The kidneys are a paired excretory organ in which the processes of filtration, reabsorption and primary excretion of urine occur. Its most important structural element is, of course, the kidney parenchyma - what it is, how it is structured, and what its characteristics are considered normal we will discuss in our review and video in this article.
How does our main excretory organ work?
Structure
Parenchyma is a Greek word that combines the totality of the functioning elements of an internal organ. In other words, this is a part of it that performs specific functions.
This is where urine is formed
Renal parenchyma is the tissue in which nephrons, the main functional units of the kidneys, are localized.
It consists of two layers, with no clear boundary between them:
- cortical, located closer to the outer shell;
- cerebral, internal.
The main part of nephrons is located in the cortex. There are about 1,000,000 of them in total, but no more than a third of them function in a healthy person.
This is such a complex structure
This is interesting. Considering that the kidneys filter and purify about 1,700 liters of blood every day, you can understand how difficult and stressful their job is.
The structure of nephrons in the kidney parenchyma is quite complex. Each of them consists of a glomerulus and a system of tubules. The glomerulus is located in the outer (cortical) layer, and the descending ends of the tubules descend into the medulla, forming the renal pyramids.
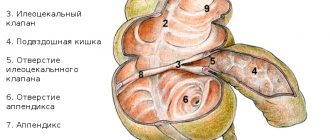
The latter open into small calyces, of which there are from 8 to 10 in each kidney. Then they enlarge, forming 3-4 large cups, and they, in turn, flow into the renal pelvis.
Typical liver changes
By conducting a study, a specialist will be able to identify the main typical changes in the parenchyma:
- change of size;
- increased echogenicity;
- changing the clarity of the contour;
- change in the pattern of blood vessels;
- violation of the homogeneity of the structure;
- focal, local or diffuse changes in liver tissue.
Sometimes even an experienced diagnostician will not give you a completely complete picture of the condition of your organs. Minor changes can hide severe pathology. And sometimes the changes are associated with previous illnesses. For a complete clinical picture, it is necessary to undergo a comprehensive examination, an MRI, and a urine and blood test.
Changes in the parenchyma are quite dangerous and lead to diseases such as cirrhosis, hepatitis, and sclerosing cholangitis.
Functions performed
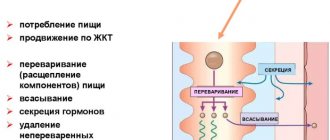
The structure of the kidney parenchyma described above ensures the following functions:
- excretory (excretory);
- concentration;
- homeostatic (ion-regulating, osmoregulating);
- endocrine;
- metabolic.
First of all, the excretory function of the organ should be noted. A large volume of blood is pumped through the kidneys every minute. Primary urine containing a large amount of liquid is formed in the glomeruli.
Then several liters of primary urine enter the tubules, where the processes of reabsorption (reabsorption) and concentration occur. The resulting secondary urine passes through the pyramids, small and large cups, pelvis and, finally, is excreted from the kidneys through the ureters into the bladder.
The photo shows the process of urine formation
This is interesting. In addition to excreting urine and maintaining a constant internal environment, the kidneys can be called a hormone-producing organ. The fact is that they produce renin, which controls blood volume, as well as erythrooetin, a stimulator of hematopoiesis.
How is the kidney parenchyma structured?
The parenchyma has two main layers - the cortex, which is located outside the kidney, and the medulla, which is internal. There is no clear boundary between them.
The main part of the functional units is located in the cortical layer. In total, there are about a million of them, but only one third of the nephrons take part in the work.
Each nephron has a rather complex structure - a glomerulus and tubules. The glomerulus is localized in the outer layer, and the system of tubules extends into the medulla and forms a pyramid, at the end of which there is a papilla. It exists to carry urine into the calyxes.
First, primary urine is formed, which differs in composition from that which comes out. It contains a lot of fluid and microelements that the body needs.
