The text is presented for informational purposes only. We strongly urge you not to self-medicate. When the first symptoms appear, consult a doctor. We recommend reading: “Why you can’t self-medicate?”
The rectum (Latin - rectum, Greek - proktos) is the terminal section of the large intestine, which serves for the formation, accumulation and further removal of feces. The average length of the rectum is 13-16 cm. Its diameter varies throughout, and in the widest part it reaches 16 mm.
Location
The rectum is a natural continuation of the sigmoid colon, and originates at the level of the upper edge of the second sacral vertebra. Most of it is located in the pelvis and only a small part (anal canal) belongs to the perineum.
Medical products (drugs, medicines, vitamins, dietary supplements) are mentioned for informational purposes only. We strongly do not recommend using them without a doctor's prescription. We recommend reading: “Why can’t you take medications without a doctor’s prescription?”
In front, the rectum borders on the bladder, seminal vesicles, prostate in men, and on the posterior wall of the cervix and vagina in women. The sacrum and coccyx are located at the back; the space between the intestinal wall and the periosteum is filled with a fatty layer. On the sides there are the ischiorectal fossae, in which the iliac vessels and ureters pass.
In the sagittal plane, the rectum has an S-shape, and seems to follow the course of the sacrum and coccyx. The upper bend is facing backward and corresponds to the concavity of the sacrum; subsequently, the direction of the intestine changes to the opposite, and a second bend is formed at the coccyx, convexly facing forward. Next, the intestine goes back and down, continuing into the anal canal, and ends with the anus.
Anesthesia and pain relief after surgery
The vast majority of surgical interventions for rectal fistulas are performed under subarachnoid or, as it is also called, spinal anesthesia. It refers to regional anesthesia methods that block the transmission of nerve impulses in a specific part of the body. A distinctive feature of any method of regional anesthesia is the minimum number of complications, in particular from the cardiovascular system, respiratory system, and brain. At the same time, you are conscious or, at your request, are in a superficial medicated sleep (sedation).
In the case of subarachnoid anesthesia during perineal surgery, the blockade of the nerve impulse occurs at the lumbosacral level. In our clinic, anesthesiologists and resuscitators prefer to perform a “saddle” block, which provides ideal anesthesia of the perineum with virtually no motor block, i.e. with preservation of motor function. If necessary, anesthesia can be supplemented with intravenous sedation. All this ensures maximum comfort for the patient and ideal working conditions for the surgeon.
If you are constantly taking a number of medications, for example, antihypertensives, those that affect blood clotting, or others, be sure to inform your anesthesiologist-resuscitator about this a few days before surgery.
Surgical interventions on the perineum can also be performed under general anesthesia.
After the operation, you will be prescribed pain relief as planned for several days, which can be easily done at home using tablets. These include local anesthetic drugs, intravenous analgesics and, in case of severe pain, potent drugs.
Structure
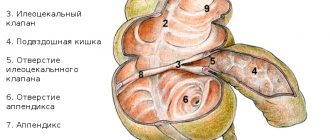
Sections of the rectum
The rectum has 3 sections:
- Rectosigmoid (supraampullary);
- Ampulla - upper ampullary, middle ampullary, lower ampullary sections;
- Anal canal.
The rectosigmoid section is a small area that represents the transition zone between the sigmoid colon and the ampulla of the rectum. Its length is 2-3 cm and its diameter is about 4 cm. At this level, the peritoneum covers the intestine on all sides, forming a short triangular mesentery, which then quickly disappears. Muscle fibers, unlike the overlying sections, are distributed evenly around the circumference, and are not collected in ribbons. The direction of the blood vessels also changes from transverse to longitudinal.
Be sure to read:
Details about the intestines: structure, sections and functions of the organ
The ampulla is the longest and widest part of the rectum. Its length is 8-10 cm, and its diameter in a healthy person is about 8-16 cm; with a decrease in tone it can reach 40 cm.
In the upper ampullary section, the peritoneum covers the intestine on three sides - in front and on the sides, downwards the peritoneal cover gradually disappears, passing to the uterus (in women) or the bladder (in men), as well as on the side walls of the pelvis. Thus, the lower parts of the rectum are located extraperitoneally, covered by the peritoneum only a small section of the anterior wall of the intestine.
The anal canal is a transition zone between the intestine itself and the anus. The canal is about 2-3 cm long and is surrounded by muscle sphincters. In the normal state, due to the tonic contraction of the internal sphincter, the anal canal is tightly closed.
The structure of the rectal wall
- Mucous membrane.
The internal lining in the upper sections is represented by single-layer transitional epithelium, in the lower sections – multilayered squamous epithelium. The mucous membrane forms 3-7 transverse folds that have a helical motion, as well as numerous unstable longitudinal folds that smooth out easily. In the anal canal there are 8-10 permanent longitudinal folds - the columns of Morgagni, between which depressions are formed - the anal sinuses.
- Submucosal layer.
The submucosa in the rectum is highly developed, which ensures the mobility of the mucosa and promotes the formation of folds. Vessels and nerves pass through the submucosal layer.
