
- Abdominal pain.
- Diarrhea.
- Vomiting and nausea.
- Temperature increase.
- Weakness.
In a chronic course, as a rule, the symptoms are hidden. The patient may be bothered by mild pain in the abdomen and loose stools.
Colitis
Colitis is considered as an inflammation of the mucous membrane of the large intestine. There are acute and chronic forms of colitis. Acute colitis occurs with infectious diseases (dysentery), poisoning, diseases of the digestive system and some autoimmune diseases.
Symptoms of colitis:
- Stomach ache.
- Flatulence. The patient also experiences constant “rumbling” in the abdominal cavity.
- Diarrhea. In acute cases, stool is frequent and tenesmus (false urge to defecate) is observed. In chronic cases, stool can be observed up to 5 times a day. Most often, bowel movements occur after eating.
- Paleness of the skin. Dry skin and the appearance of cracks are also observed. This is due to impaired absorption of vitamins into the body.
- Increased body temperature in acute cases.
Proctitis
Proctitis refers to inflammatory diseases of the rectum. It occurs against the background of inflammatory bowel diseases, infectious, and radiation exposure to the rectum.
As the disease develops, the patient complains of a constant urge to defecate. However, they are false and defecation does not occur. You may see blood or mucus in the stool. In some cases, the patient may feel severe pain in the rectum and anus.
Other diseases
Other diseases of the digestive system include:
- Gastric ulcer (this is a chronic disease characterized by the formation of ulcers on the gastric mucosa). Symptoms of the disease include pain in the epigastric region, heartburn, and “hunger pains.” An ulcer is dangerous due to its complications. Namely, bleeding, peritonitis and degeneration into gastric cancer.
- Cirrhosis is a chronic liver disease characterized by its gradual destruction. This disease often occurs due to alcohol abuse, viral hepatitis, cancer and some autoimmune diseases.
- Haemorrhoids. It is a varicose vein of the hemorrhoidal plexus. Occurs after childbirth or during pregnancy, due to heavy lifting and excessive straining during bowel movements. Symptoms include blood in the stool and pain in the anus.
Departments
Let's talk about the two main sections of the intestinal tract: the small and large intestine.
Thin
The small intestine is a multifunctional organ, the activity of which determines the coordinated functioning of the entire digestive system. It performs a secretory function, that is, it secretes juice necessary for the breakdown of food. Digestive secretions include mucus, which prevents the intestines from self-digesting.
In addition, the organ performs an absorptive function. Nutrient compounds are absorbed through the mucous membrane. The structure of the mucous layer of the intestinal wall ensures the absorption of exclusively beneficial elements. Endocrine function is ensured by the ability of cells to secrete peptide hormones. They affect the functioning of not only the intestinal tract, but also the entire body.
The muscle structures of the organ are responsible for motor function. The contraction of these muscles ensures digestion, separation of the food bolus and its further pushing. Diseases of the small intestine can have an inflammatory, functional or tumor nature. Some pathologies are congenital, while others are acquired.
Let's look at the most common diseases of the small intestine:
Diseases of the small intestine
- enteritis. Inflammation of the mucous membrane can be caused by exposure to viruses, bacteria, parasites, and fungi. As the disease progresses, the mucous layer swells and turns red. The disease can be acute or chronic;
- allergy. The immune system reacts violently to certain foods that come into contact with the mucous membrane of the small intestine. The pathology provokes the appearance of skin rashes, swelling of the mucous membranes, as well as the appearance of dyspeptic disorders;
- tumors: lipomas, polyps, fibromas;
- peptic ulcer. Most often the disease is localized in the duodenum. The main etiological factor in the occurrence of the disease is Helicobacter pylori infection. An important role is played by genetic predisposition, the presence of bad habits, and emotional stress;
- ileitis. The disease causes inflammation of the final section of the small intestine. The cause of the disease is usually a viral or bacterial infection. Ileitis causes abdominal pain, nausea, as well as a disturbance in the general condition, up to an increase in temperature.
