Definition
So, sphincter of Oddi dysfunction (SDO) is one of two functional diseases of the biliary tract (the second is a disorder of motor activity of the gallbladder). The concept of DSO refers to motor disorders of the sphincter of Oddi leading to intermittent obstruction of the bile or pancreatic ducts, the main clinical manifestation of which is a typical pain syndrome [8]. There is another definition - a benign clinical condition of non-calculous etiology, manifested by a disturbance in the flow of bile and pancreatic juice at the level of the junction of the common bile duct and pancreatic duct [1]. There are biliary and pancreatic forms of DSO and two types of DSO - stenosis and dyskinesia of the sphincter of Oddi. It seems to me that stenosis that arises, for example, as a result of a stone passing through the sphincter of Oddi, should not be included in the actual concept of DSO. True stenosis, which develops as a result of inflammation and fibrotic changes, is an anatomical rather than functional motor lesion. With the same success, we could combine diseases into one group, for example, diffuse longitudinal spasm of the esophagus and its peptic stricture.
Symptoms of the disease
Symptoms of this disorder can manifest in different ways. Most often, patients are concerned about:
- pain in the stomach (epigastric region) and right hypochondrium. The pain may last for 30 minutes or more in a row, alternating with pain-free periods;
- over the course of 12 months, the patient has experienced at least one such pain attack (or more);
- persistent pain makes it difficult to do any work and requires seeing a doctor;
- however, there are no structural changes in organs that could explain the development of pain. Ultrasound of the liver, pancreas, gall bladder shows normal.
Patients note that the first attacks of pain appear 2–3 hours after eating food.
Biliary DSO
Most often, this pathology is detected in people who have undergone cholecystectomy, but with persistent attacks of biliary pain. One of the hypotheses for the development, or rather the manifestation of this pathological condition precisely after cholecystectomy, is the loss of the reservoir function (which made it possible to compensate for increased pressure in the bile ducts) performed by the gallbladder [8]. There is also an opinion about the role of the intersection of nerve fibers going from the gallbladder to the sphincter along the cystic duct [7]. The question of the existence of clinically independent DSO before surgery is debatable. DSO occurs in 1-2% of patients after cholecystectomy [8]. A typical patient with this pathology is a woman 40-60 years old who has undergone cholecystectomy in the last 5 years. There are 3 groups of biliary DSO, each of which has certain clinical and laboratory criteria [5].
- The first type: biliary pain, changes in liver function tests (at least twice), dilatation of the common bile duct more than 12 mm, slowdown in contrast emptying for more than 45 minutes.
- The second type: biliary pain and 1-2 of the following signs - changes in liver function tests (at least twice), dilatation of the common bile duct more than 12 mm, slowdown in contrast emptying for more than 45 minutes.
- Third type: only a typical attack of biliary pain.
It should be noted that patients of group 3 predominate in clinical practice.
Literature
- McNally P.R. Secrets of gastroenterology. Moscow. "Publishing house BINOM". 1999. P. 359.
- Brandstatter G, Schinzel S, Wurzer H. Influence of spasmolytic analgesics on motility of sphincter of Oddi. Dig Dis Sci 1996;41:1814-8.
- Geenen JT, Hogan J, Dodds WJ, et al. The efficacy of endoscopic sphincterotomy in post-cholecystectomy patients with sphincter of Oddi dysfunction: Results of a four year prospective study. N Engl J Med.
- Hogan W.J. Clinical manifestations and diagnosis of sphincter of Oddi dysfunction. UpToDate.com, 1999.
- Hogan WJ, Geenen JE. Biliary dyskinesia. Endoscopy 1988;20(Suppl.1):179-83.
- Khuroo MS, Zargar SA, Yattoo GN. Efficacy of nifedipine therapy in patients with sphincter of Oddi dysfunction: a prospective, double-blind, randomized, placebo-controlled, cross-over trial. Br J Clin Pharmacol 1992;33:477-85.
- Luman W, Williams AJ, Pryde A, et al. Influence of cholecystectomy on sphincter of Oddimotility. Gut 1997;41:371-4.
- Prajapati ND, Hogan WJ Sphincter of Oddi dysfunction and other functional biliary disorders: evaluation and treatment. Gastroenterol Clin N Am 32 (2003) 601–618.
- Rolny P, Geenen JE, Hogan WJ. Post-cholecystectomy patients with 'objective signs' of partial bile outflow obstruction: clinical characteristics, sphincter of Oddi manometry findings, and results of therapy. Gastrointest Endosc 1993;39:778-81.