- Muscular membrane.
The muscular layer has 2 layers: circular (inside) and longitudinal (outside).
In the upper part of the anal canal, the circular layer thickens sharply and forms the internal sphincter. Outside of it and somewhat distally is the external sphincter, formed by striated muscle fibers.
The longitudinal muscles are distributed evenly in the walls of the intestine and below are intertwined with the external sphincter and the levator ani muscle.
What is the likelihood of the disease returning?
The risk of disease relapse with complex, high fistulas is slightly higher than with simple intrasphincteric fistulas and depends on the type of fistula, its location, and the presence of previous surgical interventions. Treatment of recurrent fistulas is a particularly difficult task for a coloproctologist. Previous operations on the anal canal create gross cicatricial deformities, changing the anatomy and significantly impairing the function of retention, and a long course of the disease or inadequate previous treatment can lead to the formation of additional streaks and passages. In such conditions, planning of surgical intervention should be carried out after a full examination.
The success of the upcoming surgical intervention largely depends on a comprehensive assessment of the available data using various diagnostic methods and a mandatory conversation with the surgeon. An important factor is also the implementation of surgical intervention in a specialized hospital, where this type of treatment is based on world research data, their own many years of experience and is carried out by specialists who have successfully completed training and courses to improve their skills in treating this disease.
Important! The skill of a coloproctologist is judged all over the world by the ability to correctly operate anorectal fistulas, since since the existence of proctology, the treatment of fistulas has been and is now perhaps the most difficult section of diseases of the anorectal zone!
Functions
The rectum performs the following functions:
- Reservoir and evacuation. The rectum serves as a reservoir for the accumulation of feces. Stretching of the rectal ampulla with feces and gases causes irritation of the interoreceptors located in its wall. From the receptors, impulses travel through sensory nerve fibers to the brain, and then through motor pathways are transmitted to the muscles of the pelvic floor, abdominal muscles and smooth muscles of the rectum, causing their contraction. The sphincters, on the contrary, relax, due to which the intestines are released from the contents.
- Hold function. In the passive state, the internal sphincter is contracted and the anal canal is closed, so that the contents are retained inside the intestine. After the urge to defecate occurs, the smooth muscles of the intestine contract and the internal sphincter relaxes involuntarily. The external sphincter is voluntary, that is, its contraction is subject to volitional effort. Thus, a person can independently regulate the process of defecation.
- Absorption of substances. In the rectum, water, alcohol and some other substances, including medicinal ones, are absorbed. The absorption function is important in medicine, allowing the use of rectal forms of drugs.
Be sure to read:
Gastroenterocolitis: symptoms and treatment methods (diet, medications)
What complications can there be after surgery?
Currently, with the availability of standardized technology and an integrated approach to the diagnosis and treatment of rectal fistulas, unpleasant consequences are minimized. However, it should be noted that the risk of complications always exists.
The most serious complication after surgery for rectal fistulas is the development of anal incontinence. The risk of its occurrence is especially high during repeated interventions, when the anatomy is significantly changed and the holding function may be initially compromised. It is worth noting that when operations are performed by an experienced specialist who performs this type of intervention on an ongoing basis, the risk of incontinence is practically absent.
In addition, bleeding may develop both in the early postoperative period and several days after surgery. The nature and severity of the complication are determined only after examination. Stopping bleeding is usually possible in a dressing room. In some cases, repeat surgery may be required.
In addition, when treating complex and recurrent fistulas, due to pronounced scar changes, the sutures fixing the mucomuscular flap may diverge, which leads to inflammation in the wound and requires repeated interventions.
Methods for examining the rectum
- Finger examination
Digital examination is a mandatory method of examining the rectum, which is carried out before any other instrumental method. Before starting a digital examination, the abdomen is palpated, women undergo a gynecological examination, and the condition of the perianal area is assessed.
To conduct the examination, the patient takes a knee-elbow position, the doctor treats a gloved finger with Vaseline and inserts it into the anus. Depending on the purpose of the study and the expected pathology, the patient's position may change.
This examination allows you to assess the tone of the sphincter, the condition of the mucous membrane of the rectum, perirectal tissue and the lymph nodes located in it. In men, digital examination can be used to assess the condition of the prostate gland.
- Sigmoidoscopy
Sigmoidoscopy allows you to visually assess the condition of the rectal and partially sigmoid mucosa, its color, the severity of the vascular pattern, the presence of various defects and neoplasms, determine the width of the intestinal lumen at its different levels, folding, mobility of the mucous layer, and identify the source of bleeding. The examination is carried out using a special device - a sigmoidoscope.
- Anoscopy
This method resembles sigmoidoscopy, but is more specialized and is used for targeted examination of the anal canal. Anoscopy is not very informative in diagnosing diseases of the rectal and sigmoid intestines.
- Colonoscopy
A high-tech method using a device based on flexible optical fiber, which allows you to examine the entire large intestine.
Thanks to the high resolution of the equipment, colonoscopy allows you to detect diseases at the earliest stages, perform multiple biopsies, and remove polyps.