Thick
The thick section has larger dimensions and a wider diameter. Three muscle bands are responsible for peristalsis and the movement of feces. Muscle structures are unevenly distributed. Upon examination, it looks like a cluster of bulges and constrictions.
Attention! Most of the beneficial bacteria live in the large intestine.
The main function of this department is the formation of feces. After entering the thick sections, chyme loses liquid, so its structure changes, it becomes denser and takes on the appearance of feces. A common disease of the large intestine is ulcerative colitis. Chronic inflammation of the mucous membrane causes destructive changes and the formation of ulcers.
The reasons are still not fully understood, but scientists note a connection between UC and genetic factors. The influence of smoking and oral contraceptives on the development of chronic intestinal inflammation was also recorded. Patients develop diarrhea with the release of scarlet blood. There is pain in the abdominal area.
[node:field_field_doprekl]
Another common pathology is Crohn's disease, which causes granulomatous inflammation. The disease can affect any part of the gastrointestinal tract and causes intestinal upset. The number of bowel movements per day can reach up to twenty times a day.
According to statistics, in developed countries, older people are at risk of developing diverticulosis. The pathology is characterized by the appearance of protrusions on the intestinal wall. The main role in the formation of the disease is played by poor nutrition, in particular, an addiction to flour and meat dishes, along with a lack of plant foods.
The intestinal tract consists of two main sections: the small intestine and the large intestine.
Diagnostic methods
The human gastrointestinal tract (its anatomy has a complex structure) for any pathology requires specific diagnosis:
- EGDS (esophagogastroduodenoscopy) - this study is an examination of the esophagus, stomach and duodenum using an endoscope. This method is used if esophagitis, gastritis, ulcers, or tumors are suspected. With its help, you can assess the condition of the mucous membrane and identify the slightest deviation from the norm.
- Colonoscopy - This is an endoscopic examination that allows you to examine the mucous membrane of the colon. With its help, you can assess the condition of the intestines, see if there is inflammation, neoplasms and other defects. A diagnostic biopsy can also be performed using a colonoscopy.
- Sigmoidoscopy is a method in which a doctor examines the rectum.
- Irrigoscopy is an X-ray examination of the large intestine. This is done using a contrast agent. This method is used when colonoscopy results are questionable or when endoscopic examination is impossible.
- X-ray of the stomach . Allows you to determine the presence of tumors, hiatal hernias, stenosis.
- Ultrasound.
Intestinal anatomy
How many meters is the intestine of an adult? The organ is structurally divided into two main parts - the small and large intestine. The length of the first section can reach four meters. The small intestine is shorter in women than in men. It consists of three main departments:
- duodenum;
- skinny;
- iliac.
This department is responsible for digesting food. It has a small diameter and thin walls. Moreover, this structure covers almost the entire lower space of the abdominal cavity and even partially the pelvis. The thin section is also responsible for moving feces further along the intestinal tract, hormonal secretion and strengthening the immune system. The overall work of the enzymes of the small intestine, gall bladder and pancreas ensures the breakdown of the food bolus into monocomponents.
Attention! The average length of the human intestine is four meters. The thin section is longer than the thick section.
The thick section can reach one and a half meters. Anatomically, it consists of the following parts:
- blind;
- ascending;
- descending;
- transverse;
- straight;
- sigmoid.
No ads 1
After death, the length of the human intestine can reach eight meters. This is due to muscle relaxation. There are no villi on the mucous membrane of the large intestine. There is no active absorption of nutrients here.
This section of the intestine is necessary for the proper formation of feces. Here the absorption of water and the formation of feces from chyme occurs. Along the intestinal wall there is an accumulation of lymphoid tissue. She takes an active part in the processes of the immune system.
The photo shows the structural features of the gastrointestinal tract
Treatment
The human gastrointestinal tract, whose anatomy is represented by complex structures, requires complex treatment:
| Principles | Methods |
| Medicines |
|
| Diet |
|
| Surgical intervention | For diseases that cannot be treated conservatively or carry a risk of complications. |
The effectiveness of diagnosing diseases of the human gastrointestinal tract directly depends on a correct understanding of its anatomy.