- Rosenblatt ML, Catalano MF, Alcocer E, et al. Comparison of sphincter of Oddi manometry, fatty meal sonography, and hepatobiliary scintigraphy in the diagnosis of sphincter of Oddi dysfunction. Gastrointest Endosc 2001;54:697-704.
- Sherman S, Troiano FP, Hawes RH, et al. Frequency of abnormal sphincter of Oddi manometry compared with the clinical suspicion of sphincter of Oddi dysfunction. Am J Gastroenterol 1991;86:586-90.
- Toouli J, Roberts-Thomson IC, Dent J, et al. Manometric disorders in patients with suspected sphincter of Oddi dysfunction. Gastroenterology 1985;88:1243-50.
- Varadarajulu S., Hawes R. Key issues in sphincter of Oddi dysfunction Gastrointest Endoscopy Clin N Am 13 (2003) 671-694.
- Wehrmann T, Seifert H, Seipp M, et al. Endoscopic injection of botulinum toxin for biliary sphincter of Oddi dysfunction. Endoscopy 1998;30:702-7.
Pancreatic DSO
Clinically it can manifest itself as recurrent chronic pancreatitis. For this form of DSO, 3 types have also been identified [11].
- The first type: pain of a pancreatic nature, amylase or lipase is 1.5-2 times higher than normal, dilatation of the pancreatic duct is more than 6 mm in the head and 5 mm in the body of the pancreas.
- The second type: pain of a pancreatic nature and 1 of the following signs - amylase or lipase is 1.5-2 times higher than normal, dilatation of the pancreatic duct is more than 6 mm in the head and 5 mm in the body of the pancreas.
- Third type: only a typical attack of pancreatic pain.
Diagnostics
It is believed that the “gold standard” for diagnosing DSO is sphincter of Oddi manometry [13]. Manometry is performed during ERCP using a special balloon. The basic tone of the sphincter and its phasic contractions are determined. Pressure above 40 mm of water column is considered pathological. Other pathological signs include an increased frequency of wave contractions and an increase in the number of retrograde peristaltic waves [12]. The absence of a decrease in sphincter pressure upon administration of smooth muscle relaxants (nitrates, calcium channel blockers) also has diagnostic significance. However, increased pressure in the sphincter of Oddi is detected in the biliary form in 86% of cases in the 1st group, in approximately 55% of cases in the second group and in 28% of patients in the third group (biliary type) and in the pancreatic form of DSO in 92%, 58%, 35 % of patients, respectively [4]. Thus, we have to admit that at least some patients with a characteristic clinical picture do not have constant sphincter hypertonicity. Unfortunately, the method of manometry in our country is inaccessible, expensive, and in addition, its implementation is associated with a certain risk of developing pancreatitis. What can we use in real clinical practice?
Ultrasound. Performing an ultrasound after prescribing a high-fat breakfast to the patient (which stimulates the secretion of bile) in patients with DSO leads to dilatation of the common bile duct as a result of increased pressure in it due to impaired outflow. An increase in diameter of more than 2 mm when measured 45 minutes after breakfast is considered diagnostic. The method is easily available in almost any medical institution. Its specificity reaches 97%, but sensitivity is only 21% (comparison was made with manometry) [10]. By the way, instead of breakfast, you can use stimulation with cholecystokinin, and to study the pancreatic duct with seretine.
The Nardi test has some value. It consists of administering substances that cause spasm of the sphincter of Oddi, for example, morphine. The result is considered positive when a characteristic pain syndrome is reproduced and (or) an increase in the concentration of AST, alkaline phosphatase or GGT in the blood. However, this test is not very specific [1].
There are reports of the successful use of syncytography for the diagnosis of DSO. However, the technique is quite complex, and the specificity and sensitivity are 78% and 49%, respectively [10].
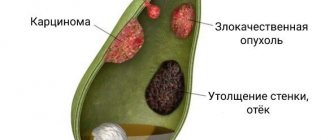
In our practice, we mainly use ultrasound. In addition, when such patients undergo RCCP and a stricture of the terminal part of the common bile duct is identified or simply a slowdown in the emptying of the biliary tract, the patient is given nitrates. The beginning (or acceleration) of their emptying after the administration of nitrates, in our opinion, with a certain degree of confidence allows us to speak about the presence of DSO in the patient. This test helps to differentiate between anatomical and functional changes in the sphincter to a certain extent. In a number of cases, seemingly obvious strictures of the terminal part of the common bile duct completely disappeared after the use of nitrates, scar narrowings did not respond to the administration of drugs. The figures show a typical RCCP picture for patients with DSO (narrowing in the terminal part of the common bile duct).
