“THE SITE IS UNDER RECONSTRUCTION WE APOLOGIZE FOR THE TEMPORARY INCONVENIENCE”
Familial adenomatosis (diffuse polyposis)- a hereditary disease of the colon, the manifestation of which is the presence of multiple up to several thousand polyps (adenomas) (formations of the colon mucosa), in most cases detected as an accidental finding during colonoscopy or sigmoidoscopy. This disease requires constant monitoring by specialists, since polyps have a tendency to grow progressively and inevitably become malignant if not treated in a timely manner.
Cause and mechanism of development:
Linkage analysis carried out back in 1986-87 in families with FAP led to the mapping of the APC gene (OMIM 611731) on chromosome 5 in the 5q22 region. The largest proportion of cases of familial adenomatous polyposis of the colon are associated with mutations in this gene. Mutations in the APC gene lead to an almost 100% risk of developing the disease. It is known that the manifestations of familial adenomatous polyposis in different families differ in the severity of the disease, the prevalence of the process and the age of onset of the disease. Studying hereditary variants of the APC gene structure in connection with the genetic and clinical characteristics of FAP may provide new information about the mutation-clinical manifestation relationship, which may play an important role in the treatment of the disease.
However, not all patients with familial adenomatous polyposis have hereditary mutations in the APC gene. In 2002, another gene was mapped, mutations in which can also cause familial adenomatosis of the colon. This is the MYH gene located on chromosome 1p34 (OMIM 604933) [Al-Tassan 2002]. At the birth of a child, signs of the disease do not appear; later, as the body grows, at the age of 6-7 years, the appearance of small polyps on the mucous membrane of the colon can already be detected.
Clinical manifestations:
As a rule, symptoms of the disease most often appear during puberty, at the age of 15-19 years; at an early age there are no severe symptoms.
The most common and constant symptom is frequent stools up to 5-6 times a day mixed with blood and mucus. Bloody discharge from the anus is usually an admixture of liquid, semi-formed feces. Abdominal pain can have varying intensity and localization. Symptoms of the disease such as fatigue, weakness, and anemia most often begin to appear by the age of 20. For most patients, this coincides with an increase in workload: the beginning of work, military service, and for women, pregnancy and childbirth. With the development of cancer from polyps, the general condition of patients worsens, and new symptoms characteristic of the oncological process appear.
The most likely detection of the disease in patient groups:
- having clinical signs of polyposis: frequent stools mixed with blood and mucus since childhood, abdominal pain, anemia, etc.;
- relatives of patients with familial adenomatosis (children, parents, brothers, sisters, including cousins).
Diagnostics:
An endoscopic examination of the colon (colonoscopy) with multiple biopsies (sampling of pieces of tissue for histological examination) is required. An examination of the upper gastrointestinal tract is mandatory for a patient with familial adenomatosis. More than half of the patients have pathological changes in the stomach: gastritis, polyps, and sometimes malignant tumors.
The presence of polyps in the colon may be accompanied by formations in other organs and tissues: sebaceous gland cysts ( Alfield syndrome
), malignant formations of the central nervous system (brain) (
Turcot syndrome
), tumors of the endocrine glands (
Solinger-Ellison syndrome
), pigmentation of the mucous membrane and skin (
Peutz-Jeghers syndrome
), while the polyps have a different structure (hamartomas).
Treatment:
Currently, the only treatment for familial adenomatosis of the colon is surgical. The principle of surgical treatment of familial adenomatosis is to remove all parts of the colon where there are polyps, because sooner or later they develop into a cancerous tumor.
Forecast:
If a patient with familial adenomatosis of the colon is not treated, the development of cancer from one or more polyps is inevitable. Performing sphincter-preserving operations is possible in 85% of patients who applied before the polyps become malignant; with the development of cancer, such operations are possible only in 30% of patients.