- Irrigoscopy
X-ray examination method. To carry it out, a contrast agent is injected into the rectum using an enema, and then X-rays are taken. Indications for this method are neoplasms of the large intestine.
- Ultrasound of the rectum
The study is carried out with a special rectal sensor and allows you to assess the condition of the intestinal wall, its thickness, and clarify the size of pathological foci.
- Sphincterometry and profilometry
Be sure to read:
Details about intestinal colonoscopy: preparation and procedure
These methods are intended to assess the closing ability of the anal sphincter.
- CT scan
Allows you to visualize rectal tumors that are not visible with other research methods.
Treatment of complex fistulas should be divided into 2 stages
At the first stage, a drainage ligature is installed into the fistula tract - a thin, almost invisible suture material (Fig. 7). The main goals of this stage of treatment are: the formation of a direct fistula tract around the ligature, drainage of possible leaks, reduction of the inflammatory process, prevention of self-closure of the external opening for constant drainage of inflammatory and/or purulent discharge.
Figure 7. Drainage ligature
At the second stage, after the acute inflammation subsides (4-6 weeks), the main surgical treatment is performed - excision of the fistula.
Important! Two-stage surgical treatment provides conditions under which radical surgery becomes possible with minimal complications.
Currently, in the treatment of rectal fistulas, various biological materials based on connective tissue (Permacol), fibrin glue, and collagen paste are widely used, which are introduced into the fistula tract, tamponing it. These methods have a lesser effect on the rectal closure apparatus; their use does not lead to the formation of a massive wound defect. However, the rate of disease recurrence is significantly higher than radical surgery.
Promising modern methods for treating fistulas are endoscopic (VAAFT) and laser (FiLaC) technologies for removal of affected tissue. These technologies practically eliminate the possibility of damage to the sphincter apparatus, however, today, the effectiveness in leading clinics in the world does not exceed 50-60%.
How does diverticular disease manifest?
Uncomplicated diverticulosis is characterized by an asymptomatic course - you may not even notice the disease. Diverticula may be an incidental finding during routine examination. In this situation, no special treatment is required. Recommendations include regular medical supervision, a diet high in fiber and low in refined carbohydrates, as well as regular physical activity and weight management.
The difficulty of timely detection of diverticular disease lies in the absence of specific symptoms. The clinical picture consists mainly of cramping pain, predominantly in the left lower abdomen, increased gas formation, unstable stools with a tendency to constipation or alternating constipation and diarrhea. Such complaints are mainly associated with disorders of colon motility.
When visiting a doctor, such patients are usually diagnosed with “irritable bowel syndrome” or “dolichosigma”, the patient is reassured, recommended to perform an ultrasound examination of the abdominal cavity and, after prescribing light therapy, is sent “home”.
However, in case of such complaints, a colonoscopy is mandatory! The above symptoms can be manifestations not only of diverticular disease, but also of many other diseases of the colon, the timely detection of which can significantly improve treatment results.
Figure 3. Colonoscopy. The orifices of the diverticula are visible
The clinical picture of diverticulitis varies significantly. Severe abdominal pain, bloating, lack of stool, may be accompanied by fever, nausea, and vomiting. Such complaints require urgent hospitalization in the coloproctology department, where patients receive antibacterial, anti-inflammatory therapy, and if this treatment is insufficiently effective, surgical intervention may be necessary.
The main cause of inflammation of a diverticulum - diverticulitis - is the ingress of dense feces into it, which are unable to come back out. At this stage, inflammatory changes and the formation of infiltration (compaction) of surrounding tissues occur.
Arterial and venous systems of the anal canal
The blood supply to the rectum is carried out by five arteries (Table 3):
- unpaired superior rectal artery;
- paired middle rectal artery;
- paired inferior rectal artery.
| Artery name | Originate from | Take part in education |
| Superior rectal artery | Inferior mesenteric artery | Internal hemorrhoidal plexuses |
| Left and right middle rectal arteries | Internal iliac or internal pudendal artery | |
| Left and right inferior rectal arteries | Internal pudendal arteries | External hemorrhoidal plexuses |
| Table 3. Arterial blood supply to the anal canal |
The final branches of the afferent arteries are intramural arteries, which have a cochlear shape and are called cochlear arteries.
The venous network of the rectum consists of three plexuses (Table 4):
- submucosal venous plexus;
- subfascial venous plexus;
- subcutaneous venous plexus.
| Name | Form | Take part in education |
| Submucosal venous plexus | Superior and middle hemorrhoidal veins | Internal hemorrhoidal plexuses |
| Subfascial venous plexus | ||
| Subcutaneous venous plexus | Inferior hemorrhoidal veins | External hemorrhoidal plexuses |
| Table 4. Structure of the venous system of the anal canal |
The initial branches of the submucosal and subcutaneous plexuses are the cavernous veins, the walls of which consist of pronounced areas of connective tissue and muscle fibers. Thanks to this structure, these veins have the ability to significantly stretch and fill with blood, which ensures a tight closure of the anal canal. After this, the cavernous veins also quickly contract to evacuate blood from their lumen.