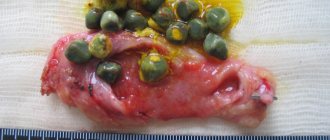
Biliary-pancreatic reflux detected on RCP also allows us to suspect this pathology, especially if the patient has a clinical picture of idiopathic recurrent pancreatitis. The picture of reflux is shown in the following figure.
Causes and risk factors
The main cause is considered to be metabolic disorders in the liver, but the following are also important:
- changes in the composition of bile,
- violation of the discharge of bile, its stagnation;
- dyskinesia of the common duct or the junction of the bile and pancreatic excretory ducts;
- careless surgical treatment, during which the sphincter of Oddi is injured, even minimally;
- excessive growth of pathological intestinal microflora.
Gastroenterologists still consider hepatic cell dyscholia to be the main reason for the formation of DSO. This is a condition in which insufficient amounts of cholecystokinin are produced. The substance is a natural regulator of the tone of the gallbladder and its ducts. Under the influence of cholecystokinin, the sphincter tone increases until the bladder is filled with bile. Once it is full, the sphincter relaxes so that bile can flow freely. After cholecystectomy, the sphincter tone changes, and bile either stagnates or continuously leaks. This changes the production of hormone-like substances that regulate metabolism in the pancreas, causing secondary pancreatitis.
Treatment
The approach to the treatment of such patients must be differentiated because the patient group is very heterogeneous. The main clinical manifestation of the syndrome is pain, and it is by its reduction that the success of treatment can be judged. Because In a number of patients with DSO, the occurrence of pain syndrome is associated with the intake of fatty foods and alcohol; it is rational to prescribe a diet similar to that for cholelithiasis. Drug treatment consists of prescribing nitrates and calcium channel blockers. For example, nifidepine proved its effectiveness in a placebo-controlled study [6]. Nitrates reduce the tone of the sphincter of Oddi in humans and animals [2], however, I have not seen any controlled studies of the effectiveness of this group of drugs in DSO. Recently, we have been trying to make wider use of antispasmodics that selectively act on the sphincter of Oddi - dicetel and duspatalin in standard dosages. They solved the unwanted cardiovascular effects inherent in the first two drugs, but there is not enough information about the degree of their effectiveness in DSO. From personal experience, the drugs lead to relief of the symptoms of “biliary” and “pancreatic” pain in a number of patients with the dyskinetic form of DSO. The positive effect of these drugs may be associated with their effect on intestinal smooth muscles, given that the combination of DSO with other dysmotor disorders of a functional nature is very likely [13]. In addition, a positive clinical effect is sometimes achieved by prescribing lyolytic therapy with ursodeoxycholic acid drugs at a dosage of 10 mg/kg body weight per day for 3-6 months. One of the possible explanations for the positive result of using this drug is the dissolution of microliths that are not detected by ultrasound.
Endoscopic sphincterotomy (EST). This is a very effective intervention that greatly facilitates the lives of patients, provided that patients are selected correctly. It is absolutely indicated for patients of group 1 and patients of groups 2-3, subject to increased basal pressure of the sphincter of Oddi. This conclusion was made based on a study of the effectiveness of PST in patients of different groups. Thus, in patients of group 1, a positive effect from sphincterotomy is observed in the vast majority of cases and, interestingly, was observed even in patients of this group with normal basal pressure in the sphincter [9]. In patients of group 2 and with increased basal pressure in the sphincter of Oddi, PST led to a positive clinical result in approximately 90% of cases; in the absence of this criterion, the intervention was ineffective [3]. Geenen JT et al. randomized patients with elevated and normal sphincter pressure to PST and “sham” PST. The percentage of patients with improvement after real and sham PST in the normotensive group did not differ significantly (42% and 33%, respectively), whereas in patients with pressure above 40 mm H2O, sphincterotomy resulted in a much higher percentage of clinical improvement than sham sphincterotomy (91% and 25% respectively) [3]. Patients in group 3 have the lowest effectiveness of PST, even with increased pressure in the sphincter [13]. Because In our work, we have decided on the possibility of measuring pressure, then in the 2nd groups we perform PST when strictures are detected on RCP or when the emptying of the common bile duct is slowed down, as well as in patients of this group with ineffective drug therapy and severe pain. We try not to perform PST in patients of the 3rd group (considering that in this group the percentage of cases of increased basal pressure in the sphincter of Oddi is small and, therefore, only a small part of patients will benefit from performing PST; in addition, they have a higher risk of developing pancreatitis and less effective PST). As for the pancreatic form of DSO, we perform PST only if biliary-pancreatic reflux is detected.
