Causes of the disease
Irritable bowel syndrome is a set of symptoms of digestive disorders
Irritable stomach syndrome is a functional disorder that affects not only the stomach itself, but the entire digestive tract. Due to the fact that patients do not always turn to doctors on time, the disease progresses to the most severe stage and brings a lot of unpleasant sensations. It is generally accepted that the main causes of this syndrome are:
- Poor nutrition, namely the consumption of protein-carbohydrate foods. This does not mean one-time use, but constant and long-term use.
- Frequent “dry” meals. This usually happens among students and schoolchildren who are too lazy to eat normally and buy rolls in the canteens of educational institutions.
- Eating food that is well seasoned, and mainly hot spices, which provoke excessive secretion of gastric juice
- Eating very fatty foods, which leads not only to disruptions in the stomach, but also significantly increases cholesterol levels in the blood
- Eating very hot food. Some people prefer to eat soups and main courses when they are just cooked. And, as you know, their temperature goes through the roof. And thereby the gastric mucosa is irritated and burned
- Eating cold food. As with hot food, cold food can cause stomach cramps.
- Taking certain medications that have a negative effect on the gastric mucosa
- Alcohol abuse. And if the consumption of weak alcoholic drinks is sometimes allowed, then even in this case they can lead to even greater irritation and pain
- Frequent consumption of coffee drinks. Strong drinks such as espresso pose the greatest danger
- Acceptance of products that have either expired or are approaching their expiration date
- The stress that a person experiences every day. Often, even strong emotional stress can lead to the fact that he feels severe pain in the abdomen
Often the cause of irritable stomach syndrome is some other disease of the digestive system, during which the process of regulating the production of gastric juice is disrupted.
Irritable bowel syndrome and other functional disorders in adults
Functional disorders (disorders, diseases) of the gastrointestinal tract are conditions that are accompanied by a number of symptoms that significantly worsen the quality of life of people, but such symptoms are not associated with any changes in target organs at the cellular level. In other words, these disorders of the gastrointestinal tract do not manifest themselves as abnormalities in laboratory tests, do not lead to changes in the tissues of the mucous membrane of the esophagus, stomach or intestines and are not diagnosed by ultrasound, CT or MRI.
In most cases, modern diagnostic tools are not able to detect any pathological changes in functional disorders; from their point of view, a person can be considered healthy. But he is worried about abdominal pain, bowel movements, nausea, bloating and other unpleasant symptoms, just like people with chronic diseases. Moreover, functional disorders are the most common among gastrointestinal diseases and occur in both adults and children.
Reasons for development
The exact causes of functional disorders have not yet been determined. It is assumed that all varieties of these diseases have common causes, the main one being dysregulation of the interaction between the central nervous system (brain) and the peripheral nervous system, which regulates the activity of the gastrointestinal tract. This mutual connection is called the “brain-gastrointestinal axis.” In addition, disturbances in the sensitivity of internal organs, gastrointestinal motility and intestinal microflora, as well as frequent stressful situations and the presence of psychological problems, additionally contribute to the development of functional diseases.
The results of independent epidemiological studies showed that in 50% of cases the development of functional gastrointestinal diseases was preceded by psychoemotional stress; in the other half of the patients, disorders began with intestinal dysfunction, which was accompanied by psychological stress.
Types of functional disorders of the gastrointestinal tract
Currently, the Rome VI revision criteria, published in 2016 by an international expert group that was specifically created to develop algorithms for the diagnosis and treatment of these diseases, are used to classify functional disorders.
The classification of functional disorders has 6 subgroups, divided according to their relationship with the affected area of the gastrointestinal tract:
- esophageal disorders;
- stomach and duodenal disorders;
- intestinal disorders;
- functional abdominal pain;
- disorders of the biliary tract (biliary tract);
- anorectal disorder.
The most common types of functional digestive disorders are: irritable bowel syndrome, functional dyspepsia and functional biliary disorder.
IBS is the most common functional disorder
Irritable bowel syndrome (IBS) is a condition associated with functional disturbances in the intestines and is accompanied by bloating, discomfort or pain in the abdomen, diarrhea or constipation, or both. This condition can last 3 or more months and is not associated with the presence of infection or inflammatory changes in the intestines. With irritable bowel syndrome, first of all, the regulation of motor activity of the colon is disrupted. Women suffer from irritable bowel syndrome more often, the average age of onset of the disease is from 20 to 40 years.