Several liters of primary urine are reabsorbed. At this moment, some of the water and nutrients are returned to the blood at the same time. After this, secondary urine passes through the underlying pathways and is excreted.
Such a system exists in order to constantly maintain the balance of the water and electrolyte composition of the blood and regulate blood pressure.
Some of the nephrons that are localized between the first and second layers secrete renin (an important factor in the regulation of blood pressure) and erythropoietin (necessary for hematopoiesis).
The total thickness of the parenchyma in humans changes throughout life. In young people it is about 1.5-2 centimeters, but by the age of 60 it decreases to 1 centimeter.
Symptoms
If the filtration and excretory functions of an organ are disrupted, this means that pathology of the organ tissue develops. Signs of diffuse disorders can either develop rapidly or increase gradually. For the most part, the following symptoms may indicate this:
- increased body temperature, especially in acute infectious pathologies of the kidneys;
- change in skin color, it acquires a yellowish tint and becomes dry;
- weakness, fatigue, possible headaches;
- impaired urination and changes in urine volume, which may decrease or increase;
- the presence of cutting and burning sensation when emptying the bladder;
- the formation of edema in the face; in certain cases, the arms and legs may swell;
- increased blood pressure, shortness of breath;
- lower back pain, both acute and aching in nature.
If kidney problems are diagnosed during a laboratory test, the urine is diagnosed by a change in its color; most often it is cloudy and dark, with pus or blood appearing in it. Also, decreased echogenicity may indicate fluid accumulation or tumor formation.
Research methods
The structure and internal structure of the kidney parenchyma is determined quite easily.
To do this, you need to pass one or more instrumental tests:
- Ultrasound;
- computed tomography;
- MRI.
Ultrasound is the easiest way to “look” inside the human body
With the help of these modern diagnostic methods, the parenchyma of the right kidney, as well as the left, is well visualized.
Standard instructions instruct the doctor to evaluate the following parameters:
- anatomical structure;
- internal structure;
- parenchyma thickness;
- density;
- absence/presence of pathological changes.
Ultrasound results in adult women and men
Diagnosis of kidney condition does not differ between people of different genders. The norms of indicators are the same for both men and women. The normal size of a woman's kidneys is different during pregnancy. The norm is considered to be lengthening of the organ up to 2 cm; slight expansion is allowed along with the pelvis and ureters. The norm for adults when deciphering the results is as follows: thickness - 40-50 mm, length 100-120 mm, width 50-60 mm, thickness of the functional part - 15-25 mm. The sizes of the right and left kidneys differ, but not more than 2 cm. The normal ultrasound scan of the kidneys in an adult is determined by the height indicator. Using the table below, you can determine the normal size of the kidneys relative to a person's height.
To maintain normal functioning, the body needs to carry out metabolism. In order for the body to receive everything it needs from the environment, there must be a continuous cycle between the person and the external environment.
During metabolic processes, metabolic products are formed in our body, which must be excreted from the body. This includes urea, carbon dioxide, ammonia, etc.
Substances and excess water are removed, as well as mineral salts, organic substances and toxins that enter the body with food or other routes.
The elimination process occurs through the excretory system, namely the kidneys.
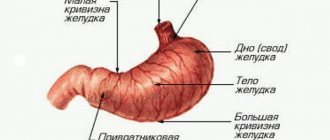
The kidney is a paired parenchymal organ, bean-shaped . The kidneys are located in the abdominal cavity, in the lumbar region, retroperitoneally.
Normal kidney values:
- length 10-12 cm,
- width – 5-6 cm,
- thickness from 3 to 4 cm;
- the weight of one kidney is 150-200 g.
The structure of the kidney also includes the main tissue - parenchyma .
Kidney cyst - symptoms and treatment
A simple renal cyst is a single benign fluid formation that is one of the most common urological diseases.
Simple renal cyst occurs in 10% of people in the general population [4]. Due to the widespread use of modern medical imaging methods (ultrasound, MRI, MSCT), the frequency of detection of this pathology is increasing every year [1][2][3][8].