We have not used surgical sphincterotomy, sphincteroplasty and sphincter excision, described as a treatment for DSO, in our practice. In any case, only manometric data that accurately verifies DSO and the ineffectiveness of all the methods described above can justify such highly invasive interventions.
Injection of botulinum toxin into the sphincter can be effective in a number of patients [14]. However, the question of the degree and duration of the positive effect remains open.
Sphincter of Oddi dysfunctions and their treatment
WITH
The finkter of Oddi (CO) performs a coordinating function, regulating the flow of bile from the liver through the bile tract into the duodenum. CO also plays an important role in regulating the activity of the gallbladder and the flow of pancreatic secretions into the intestine. The evacuation of contents (through the major duodenal papilla into the duodenum) is significantly influenced by the motor activity of the gastrointestinal tract. A disorder of the CO function can lead to various disorders of this system. Clinically, this is manifested by attacks of pain in the upper abdomen, transient increases in liver enzymes, dilation of the common bile duct, increased pancreatic enzymes, or episodes of pancreatitis.
The causes of these disorders can be both structural (for example, CO stenosis) and functional. Currently, in accordance with the Rome consensus of 1999 (Rome II), it is recommended to distinguish sphincter of Oddi dysfunction among functional disorders of the biliary tract [7].
The sphincter of Oddi is a fibromuscular sheath surrounding the terminal sections of the common bile and pancreatic ducts and the common canal at the point of their passage through the wall of the duodenum (Fig. 1).
Rice. 1. Scheme of the anatomical structure of the sphincter of Oddi (according to MT Smith, 1999)
Accordingly, three segments are distinguished:
- the sphincteric segment of the common bile duct surrounding its distal part;
- sphincteric segment of the pancreatic duct (PG), surrounding the pancreatic duct;
- sphincter ampulla surrounding the common canal, which is formed by the confluence of the common bile duct and the pancreatic duct.
The smooth muscle fibers of the sphincter are located both longitudinally and circularly and regulate pressure in the ductal system. Basal tonic tension at rest is maintained at 10–15 mm Hg. Manometric studies show that the length of the physiological part of the sphincter is approximately 8–10 mm and may be less than its true anatomical length [8,13,14].
The sphincter of Oddi performs 3 main functions:
- regulates the flow of bile and pancreatic juice into the duodenum;
- prevents reflux of duodenal contents into the common bile and pancreatic ducts;
- ensures the accumulation of hepatic bile in the gallbladder.
These functions are related to the ability of the sphincter to regulate the pressure gradient between the ductal system and the duodenum. The coordinated contractile activity of the gallbladder and sphincter of Oddi ensures that the gallbladder is filled between meals.
Sphincter of Oddi dysfunction (SOD) is a term used to define dysfunction of the sphincter of Oddi. DSO is characterized by a partial obstruction of the patency of the ducts at the sphincter level and can have both an organic (structural) and functional (impaired motor activity) nature and be clinically manifested by a violation of the outflow of bile and pancreatic juice.
Patients with DSO can be divided into 2 groups: 1) patients with DSO due to sphincter stenosis; 2) patients with a primary functional nature of sphincter dyskinesia. True anatomical stenosis of the sphincter of Oddi and the major duodenal papilla occurs due to inflammation and fibrosis, as well as possible hyperplasia of the mucous membrane. The development of inflammatory and fibrotic changes is facilitated by the passage of small stones through the common bile duct or (presumably) relapses of pancreatitis. As a rule, it is quite difficult to distinguish functional stenosis of the sphincter of Oddi from organic one, since both conditions can be caused by the same factors.
DSO very often occurs in people who have undergone cholecystectomy. Most cases of the so-called postcholecystectomy syndrome are caused by the development of DSO. According to U. Leuschner (2001), 40% of patients who undergo standard cholecystectomy for gallstones retain clinical symptoms after surgery. In 40–45% of patients, the cause of complaints is organic disorders (biliary strictures, unrecognized stones of the common bile duct, previous diseases of the gastrointestinal tract, etc.), in 55–60% – functional ones.