Risk factors for developing IBS are:
- an episode of acute intestinal infection in the medical history;
- chronic stress and emotional instability;
- disturbance of intestinal microflora;
- low levels of intestinal enzymes involved in the digestion of organic substances contained in some foods.
What is functional dyspepsia?
Functional dyspepsia is a disorder of the gastrointestinal tract, characterized by a feeling of fullness in the abdomen after eating, early satiety, pain or burning in the upper abdomen (epigastric region), which is not explained by the results of an endoscopic examination. Like IBS, functional dyspepsia is more common in women.
Risk factors for the development of functional dyspepsia are:
- taking non-steroidal anti-inflammatory drugs;
- the presence of concomitant psycho-emotional disorders;
- Helicobacter pylori infection;
- an episode of acute intestinal infection in the medical history;
Currently, patients with functional stomach disorders after eating can take part in a clinical trial conducted at the Expert Center. Inquiries by phone...
Biliary dyskinesia and its new name
Until recently, the term “biliary dyskinesia” was commonly understood as a complex of disorders of the biliary system caused by impaired motor function of the gallbladder and bile ducts in the absence of their organic changes. However, after more detailed consideration and study by an expert group of gastroenterologists from the Rome Foundation, it was decided to give this condition a new name - functional biliary disorder, which is divided into gallbladder function disorder and sphincter of Oddi disorder.
Risk factors for the development of biliary disorders are:
- hereditary predisposition;
- elderly age;
- concomitant chronic gastrointestinal diseases (gastritis, duodenitis, colitis, ileitis, peptic ulcer, celiac disease);
- chronic inflammatory processes of the abdominal and pelvic organs;
- infections (bacterial, viral, helminthic, parasitic, giardiasis);
- hormonal disorders and obesity;
- postoperative conditions - removal of the gallbladder, etc.;
- allergic diseases;
- psycho-emotional overload;
- the use of medications that lead to “thickening” of bile.
Symptoms
Depending on the area of the gastrointestinal tract affected by the functional disorder, the following symptoms are possible:
- from the esophagus (feeling of a lump in the throat, belching of air or food, chest pain, heartburn, difficulty swallowing food and liquid);
- from the stomach (heaviness, discomfort and pain in the stomach, feeling of fullness, increased swallowing of air when eating);
- from the intestines (diarrhea, constipation, unstable stools, abdominal pain, bloating);
- from the bile ducts and gallbladder (pain in the right or left hypochondrium, bitter taste in the mouth, nausea, vomiting);
- from the anorectal region (difficulty in defecation, fecal incontinence).
Symptoms of functional disorders are often similar to those of other chronic diseases of the gastrointestinal tract (inflammatory bowel disease, celiac disease, peptic ulcer disease) and including cancer of the gastrointestinal tract. Therefore, the diagnosis is established only after a detailed examination and exclusion of pathologies.
Alarming symptoms indicating the possible presence of a dangerous gastrointestinal disease:
- unexpected weight loss (> 10% of ideal body weight);
- nocturnal diarrhea or abdominal pain at night;
- constant severe abdominal pain;
- onset of symptoms in old age;
- blood in stool;
- blood relatives with inflammatory bowel disease or colon cancer.
Diagnostics
Diagnosis of functional disorders begins with a detailed examination by a gastroenterologist and depends on the prevailing symptoms and individual characteristics. The set of studies required for the examination is determined after a detailed examination and questioning of the patient and may include:
- lab tests;
- Ultrasound of the abdominal cavity and intestines;
- endoscopic examinations with biopsy (FGDS, colonoscopy);
- esophageal manometry;
- daily pH-metry and impedance measurements;
- endo-ultrasound or magnetic resonance cholecystocholangiography.
In addition to consulting a gastroenterologist, in some cases and depending on the symptoms, consultation with a cardiologist, neurologist or psychotherapist may be required.
The diagnosis is established only after excluding chronic diseases that cause damage to the gastrointestinal tract and have similar symptoms.
You can get advice from doctors specializing in the management of patients with functional disorders at GC Expert, make an appointment by phone + or through the form on the website.