The kidney is one of the most common places for the formation of cysts, and the urinary system of our body ranks first in the number of development of various anomalies [1][2][3]. Cystic lesions are the most common type of renal structure abnormality, and simple cysts are the most common type of cystic lesion. Simple kidney cysts are more often diagnosed in men; the frequency of their occurrence increases with age. Renal cysts (single or multiple) are observed in 50% of people over 50 years of age [4][8].
A congenital simple renal cyst occurs as a result of an abnormal development of the renal tubules, which lose communication with the urinary tract. The hereditary mechanisms responsible for the formation of kidney cysts during intrauterine development of the fetus remain unclear. A congenital simple renal cyst can appear either as a result of the inheritance of certain genes (genetic diseases) or due to a mutation during embryo development (in the period from 32 to 50 days from the moment of conception). These mechanisms are not mutually exclusive and in some cases may work together.
In addition to simple renal cysts, there are many different congenital cystic kidney anomalies: polycystic, multicystic, solitary cyst, multilocular cyst, spongy kidney, calyceal diverticulum in the upper pole of the kidney. These diseases differ not only in the type of inheritance, but also in the clinical and pathomorphological picture. Diseases such as polycystic disease (polycystic disease) and multicystic disease have significant differences from simple cysts. For example, a multicystic kidney is formed when embryogenesis is disrupted at 4-6 weeks and is characterized by total replacement of the renal parenchyma with cysts of different sizes [15].
In the embryonic period, dermoid cysts can also form in the kidneys, which are sometimes similar to congenital simple cysts. A renal dermoid cyst is a cavity formation of germinal tissue. This is a very rare pathology that is formed as a result of a chromosomal malfunction and disruption of normal cellular differentiation and development of the embryo. Unlike a simple cyst, they contain the rudiments of adipose tissue, teeth, hair, etc. Dermoid cysts should cause serious oncological suspicion among both doctors and patients. In 5-8% of cases, malignancy (cancerous degeneration) of the dermoid cyst occurs. Some of its cells can eventually turn into a source of tumor growth. This happens under the influence of internal or external irritating factors. Such cysts require surgical treatment [1][2][3][6].
An acquired renal cyst can be the outcome of various diseases occurring in the kidneys, such as urolithiasis, chronic pyelonephritis, various kidney tumors [1][2][3][6]. One of the reasons for the formation of kidney cysts may be damage to the organ by parasites (echinococcus, alveococcus). For example, hydatid cysts of the kidney (caused by Echinococcus granulosus) occur in 2-3% of all kidney cysts. The larva of echinococcus is carried by the bloodstream into the kidney from the liver, so first of all it is necessary to exclude the presence of a large parasitic formation in the liver.
Multiple kidney cysts occur in patients who suffer from chronic kidney disease and have been on hemodialysis for many years. It is known that kidney cysts occur in 50% of patients undergoing dialysis for more than 10 years. At risk are patients with a transplanted kidney, end-stage chronic renal failure, Hippel-Lindau disease (a rare genetic disease characterized by the development of various tumors and cysts in the central nervous system and other internal organs) [1][2][3][ 6][12]. Also, numerous other reasons contributing to the formation of kidney cysts include: hereditary predisposition, previous diseases, traumatic kidney damage, frequent hypothermia [1][2][3][6][12].
Main indicators of parenchyma: norm and pathology
Thickness
The normal thickness of the kidney parenchyma is 15-25 mm. In elderly patients over 60 years of age, this figure is slightly lower - about 11 mm. If it deviates either upward or downward, it is necessary to promptly establish the cause.