Most patients who have undergone cholecystectomy are characterized by insufficiency of the sphincter of Oddi with continuous flow of bile into the lumen of the duodenum. However, its spasm may also be observed. After removal of the gallbladder, even a moderate contraction of the sphincter of Oddi can lead to a significant increase in pressure in the entire biliary tract. As a result, pain may appear, which is confirmed in experiments with the administration of morphine, which increases pressure in the bile ducts.
The Rome Consensus II (1999) provides the following criteria for diagnosing DSO.
Episodes of severe, persistent pain localized to the epigastrium and right upper quadrant of the abdomen, and all of the following:
1) painful episodes last 30 minutes or more, alternating with pain-free intervals;
2) development of one or more attacks during the previous 12 months;
3) the pain is persistent and interferes with work activity or requires consultation with a doctor;
4) there is no evidence for structural changes that could explain these signs.
In addition, pain may be associated with one or more of the following: elevated serum transaminases, alkaline phosphatase, g-glutamyl transpeptidase, direct bilirubin and/or pancreatic enzymes (amylase/lipase).
Taking into account the differences in the clinical picture of patients with DSO, 2 large categories are distinguished: 1) patients with dysfunction of the biliary segment of the sphincter of Oddi (the majority); 2) patients with predominant dysfunction of the pancreatic segment of the sphincter of Oddi (minor part).
The study of the clinical picture, laboratory data and results obtained during ERCP and sphincter manometry made it possible to subdivide DSO patients into the following groups:
1. Biliary type I
– includes:
– the presence of typical attacks of biliary colic;
– expansion of the common bile duct (> 12 mm);
– slow removal of contrast agent during ERCP (> 45 min);
– changes in the level of liver enzymes (2-fold excess of the normal level of transaminases and/or alkaline phosphatase, at least in 2-fold studies).
The cause of sphincter of Oddi dysfunction in this group is most often sphincter stenosis. Manometric evidence of DSO is found in 65–95% of patients and confirms the assumption of structural changes in the sphincter (stenosis).
2. Biliary type II
– a typical attack of biliary pain in combination with one or two other type I criteria. In patients with biliary type II, disorders can be both structural and functional. Manometric evidence is the presence of DSO in 50–63% of patients.
3. Biliary type III
– only a typical attack of biliary pain without any objective disorders characteristic of type I. In group III, DSO is usually functional in nature. Only 12–28% of patients in this group have manometric confirmation of sphincter of Oddi dysfunction [8,13].
4. Pancreatic type of DSO
clinically manifested by epigastric pain characteristic of pancreatitis, which often radiates to the back, and is accompanied by a significant increase in serum amylase and lipase. Because there are no traditional causes of pancreatitis (cholelithiasis, alcohol abuse, or other known causes of pancreatitis), these cases are usually given an indeterminate diagnosis of idiopathic recurrent pancreatitis. In the general group of patients with idiopathic recurrent pancreatitis, manometric examination reveals DSO in 39–90% of cases [7,12,13,15].
The reason for an in-depth examination to identify DSO is: the presence in patients of episodic pain, similar to the pain that occurs with gallbladder diseases, but negative according to the results of diagnostic tests (including ultrasound and examination of gallbladder bile for microcrystals); the presence of postcholecystectomy abdominal pain in patients; patients with idiopathic recurrent pancreatitis.
Initially, the diagnosis of DSO was based only on clinical manifestations. Several diagnostic tests have since been described to help identify DSO, but none of the currently used tests are ideal, and their diagnostic value remains controversial.
Laboratory research
can only be significant if they are carried out during or immediately after a painful attack. During an acute attack of pain, some patients experience a transient increase in the level of liver enzymes (AST, ALP, GGTP) and/or pancreatic enzymes (amylase, lipase). A transient increase in the level of liver or pancreatic enzymes (2 times or more) during a painful attack indicates the presence of an obstruction in the ducts, which, however, is not strictly specific for dysfunction of the sphincter of Oddi. It is necessary to exclude other causes of obstruction of the bile ducts (in particular, choledocholithiasis).
Towards non-invasive tests
belongs to the use of ultrasound scanning to determine the diameter of the common bile and/or pancreatic ducts before and after the administration of provocative agents. Fatty meal ultrasound involves ingesting fat to stimulate endogenous cholecystokinin production and increase bile secretion. The diameter of the bile ducts is measured at intervals of 15 minutes for 1 hour. Normally, the diameter of the bile ducts does not change or decreases slightly. An increase in diameter by 2 mm or more compared to the original suggests the presence of incomplete blockage of the bile ducts, but does not provide the opportunity to differentiate DSO from other causes of obstruction of the patency of the bile ducts (for example, from blockage with stones, strictures, tumors). The sensitivity and specificity of this test have not yet been precisely determined.