Treatment
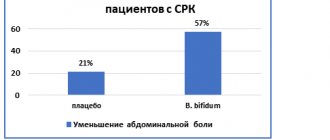
Treatment of functional disorders is complex and depends on the prevailing symptoms and the gastrointestinal organs involved. It consists of both treatment aimed at weakening and eliminating symptoms, and aimed at normalizing the functioning of the gastrointestinal tract. In case of irritable bowel syndrome, the composition of the intestinal microflora (microbiota) is also corrected.
Psychotherapeutic treatment is also often used; it is necessary to focus patients’ attention on reducing stress, normalizing sleep and rest.
Do I need to follow a diet for functional disorders?
General dietary recommendations consist of gentle and regular meals 3-4 times a day, avoiding overeating and consuming foods that provoke an increased secretion of digestive juices, bile or cause fermentation in the intestines. These products include:
- fatty, fried, too salty foods;
- smoked, spicy dishes;
- cabbage and legumes;
- Rye bread;
- spices and alcohol.
A special diet may be effective for some people with irritable bowel syndrome and bloating associated with improper digestion of food components such as fermentable oligosaccharides, disaccharides or monosaccharides and polyols, known as the FODMAP diet.
For disorders associated with the biliary tract and gall bladder (functional biliary disorders), it is recommended to take as a basis a balanced diet with the exclusion of foods containing refractory fats and the inclusion of a sufficient amount of plant fiber and foods with lipotropic properties (preventing the accumulation of fat in the liver).
You can undergo examination and treatment of functional disorders at GC Expert. Our center’s gastrodietician, Svetlana Igorevna Kovaleva, will help you create a diet that will help improve your well-being for various types of functional gastrointestinal disorders.
Symptoms of an irritable stomach
Acute pain as one of the symptoms
Gastric juice plays a big role in the digestion process, and then when malfunctions occur, that is, it ceases to be produced normally or, on the contrary, too much of it is produced, and problems begin. Irritable stomach syndrome has several obvious symptoms, which, however, can be confused with another disease. In any case, if you experience the following sensations, you should contact a specialist:
- Nausea, which occurs mainly after eating. Throughout the day, a person feels normal, but when he eats something, literally after twenty or thirty minutes he begins to suffer from nausea, which can be either strong or not so strong. It all depends on the degree of development of the problem
- Belching, which is not a one-time occurrence. Moreover, it also begins to appear after eating, and the number of attacks can reach ten or twenty times per hour
- Heartburn. It appears, like the two above symptoms, after eating. It happens especially clearly if a person has eaten and immediately assumes a lying position. It is in this position that gastric juice begins to be released more into the esophagus, thereby irritating the mucous membrane. In especially severe cases, when a large amount of gastric juice is thrown back, the person may vomit, as a lot of saliva will be produced
- Painful sensations that may or may not appear. But many patients note that immediately after eating, the stomach seems to shrink, and a strong pain sensation appears, the so-called spasm. Usually it goes away within half a minute, but all this time it gives the person unpleasant sensations
- A feeling of heaviness that is absolutely independent of the time of eating. Most often it is constant, but in some cases it subsides for a short period of time, but then appears again
- Vomiting, during which a huge amount of gastric juice will be thrown out
- Weight loss, which occurs when a person does not pay attention to problems and does not try to help the body
- Intolerance to certain foods. Typically this includes salted fish (for example, herring), spicy fish, radishes, the digestion of which requires the production of more gastric juice
If at least a few of the listed symptoms appear, you must urgently pay attention to this and visit a specialist who will accurately determine the cause of their occurrence and, if necessary, prescribe appropriate treatment.
Symptoms
Doctors distinguish three groups of IBS symptoms:
- Defecation disorders: constipation, diarrhea, their alternation. Digestive disorders: nausea, vomiting, decreased appetite.
- Unpleasant sensations in the intestinal area: pain, spasms, twisting, bloating, seething, distension and fullness, numbness, burning, etc.
- Symptoms from the nervous system and mental sphere: increased attention to one’s physical condition, hypochondria, anxiety, obsessive fears, sleep disorders (from insomnia to increased drowsiness), avoidance of certain foods, increased fatigue, headaches, etc.
IBS is characterized by some relief after a bowel movement and absence of symptoms during sleep.
In adults
For adults, there is a higher prevalence of IBS in women than in men, a direct connection with the emotional state. The older the age, the less pronounced the symptoms.