To understand, you need to remember the anatomy
Table: Reasons for deviation from the norm:
| Thickening of the renal parenchyma | Thinning of the kidney parenchyma |
| Acute inflammatory processes (for example, with glomerulonephritis) | Chronic glomerulonephritis |
| Acute nephrotic syndrome | Infectious diseases |
| surge arrester | Chronic inflammatory lesions of the parenchyma |
| Cysts | Neoplasms originating from epithelial tissue |
| Tumors and other neoplasms originating from parenchymal tissue | Hydronephrosis |
| Compensatory (vicarious) kidney hypertrophy |
If we compare all parenchymal dystrophies, the most common is a decrease in the kidney parenchyma. This condition is fraught with a decrease in the number of functioning nephrons and the development of renal failure. The final stage of the pathological process is parenchymal atrophy.
Structure
When a patient undergoes an ultrasound of the kidneys, he may often find in the conclusion an indication that the echostructure of the parenchyma is changed. What does it mean?
Normally, the structure of the organ tissue is homogeneous, without pathological inclusions. With any disease, diffuse or focal changes can be observed.
This is what healthy kidneys look like on an ultrasound
Uniformly heterogeneous renal parenchyma is observed with:
- development of urolithiasis;
- inflammatory, including autoimmune diseases;
- some endocrine diseases - diabetes mellitus, hyperthyroidism;
- atherosclerosis of renal vessels.
- diffuse metabolic changes (a typical example is calcifications in the parenchyma).
Focal
Limited (focal) changes in the parenchyma are observed with:
- benign neoplasms (oncocytoma, angiomyolipoma, adenoma);
- malignant neoplasms (cancer);
- cysts.
A pathological focus can also be caused by a stone in the parenchyma.
The calculus is well visualized
Density
The echogenicity of the parenchyma is its ability to reflect or transmit ultrasonic waves.
Normal on ultrasound:
- the pyramids have low echogenicity (almost black);
- the cortex and columns are isoechoic and identical to each other (gray);
- sinuses are hyperechoic (the lightest).
Most often in medicine, increased density of the kidney parenchyma is encountered.
This may indicate development:
- diabetic nephropathy;
- chronic infectious diseases;
- consequences of arterial hypertension;
- glomerulonephritis;
- amyloidosis;
- sclerotic changes.
If the echogenicity of the renal parenchyma in the fetus is increased, this is a consequence of congenital developmental anomalies. Severe parenchymal fibrosis should alert the physician.
During pregnancy, it is very important to undergo screening ultrasound examinations
In adults, the renal parenchyma is denser more often in chronic diseases, chronic renal failure. Typically, this pathology is diagnosed in elderly patients. As a rule, parenchymal fibrosis is a consequence of the replacement of functioning nephrons with connective tissue.
Note! Ultrasound diagnostic doctors are well acquainted with so-called pseudopathologies. For example, sometimes enlarged Bertin's columns extend quite deeply beyond the parenchyma into the renal sinus. It seems that such a parenchymal bridge of the kidney literally divides the organ in two. However, this is not a tumor or pathological tissue, but simply an individual characteristic of the patient.
Parenchyma cells are an important structural element of any organ. Kidneys are no exception. Regular preventive examinations and disease prevention ensure that they remain healthy for a long time.
Parenchyma tumor
Parenchyma tumors are numerous neoplasms of various structures. It is necessary to distinguish between malignant and benign tumors. Renal cell cancer is very common, accounting for approximately 85−90% of the total number of parenchymal tumor diseases.
Benign neoplasms of the parenchyma account for about 6−8% and adenoma, angiomyolipoma and oncocytoma of the kidneys are more often observed. A feature of kidney cancer is the so-called venotropy, which is distributed in the form of a blood clot and goes through the veins into the main trunk, and then into the inferior vena cava, and sometimes reaches the atrium. This neoplasm is most often detected by ultrasound and CT.
As for the symptoms of this disease, they are diverse and are divided into extrarenal and renal. Renal signs are classic symptoms, which include hematuria, pain and a mass in the hypochondrium, which is felt on palpation.