Currently, the most acceptable for practical use, especially when endoscopic manometry is unavailable or as a screening examination, before performing manometry, is hepatobiliary scintigraphy.
. Cholescintigraphy allows you to determine the transit time of the isotope with bile from the liver to the duodenum. A delay in transit may be in favor of DSO.
It has been shown that there is a close correlation between the results of cholescintigraphy and the results of a manometric study of the sphincter of Oddi [7].
To invasive methods
studies of SO function include: endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic manometry of the sphincter of Oddi.
ERCP
– helps exclude other diseases of the pancreas and biliary tract that cause a similar pain syndrome (for example, blockage of the duct with stones, duct strictures, tumors of the papilla of Vater and chronic pancreatitis). This method also determines the diameter of the ducts and the time of their emptying.
Endoscopic CO manometry
- is currently considered as the most reliable method for studying sphincter function. This method involves direct measurement of sphincter pressure using a special triple-lumen catheter inserted through a duodenoscope into the common bile or pancreatic duct. The proximal end of the catheter is connected to an external transducer and a writing device. Sphincter pressure is measured while the catheter is slowly withdrawn from the duct and placed in the sphincter area. Using endoscopic manometry, some indicators reflecting the motor activity of the sphincter are examined. First, the basal sphincter pressure is determined, after which the superimposed phase-wave pressure changes are recorded, as well as the amplitude, frequency and direction of propagation of the phase waves. A normal indicator of pressure in the common bile duct is a pressure that exceeds that in the duodenum by 10 mm Hg. The pressure in the CO, which is 18±4 mmHg under normal conditions, increases during its spastic contractions to 110±25 mmHg. [3,14].
Signs of DSO during manometric examination are; a) increase in basal pressure in the lumen of the sphincters; b) increase in the amplitude and frequency of phase contractions (tachyodia); c) increase in the frequency of retrograde contractions; d) paradoxical response to the administration of cholecystokinin analogues.
However, conducting this difficult study even by an experienced specialist is successful only in 80–90% of cases. 2–10% of patients develop pancreatitis after this study, the incidence of which is higher than that after ERCP.
Pretreatment manometry is not necessary in all patients with suspected sphincter of Oddi dysfunction. The prescription of CO manometry is usually based on the severity of clinical manifestations and the severity of the body's response to conservative therapy. Manometry allows an accurate diagnosis to be made before more radical treatment methods are applied.
Manometry is not needed in patients with dysfunction of the sphincter of Oddi biliary type I, changes in which are detected in approximately 80–90% of cases. Endoscopic sphincterotomy is effective in more than 90% of cases (even if the results of sphincter of Oddi manometry are normal). There is usually no need to conduct a study in biliary type III DSO, since pathological changes in SO function are rarely detected in them, and the risk of complications as a result of the study is quite high. On the contrary, in patients with biliary type II disease, a manometric study is considered mandatory, because only 50% of these patients have increased basal sphincter pressure. It is more difficult to make a decision about performing ERCP and manometric examination of CO in patients with the pancreatic type of disease. These patients are at high risk of developing study-related pancreatitis [9,11].
Treatment
Treatment methods for sphincter of Oddi dysfunction can be divided into non-invasive and invasive.
Conservative (non-invasive) treatment
Treatment should always begin with a diet and a course of drug therapy.
Diet
must have low fat content. Dietary fiber should be added to the diet in the form of plant products or food additives (bran, etc.). At the same time, vegetables, fruits, herbs are best used heat-treated (boiled, baked).
Pharmacotherapy should primarily be aimed at relieving smooth muscle spasm. For this purpose, a number of drugs that have an antispasmodic effect are used.
Nitrates:
nitroglycerin is used for rapid pain relief, nitrosorbide is used for course treatment. However, pronounced cardiovascular effects and the development of tolerance make them unsuitable for long-term treatment of biliary dyskinesia.
Anticholinergics
, blocking muscarinic receptors on the postsynaptic membranes of target organs, and as a result - relieving muscle spasm. Belladonna, metacin, platiphylline, buscopan, etc. are used as antispasmodics. However, when taking drugs of this group, a number of well-known side effects can be observed. The combination of rather low efficiency with a wide range of side effects limits their use in DSO.
Slow calcium channel blockers
– veropamil, nifedipine, diltiazem, etc. cause relaxation of smooth muscles. The drugs have numerous cardiovascular effects, primarily vasodilating ones, and therefore they are not widely used in the treatment of DSO.