In children
IBS in children is most often a manifestation of neurosis - a psychological conflict between what is desired and what is actual. The most common reason for this violation lies in family relationships. Therefore, to adequately help a child with IBS symptoms, family psychotherapy will be required.
Who is treating? Who and where to turn to for IBS?
IBS is treated by a psychotherapist or psychiatrist. You can contact any clinic licensed to provide mental health care: a private psychiatric clinic, a public hospital or a mental health center.
Detection and diagnosis
To make an accurate diagnosis, it is necessary to exclude internal diseases that occur with similar symptoms: infections of the gastrointestinal tract, intestinal neoplasms, gastrointestinal bleeding, inflammatory and degenerative diseases of internal organs. To do this, the doctor carefully collects an anamnesis (life history and illness), assesses the physical and mental state. If necessary, tests and hardware examinations (tomography, ultrasound, colonoscopy) can be carried out and related specialists can be involved: surgeon, gastroenterologist, infectious disease specialist, gynecologist, urologist and others.
Establishing diagnosis
Only a doctor can make an accurate diagnosis, and only after conducting appropriate tests and studies, the results of which will make the whole picture clear. The specialist will prescribe a series of studies that will help narrow the range of problems and exclude more serious diseases. The main methods for diagnosing irritable stomach syndrome include:
- X-ray. It is during the X-ray that the amount of gastric juice that is currently present in the stomach will be visible.
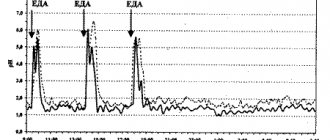
- Study of the acidity of the environment. To do this, a special probe is inserted through the person's mouth, with which the acidity in the stomach is measured. To do this, several areas are selected, which is necessary for a more accurate result. In addition, the probe measures basal temperature, as well as how quickly or slowly acid is produced. Today, thanks to the latest technologies, it is possible to accurately determine where the cells are located that produce either less or more acid.
- Research using stimulants. The stimulant activates the production of secretion. Using this study, the acidity of the stomach is measured, which a person will have on an empty stomach, as well as after eating
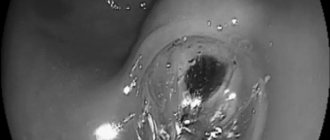
- FGDS, during which the doctor will completely examine the internal state of the mucous membrane of not only the stomach, but also the duodenum, which is closely connected to it
- Ultrasound examination, during which it is determined whether there are any abnormalities in the pancreas, as well as the absence of enlargement of other important organs
Before making a diagnosis, the doctor will fully study the results and, guided by them, prescribe treatment, if required.
Treatment of the syndrome
Diet as one of the treatment methods
If a person has been diagnosed with this, it will be necessary to follow all the doctor’s recommendations so that the disease does not progress to a more severe stage, which is not only problematic, but sometimes impossible to treat. Treatment will be as follows:
- Eating only healthy foods
- Avoiding fatty and spicy foods
- Following a special diet
- Taking sedatives that primarily affect the nervous system. And as mentioned above, stress is one of the most common causes of the problem.
- Taking antacids, which will not only reduce the activity of gastric juice and reduce pain that occurs immediately after eating
- Taking activated carbon or decoctions made according to folk recipes in order to reduce gas formation
- Taking medications that will stimulate peristalsis
- Taking enzymes to help digest food better
Maintaining proper nutrition plays a big role in the treatment of irritable stomach syndrome, because if this is not done, then medications are unlikely to have a positive effect and relieve at least pain.
Gastritis - inflammatory changes in the gastric mucosa
16.04.2021
Gastritis is a stomach that is inflammatory in nature and affects the mucous membrane. This is a fairly common disease that occurs in people of all ages. Gastritis can be chronic and acute. Chronic gastritis is associated with recurrent lesions, dysfunction of the stomach and structural changes in its mucosa. It can be: bacterial, autoimmune, mixed. There is also reflux gastritis. Acute, caused by temporary damage to the gastric or in addition to infections. Acute gastritis can be fibrous, catarrhal, corrosive, phlegmanous.