These symptoms do not allow an accurate diagnosis to be made in a timely manner for the reason that they are observed in approximately 8% of patients and are not characteristic of an advanced process. Combinations of these symptoms can also occur in other diseases due to the fact that the kidney parenchyma is susceptible to various diseases.
Surgical intervention today remains the only method that allows one to fully or partially expect a cure and prolongation of life for a disease such as kidney cancer.
Preparation
To obtain the most reliable information, you need to pay attention to preparatory activities. Before the procedure, it is important not to eat for 6 hours. For 3 days you should avoid eating foods that cause increased gas formation. It is also not recommended to smoke, suck candy, or chew gum immediately before an ultrasound.
In addition, in order to properly prepare, you should drink at least 1 liter of clean water an hour before the procedure. Filling the bladder will help improve the ultrasound and improve the quality of the examination. During pregnancy, women can have their kidneys diagnosed by ultrasound; this procedure does not have a detrimental effect on the fragile fetus.
For your information, if the transcript indicates increased pneumatosis, then this is considered a sign of increased gas formation. This circumstance is evidence that the preparation for the procedure was poorly carried out. Ultrasound is a fairly informative method for diagnosing the condition of the renal apparatus. It allows you to identify many diseases at their initial stage of manifestation.
Leave a comment 44,663
At the moment, one of the frequently prescribed diagnostic methods that determine the condition of the kidneys is ultrasound examination. The results of a kidney ultrasound will help identify possible organ diseases or pathological manifestations. Using ultrasound, the following parameters are determined: quantity, location, contours, shape and size, structure of parenchymal tissue. It is determined whether there are neoplasms, stones, inflammation and swelling. Renal blood flow is visualized.
Indications for an ultrasound are: impaired urination, the appearance of blood in the urine, pain in the lumbar region, injuries, existing inflammatory processes, poor urinalysis.
Kidney ultrasound allows you to examine the health or progress of the organ’s disease, selecting appropriate therapy based on the data obtained.
Questions for the doctor
About kidney cyst
Hello! I am 36 years old, female, and have not been ill with anything special. Recently I decided to do an ultrasound of all organs for prevention, and during an examination of my kidneys, a cyst on the right measuring 13*17 mm was discovered. What could have provoked its formation? Is it dangerous? How to treat? Thank you.
Good day! A kidney cyst is in most cases a benign tumor formation that occurs quite often. The causes of this disease, unfortunately, have not been sufficiently studied; parenchymal cysts are usually congenital. The process of cyst formation itself is associated with overflow of the renal tubule with fluid.
The choice of treatment tactics in each case is selected by the doctor individually. Since your tumor is relatively small in size, conservative treatment or even just observation may be successful. Be sure to consult a urologist.
Why is atrophy dangerous?
Dad has had kidney problems for a long time; doctors diagnosed urolithiasis. When he was last seen, the doctor said that his condition was worsening, and the ultrasound clearly showed signs of hydronephrosis on the left. I scared that soon the kidney would stop working completely, since almost all of the “working” tissue was compressed. Is there any way to prevent this?
Hello! Hydronephrosis is a very dangerous syndrome that ultimately leads to atrophy of parenchymal tissue and the development of renal failure. In the later stages, it can be treated surgically; be sure to show your dad to a urologist to decide on the need to install a nephrostomy. Be healthy!
Diffuse changes in the renal parenchyma
These changes have no independent meaning and there may be several reasons for this. The reasons for the changes include the initial stage of urolithiasis, the formation of plaques in the area of the pyramids, which later turn into kidney stones.
These changes can also be hyperechoic inclusions, which are caused by adipose tissue or renal vessels. And in order to accurately determine the diagnosis and stage of the disease, sometimes it is necessary to conduct a comprehensive examination, which allows you to determine everything with precision.
Children's sizes
Kidney ultrasound is often performed to diagnose children. It allows you to determine the presence of congenital anomalies. Most often, the procedure is prescribed if there are complaints of pain in the lower back, lower abdomen, after injuries, or problems with urination. An examination of the newborn is carried out to exclude anomalies that are associated with heredity, in case of a difficult pregnancy, or in the serious condition of the child at the time of birth.