Types of adenomatous rectal polyps
By the age of sixty, approximately 50% of people on Earth have at least one adenomatous rectal polyp with a diameter of one centimeter or more. Multiple adenomatous polyps in most cases lead to adenomatous polyposis. Proctologists distinguish three types of adenomatous rectal polyps:
- Tubular adenomas are the most common neoplasms from the class of adenomatous polyps. They can be found anywhere in the rectum. Compared to the other two types of rectal polyps, they are least likely to develop into cancer;
- Tubular-villous adenomas of the rectum often degenerate into a cancerous tumor;
- Villous adenomas are polypous neoplasms that are most often found on the surface of the rectum. They are usually larger in size than other types of adenomatous polyps. These neoplasms do not have legs and resemble cauliflower in appearance. Their surface is velvety. This type of adenomatous polyp is associated with the highest incidence of rectal cancer and mortality from malignant rectal tumor. Villous adenomas sometimes cause hypersecretion syndrome. It is characterized by a decrease in the level of potassium in the blood plasma and copious mucus secretion.
The risk of an adenomatous rectal polyp progressing to cancer increases if the polyp is larger than one centimeter in size and contains a high percentage of villous component. The form of adenomatous polyps of the rectum is also associated with the risk of developing into cancer. Most pedunculated polyps are smaller in size than sessile polyps. The latter have a shorter path for migration of atypical cells from the tumor to the submucosa and more distant structures. If the size of wide-based adenomatous rectal polyps is more than two centimeters, then they mostly already contain villous elements, have a high malignant potential and a tendency to re-form after colonoscopic polypectomy.
Although tubular adenomatous rectal polyps are not as dangerous as villous and tubulovillous adenomas, they can become cancerous when they grow large. Larger tubular adenomatous rectal polyps have an increased risk of malignant transformation because they form more villous components and can become sessile polyps.
Symptoms and diagnosis of adenomatous polyps
At the onset of the disease, rectal polyps do not manifest clinical symptoms. Adenomatous polyps of the rectum during their growth can cause intestinal bleeding, which proctologists detect using a special test. People over the age of 50 are recommended to undergo a sigmoidoscopy procedure once every 3-5 years using a flexible instrument to identify any abnormal growths that may be an adenomatous polyp.
If adenomatous polyps are found during this procedure, the patient will also have to undergo a colonoscopy procedure. Proctologists recommend this procedure as an important part of the examination for the early detection of colon cancer, since adenomatous polyps can be found in any part of the large intestine. As methods for removing an adenomatous polyp of the rectum identified during colonoscopy, a loop or cauterization is used. Doctors at the proctology department prefer colonoscopy to sigmoidoscopy for the reason that the first procedure allows you to examine the entire cavity of the colon. This is very important because more than half of colon polyps are located in the upper part of the colon, which is inaccessible to sigmoidoscopy.
Adenomatous polyps of the rectum are also detected in the absence of symptoms of the disease during screening examinations or when the study is carried out for other reasons (gastrointestinal bleeding), endoscopic examination (sigmoidoscopy or colonoscopy) or x-ray method (irrigoscopy).
If small polyps (less than 1 cm) are detected during sigmoidoscopy, a biopsy is performed followed by a morphological examination. If the polyp is larger than 1 cm, a biopsy is usually not required, as the patient will need a colonoscopic polypectomy. If the histological structure of the polyp detected during sigmoidoscopy corresponds to an adenoma, the patient needs a colonoscopy.
Functions of the colon
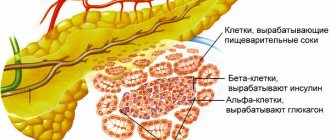
The colon produces:
In the colon, water, electrolytes (calcium, potassium, sodium, magnesium salts, etc.), glucose, fatty acids, amino acids, fat-soluble vitamins, etc. are absorbed. Enzymes, cholesterol, heavy metal salts are released into the intestinal lumen, and fiber fermentation occurs. . Intestinal microflora plays an important role in fermentation. The gut contains more than 400 different aerobic and anaerobic microorganisms. Anaerobes predominate, in a ratio of 1:1000. Normal intestinal flora has enzymatic, vitamin-synthesizing (vitamins B, C, K) and protective properties. Anomalies and malformations
|
Polyps and polyposis
Polyps are classified as benign neoplasms arising from epithelial cells of the colon; some of them are prone to malignancy (malignant degeneration). Polyps are found in 10-12% of proctological patients. When performing preventive colonoscopy, it is 2-4%. In men, polyps are found 2-3 times more often than in women. Polyps can be single or multiple. The diameter ranges from 0.5 to 2 cm, sometimes they reach 3-5 cm. Polyps with a “leg” hang into the intestinal lumen; polyps with a broad base are less common. There are juvenile, hyperplastic, adenomatous (glandular), villous polyps, villous tumors, as well as multiple colon polyposis (true and secondary).