The main disadvantages of drugs from all of the above groups are: a) lack of a selective effect on CO; b) significant differences in individual effectiveness in the treatment of DSO; c) the presence of undesirable effects caused by the effect on the smooth muscles of blood vessels, the urinary system and all parts of the digestive tract.
Myotropic antispasmodics
reduce the tone and motor activity of smooth muscles. The main representatives of this group of drugs are papaverine, drotaverine, bencyclane.
The most effective myotropic antispasmodic is mebeverine
– a muscle-tropic, antispastic drug with a direct effect on smooth muscles. Mebeverine has a selective effect on CO; it is 20–40 times more effective than papaverine in its ability to relax CO. In addition, mebeverine has a normalizing effect on the intestines - the drug eliminates hyperperistalsis and spasm of the duodenum without causing hypotension. The normorelaxing effect of mebeverine is due to its dual mechanism of action. Firstly, the drug has an antispastic effect, blocking the influx of sodium ions and disrupting the entry of calcium ions into the cell, which prevents depolarization of muscle cell membranes and contraction of muscle fibers. Secondly, by reducing the filling of cellular stores of calcium ions, mebeverine indirectly reduces the outflow of potassium ions and, accordingly, does not cause hypotension [1,2].
Another myotropic antispasmodic with a selective effect is the drug hymecromon (Odeston)
. Hymecromone is a phenolic derivative of coumarin, does not have anticoagulant properties, and has a pronounced antispasmodic and choleretic effect. Hymecromone is a synthetic analogue of umbelliferone, found in anise and fennel fruits, which were used in pharmacy as antispasmodics.
The mechanism of action of the drug is based on the peculiarities of its relationship with cholecystokinin (CC) at various levels of the biliary tract. At the level of the sphincter of Oddi, it acts synergistically with CC, reduces basal pressure and prolongs the opening time of the sphincter of Oddi, thereby increasing the passage of bile through the bile ducts. Being a highly selective antispasmodic, Odeston also has choleretic properties. The choleretic effect is due to the acceleration and increase in the flow of bile into the small intestine. An increase in the flow of bile into the lumen of the duodenum helps to improve digestion processes, activate intestinal motility and normalize stool [1,2,4].
Odeston is prescribed 400 mg (2 tablets) 3 times a day 30 minutes before meals, which ensures a relatively constant concentration of the drug in the serum, exceeding 1.0 μg/ml. The duration of treatment is individual (from 1 to 3 weeks).
In our observations, when prescribing Odeston as monotherapy at a dosage of 400 mg (2 tablets) 3 times a day for 3 weeks.
in patients with biliary type III sphincter of Oddi dyskinesia (19 patients) and DSO as a manifestation of postcholecysectomy syndrome (32 patients), a positive effect was obtained in all cases. The drug Odeston was well tolerated by patients; no side effects were observed in any case of its administration. The results of the study are presented in the table. Invasive treatment methods
Invasive treatment methods are recommended for patients with more severe symptoms. If conservative therapy is ineffective, as well as with suspected stenosis of the joint, most patients require endoscopic papillosphincterotomy
.
Moreover, in patients with biliary type I disease, a good effect is observed in 90% of cases. In patients with type II biliary disease and increased basal pressure of the sphincter of Oddi (based on manometry), the effectiveness of papillosphincterotomy reaches 92%. The frequency of detection of abnormalities during manometry in patients with type III biliary disease is very variable (7–55%), a positive effect is possible only in half of patients with the disease, and the risk of surgery is quite high. Therefore, papillosphincterotomy for biliary type III is practically not used [9,13]. Invasive treatment methods are recommended for patients with more severe symptoms.
If conservative therapy is ineffective, as well as if there is suspected stenosis, most patients need. Moreover, in patients with biliary type I disease, a good effect is observed in 90% of cases. In patients with type II biliary disease and increased basal pressure of the sphincter of Oddi (based on manometry), the effectiveness of papillosphincterotomy reaches 92%. The frequency of detection of abnormalities during manometry in patients with type III biliary disease is very variable (7–55%), a positive effect is possible only in half of patients with the disease, and the risk of surgery is quite high. Therefore, papillosphincterotomy for biliary type III is practically not used [9,13]. Patients with recurrent pancreatitis due to DSO, usually with pancreatic sphincter stenosis, are also candidates for papillosphincterotomy. However, due to the high percentage of complications, indications for papillosphincterotomy for the pancreatic type of DSO should be set very carefully.