What is the normal parenchymal layer on the kidney?
The tissue outer membrane of the kidney is called parenchyma, which consists of the medulla and cortex. The structure of the layer is very thin, consisting of small capsules that are connected by a system of blood vessels. There are more than a million of them in the structure of the right and left kidneys, and they are responsible for the reproduction of urine. Bypassing the sinuses, which are located in the medulla of the parenchyma, the fluid enters the pelvic and calyceal sections of the kidneys.
Moderate structural changes are considered normal and develop as the human body ages. At the age of 16-18 years, the thickness of the upper layer of the kidney is 1.3-1.6 cm. After both sexes reach a certain age (16 years), the thickness of the kidney parenchyma decreases to 1-1.1 cm.
Return to contents
Kidney abnormalities
Renal anomalies include many diseases; now we will look at the thinning of the kidney parenchyma, which can be caused by a number of factors.
Most often, this occurs as a result of an infectious disease and improper treatment, resulting in a load on the entire renal system. Improper treatment and failure to comply with the necessary conditions after treatment of kidney diseases can lead to the fact that the kidney parenchyma is on the verge of depletion.
All diseases, including diseases of the genitourinary system, should be treated in a timely manner, and it is best to take preventive measures so as not to get sick at all.
Causes
Quite often, diffuse changes in the renal parenchyma occur as a result of exacerbation of pathological processes in the kidneys. But this is not the only reason for this pathology; other diseases can also provoke negative changes.
The following abnormalities in the body can provoke the disease:
- inflammation of adipose tissue;
- diabetes;
- congenital vascular pathologies;
- hyperthyroidism;
- vascular diseases that increase the echogenicity of the parenchyma;
- formation of calcifications in renal tissue;
- initial stage of development of urolithiasis;
- inflammation of the tubules and parenchyma nodules;
- fat deposits;
- accumulation of cholesterol.
All of the above reasons can provoke the development of such a deviation as renal parenchyma. If a person is diagnosed with at least one of the pathologies listed above, then it is necessary to systematically undergo examinations and be observed by a doctor in order to immediately begin treatment when the first signs indicating the development of the pathology appear.
Note! Signs indicating the disease can be pronounced, or they can be completely invisible. The presence of pathology can only be determined by ultrasound results. In order to identify pathology, it is recommended to undergo annual preventive examinations.
Among other things, the following problems can provoke diffuse changes in the kidneys:
- salt deposits that arise as a result of metabolic disorders, as well as malnutrition and pathologies of certain organs. In this case, dead kidney tissue accumulates in the parenchyma, as a result of which calcium microcrystals accumulate on the surface. To prevent this situation, it is recommended to move as much as possible and avoid systematically consuming protein foods;
- development of tumors, mostly benign tumors. But the danger in this case is that in some cases the tumor can develop into kidney cancer. With this degeneration, the patient exhibits symptoms such as chills, increased blood pressure and tissue swelling;
- thinning of the parenchyma - this problem develops if a person is diagnosed with chronic renal abnormalities. In the human body, pathogenic bacteria develop, which provoke the progression of the inflammatory process. In order to avoid this, you need to carefully monitor your health and start treatment when the first symptoms appear, otherwise the infection can lead to the death of natural filters. If the disease leads to thinning of the parenchyma, then a serious disruption of the functionality of human organs occurs. Delay in such a situation, as well as self-medication, pose a serious threat to both human health and life. With such symptoms, renal failure may develop.
After an ultrasound examination, the doctor will be able to identify the following disorders and abnormalities:
- the presence of fluid in the renal pelvis;
- reduced echogenicity;
- reverse circulation in the renal arteries;
- poor visualization of the renal veins;
- echo signal from the area of the kidney sinuses;
- tumor thrombosis;
- the presence of unclear outlines of the parenchyma.