Juvenile polyps
They are observed mainly in children. The mucous membrane of the rectum is most often affected. Macroscopically, polyps have the appearance of a bunch of grapes, their surface is smooth, the color is more intense compared to the surrounding unchanged mucous membrane. These are typical glandular-cystic formations in which the stroma predominates over the glandular elements. As a rule, juvenile polyps do not become malignant.
Hyperplastic (metaplastic) polyps
Small (2-4 mm) formations, most often have a cone shape. They retain the normal structure of the intestinal mucosa with a significant increase in the number of glands, due to which the impression is created of a thickening of the mucous membrane in the form of a polyp. They become malignant very rarely.
Adenomatous (glandular) polyps
Observed in 90%. An adenomatous polyp has the appearance of a tumor with a smooth surface, round in shape, located on a stalk with a wide base, and is an area of hyperplasia of the mucous membrane. With a size of more than 2 cm, malignancy of the polyp occurs in 50% of cases.
Villous polyp (adenopapilloma)
Occurs in 5% of cases of detection of polyps - it has a lobed structure, a velvety surface, and is covered with thin delicate villi. The villous tumor protrudes into the intestinal lumen and is located on a broad base (nodular form). One of the varieties of villous tumors is the creeping, carpet form, in which there is no tumor node. The process spreads over the surface of the mucous membrane, occupying a fairly large area around the entire circumference of the intestine, and manifests itself as villous or finely lobulated growths. The size of villous tumors is 1.5-5 cm. The tendency to malignancy is up to 90%. Most often, villous tumors are localized in the rectum and sigmoid colon. The clinical picture is characterized by the release of mucus during bowel movements, the amount of which can reach 1 - 1.5 liters per day, which leads to water and electrolyte disorders. Slight vulnerability of the tumor villi leads to bleeding. Abdominal pain, constipation, diarrhea, and intestinal discomfort are noted.
Colon polyposis (multiple polyps)
It can be congenital, familial or secondary (as a result of other lesions of the colon, such as colitis). The incidence of malignancy reaches 70% and higher. Polyposis can be considered an obligate (obligatory) precancer. Congenital familial polyposis is inherited, affecting several family members. The disease is usually detected in children and young people. Polyps can be localized throughout the gastrointestinal tract. The combination of multiple colon polyposis with benign tumors of soft tissues and bones is called Gardner's syndrome. The combination of polyposis of the digestive tract with pigment spots on the mucous membrane of the cheeks, around the mouth and on the skin of the palms is called Peutz-Touraine syndrome. Multiple colon polyposis is characterized by abdominal pain without clear localization, diarrhea, discharge of blood and mucus in feces, weight loss, and anemia. Diagnosis of the disease is carried out on the basis of clinical symptoms, anamnestic data and instrumental examination data. The main treatment for colon polyps is surgical removal of the polyp or part of the colon. The volume is determined on the basis of anamnesis, instrumental examination data and the results of histological examination.
Diagnostic measures at PATERO CLINIC:
- Consultation with a surgeon-proctologist.
- Video endoscopic examination.
- in the absence of indications, the first examination is at 45 years of age,
- in the absence of pathology - colonoscopy every three years,
- if pathology is present, treatment is carried out, then colonoscopy every year.
- If you refuse a colonoscopy, perform a virtual colonoscopy (CT colonoscopy)
- Histological examination of the biopsy specimen in the laboratory of PATERO CLINIC.
- If necessary, ultrasound, MSCT, MRI, laboratory diagnostics.