Causes of the disease
The causes of gastritis are different. The most common cause is infection with the bacterium Helicobacter pillory, which is very easy to become infected, but sometimes there are no signs of infection, even after several years, and at this time changes are already occurring in the stomach . Other reasons may be:
- bad habits (smoking, alcohol);
- stress;
- unhealthy diet (violation of the eating schedule, dry food, constant consumption of fatty, spicy foods);
- allergic reactions to certain foods;
- medical supplies;
- worms;
- reflux;
- infections;
- autoimmune diseases.
Symptoms. Diagnosis of gastritis
With chronic gastritis , symptoms such as belching , loss of appetite, nausea , pain, heaviness in the stomach , bitterness in the mouth , and coating on the tongue usually appear. Chronic gastritis often progresses sluggishly.
Acute gastritis itself appears suddenly. It is characterized by acute pain in the solar plexus, bloating , nausea , heartburn , and increased gas .
Initially, the diagnosis begins with an analysis of the patient’s complaints, then the doctor examines the skin and palpates the abdomen in the stomach for the presence of pain. Then laboratory methods are carried out, such as: analysis for the presence of the bacterium Helicobacter pillory, general blood , stool analysis for hidden bleeding and its microscopy, biochemical analysis of blood and urine . Instrumental diagnostics are also important for more effective treatment afterwards. gastritis is suspected, gastroscopy is performed . A flexible endoscope, which is equipped with a camera, is inserted through the mouth into the stomach . This helps to see a more complete picture of what is happening in the body, because the doctor sees the mucous membranes, and in some cases takes pictures or video. Also, in order to make sure that the symptoms are not caused by other diseases, the doctor prescribes an ultrasound examination of the abdominal cavity, and sometimes an MRI.
Treatment of gastritis
Treatment of chronic gastritis is selected individually for each patient. If the patient has an advanced form, then treatment takes place in the hospital , most often for two weeks. The main ones are giving up cigarettes and alcohol, medication and diet . There are different groups of medications. For pain, doctors prescribe antispasmodic drugs. In order to protect the gastric , gastroprotectors are used. If bacteria is detected. Antacids are prescribed when the patient has hyperacidity. Diets are also prescribed differently, for example, if the patient has high acidity, he should follow diet table No. 1 for the first days, then switch to diet table No. 16 for two weeks, then table No. 1 for the next three months. For low acidity - table No. 2. After three months of such nutrition, you still need to follow a diet that is not so strict, but you need to forget about fried, salty, spicy, pickled or fatty foods. You should visit your doctor and undergo examinations.
For acute gastritis, medications are also taken. the stomach is cleansed . A course of vitamins is prescribed; in case of poisoning with toxins, antibiotics, antispasmodics, antacids and enterosorbents are prescribed. The first day it is recommended to drink only warm water, then gradually start eating liquid food, then you can eat crackers and liquid cereals, drink jelly. After a week of eating this way, you can switch to diet table No. 1. Acute gastritis can generally be cured in two weeks, but this does not mean that you need to return to your previous lifestyle. As is the case with chronic gastritis , it is better to get rid of bad habits and carefully monitor your diet.
Published in Gastroentorology Premium Clinic
Principles of nutrition
As with any other stomach disease, you need to immediately rebuild your body and start eating only healthy foods. It is strictly forbidden to eat hamburger, potatoes and other dishes, the content of cholesterol and fat in which is simply off scale. In addition, you need to eat at least five times a day. This does not mean that at each of these meals you need to eat as much as you could eat in a week. If for some reason you had to eat fatty foods, then it is best to drink either Nosh-pu or Pakreatin. Nosh-pa will relieve spasms, but pancreatin will help digest food better.
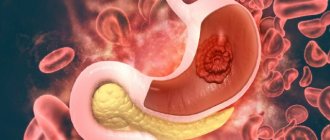
Causes of development of gastric ulcer
Stomach ulcer is a common disease that causes the development of local damage to the mucous membrane of the digestive organ and disruption of tissue nutrition.
Up to 40% of cases of peptic ulcer develop as a result of exposure to infectious factors (the causative agent is the bacterium H. pylori). In addition, the cause of gastric ulcer (GUD) can be taking medications, the presence of cancer, the presence of foreign bodies in the stomach, tuberculosis, syphilis and HIV. Gastric ulcer is a recurrent disease, characterized by alternating periods of exacerbation and remission. More than 300 million people worldwide suffer from peptic ulcer disease.