After this, the doctor will be able to prescribe effective treatment that will help the patient get rid of the disease in a fairly short period of time.
Parenchyma structure disorders
Sometimes, during an ultrasound examination, the doctor says that the patient has diffuse changes in the renal parenchyma. What could this mean?
Uniform defeat
Such changes result from a number of diseases that occur with damage to the kidney tissue and a progressive deterioration in organ function. Most often this can be:
- Urolithiasis disease. The appearance of stones and sand in the kidney tissue leads to infectious complications and delayed outflow. When a stone moves into the lower urinary tract, the patient experiences severe pain, which is commonly called renal colic. Sand and small stones are detected in the urine; sometimes hematuria occurs as a result of damage to the mucous membrane by the sharp edge of the stone.
- Inflammatory changes that are observed with pyelonephritis. The patient's temperature rises, dull pain develops in the area of the diseased kidney, and leukocytes are found in the urine. Inflammation also occurs during glomerulonephritis, but it is not infectious, but autoimmune in nature.
- Polycystic. Unlike a solitary (ordinary) cyst, it develops as a hereditary disease that quickly leads to the development of insufficiency. Treatment is carried out in the later stages, since at first there are no symptoms. Often, a kidney affected by multiple cysts has to be removed.
- Endocrine pathology (diabetes mellitus or thyrotoxicosis). As a result of disorders associated with the pancreas or thyroid gland, a change in the structure of the vascular wall that makes up the nephron glomerulus occurs. This makes normal urine filtration impossible. Gradual atrophy and replacement with connective tissue occurs.
Some types of pathology, such as fatty or atherosclerotic deposits, are also noted on ultrasound as hyperechoic inclusions.
It becomes possible to clarify the diagnosis only after a comprehensive examination and research.
Focal processes
Focal changes occur as a result of the development of a tumor of any origin or cyst. Benign neoplasms can be significant in size and yet not produce any symptoms for a long time.
The first signs of pathology are discovered accidentally during an ultrasound scan, or in the case when compression of the urinary tract and expansion of the collecting system occurs.
In the presence of a malignant tumor, parenchyma is also detected at a late stage, which significantly worsens the prognosis.
Quite often, after examination, a doctor reveals a parenchymal kidney cyst. They can be single or multiple, the sizes are quite variable - from a few millimeters to 5 or more centimeters.
Large formations lead to compression of the parenchyma and disruption of fluid outflow. For small cysts, treatment is not prescribed; the patient is under observation; large cysts must be removed surgically.
How are pathological processes treated?
Treatment of diseases of the kidney parenchyma without professional help is almost impossible. Since diffuse changes in the renal parenchyma have different development factors, they should be treated separately. If infection is considered the basis of a pathological deviation in the parenchyma, then its source must first be eliminated. This treatment is carried out with the help of antibiotics, a dietary regimen and increased rest. Drug therapy, as well as specially selected nutrition, will help cope with poor blood flow. When none of the approaches help, doctors resort to surgery to preserve the functionality of one or both kidneys.
Self-medication is dangerous to human health and can lead to surgery.
The surface layer of the kidney plays an important role in the filtration and excretory capacity of the organ. Parenchymal abnormalities develop due to various factors and can significantly undermine human health. At the first unpleasant manifestations in the lumbar region, you should seek advice from a specialist, since self-medication can provoke a deterioration in the condition of the organ.
prourinu.ru
Renal parenchyma cyst
These are neoplasms of a liquid nature in the kidneys; single and multiple cysts should be distinguished. Bilateral kidney damage is much more common than a single cyst. This disease is called polycystic kidney disease. It should be noted that this disease is most often hereditary in nature and is transmitted directly from parents. Typically cysts do not exceed 3−5 cm.
This disease can be detected by ultrasound examination. As for treatment, there are two methods: surgery and conservative treatment. Conservative treatment includes a method of treating pyelonephritis with complex antibacterial therapy.