Endoscopic balloon dilatation
and the installation of temporary catheter-stents constitute an alternative to papillosphincterotomy. However, the effectiveness of balloon dilatation in the treatment of patients with sphincter of Oddi dysfunction has not yet been proven, and its use is currently limited. The method of installing temporary catheter-stents in the common bile or pancreatic duct is advisable to use in patients with non-dilated bile ducts, since it is difficult to predict the outcome of papillosphincterotomy and, in addition, there is a high risk of pancreatitis. The installation of catheter-stents also does not belong to the category of absolutely safe methods [5,10].
A relatively new treatment method currently in clinical trials is botulinum toxin injection.
into the duodenal nipple. After 3–9 months. the effect of botulinum toxin disappears. Botulinum toxin leads to a reversible inhibition of acetylcholine release in local motor neurons, resulting in a decrease in CO tone. To date, this method is not widely used in clinical practice [3].
Thus, the use of modern methods for diagnosing sphincter of Oddi dysfunction, taking into account the clinical features of the course of the disease, allows timely diagnosis of this pathology in most patients.
The emergence of effective drugs with different and sometimes combined mechanisms of action makes it possible to select adequate therapy, thereby significantly improving the well-being and quality of life of patients with functional disorders of the biliary tract.
Invasive treatment methods should only be used when sphincter of Oddi stenosis is confirmed. Literature:
1. Kalinin A.V. Functional disorders of the biliary tract and their treatment // Klin. prospects for gastroenterol., hepatol. – 2002. – No. 3. – pp. 25–34.
2. Ilchenko A.A. Dysfunctions of the biliary tract and their drug correction // Klin. prospects for gastroenterol., hepatol. – 2002. – No. 5. – pp. 25–29..
3. Leishner U. Practical guide to diseases of the biliary tract. – M.: GEOTAR Medicine, 2001. – 264 p.
4. Yakovenko E.P., Agafonova N.A., Kalnov S.B. Odeston in the treatment of diseases of the biliary tract // Proc. doctor. Gastroenterology. – 2001. – Issue 4, No. 19. – P. 33–35.
5. Bader M. Geenen IE, Hogan WJ Endoscopic bolloon dilatation of the sphincter Oddi in patients with suspected biliary dyskinesia: results of a prospective randomized trial // Gastrointest. Endoscopy – 1986. – Vol. 32. – P.158.
7. Corazziari E, Shatter EA, Hogan WJ et al. Functional Disorders of the Biliary Tract and the Pancreas // Rome II. The Functional Gastrointestinal Disorders. Diqgnosis, Pathophysiology and Treatment, Second Edition, 1999 – P. 433–481.
8. Geenen JE, Hogan WJ, Dodds WJ Sphincter of Oddi // Gastroenterological Endoscopy. – Philadelphia: Sounders; 1987. – P. 735.
9. Geenen JE The efficacy of endoscopic sphincterotomy after cholecystectomy in patients with sphincter of Oddi dysfunction // New Engl. J. Med. – 1989. – Vol. 320. – P. 82–87.
10. Guelrud M., Siegel JH Hypertensive pancreatic duct sphincter as a cause of pancreatitis: successful treatment with hydrostatic balloon dilatation // Dig. Dis. Sci. – 1984. – Vol. 29. – P. 225–231.
11. Lehman GY, Sherman S. Sphincter of Oddi dysfunction // Int. J. Poncreatol. – 1996. –Vot.20. – P. 11–25.
12. Okazaki K., Yamamoto Y., Nishimori I. et al. Motility of the sphincter of Oddi and pancreatic main ductol pressure in patients with alcoholic, gallstone-associated, and idiopathic chronic pancreatitis // Amer. J. Gostroenterol. – 1988. – Vol. 83. – P. 820–826.
13. Sherman S, Troiano PP, Hawes RH et al. Frequency of abnormal sphincter of Oddi manometry compared with the clinical suspicion of sphincter of Oddi dysfunction // Amer. J. Gastroenterol. – 1991. – Vol. 86. –P. 586–590.
14. Smith MT Dysfunction of the sphincter of Oddi // Secrets of gastroenterology: Transl. from English – M.; St. Petersburg: BINOM, Nevsky dialect, 1998. – pp. 357–372.
15. Tuouli J., Roberts–Thomson IC, Dent I. et al. Sphincter of Oddimotility disorders in patients with idiopathic recurrent pancreatitis // Brit. J. Surg. – 1985. – Vol. 72. – 859–863.