The gallbladder is a reservoir for bile secreted by the liver. It regulates the flow of bile into the intestines and if its functioning is disrupted, the acid-base balance is disrupted and damage is caused to liver tissue. The gallbladder also performs other functions: the production of special mucus, acetylcholecystokinin, and the reabsorption of nutrients occurs in it. The main tasks performed by this body:
- Gastric juice is neutralized in the gallbladder;
- Activates the production of necessary enzymes in the intestines;
- Neutralization of harmful microorganisms in the digestive tract;
- Improves intestinal elasticity and mobility;
- In case of poisoning and intoxication of the body, it is the gallbladder that promotes the removal of harmful and dangerous substances.
Types of diseases
There are a large variety of gallbladder diseases, but they can all be divided into main types:
- Inflammatory processes - caused by fungi, viruses, infections, can cause a disease such as non-calculous cholecystitis;
- Stagnation of bile. Due to the disturbance in the composition of bile, there is an increased risk of cholelithiasis;
- Neurological diseases. Due to a disruption in the flow of impulses into the gallbladder, the release of the required amount of gastric juice fails;
- Hereditary predisposition and genetic abnormalities. Most often, a congenital bend of this organ is observed;
- neoplasms in the gallbladder: polyps, malignant tumors.
Causes
JVP can be primary or secondary. It is worth noting that pathology rarely occurs as a separate disease. The primary process can be caused by the following reasons: nervous overstrain (no structural changes in the organ are observed), eating disorders: overeating, fasting, quick snacks, abuse of fatty, fried foods, sedentary lifestyle, muscle weakness, lack of body weight, allergies, bronchial asthma and more.
The secondary process occurs against the background of existing diseases:
- diseases of the digestive tract: gastritis, duodenitis, colitis, peptic ulcer;
- chronic diseases of the abdominal cavity and pelvic organs: adnexitis, pyelonephritis, ovarian cyst;
- disorders of the liver, gallbladder and biliary tract;
- bacterial inflammation of the gastrointestinal tract;
- giardiasis;
- congenital anomalies of the gallbladder;
- endocrine disorders.
Dyskinesia can be caused by nervous tension.
Common symptoms of gallbladder disease
- Pain under the right rib. The intensity can be very different, depending on the disease. Oncological diseases at an early stage are practically painless, but cholelithiasis is characterized by acute, throbbing pain;
- Nausea, vomiting, diarrhea, increased sweating are common symptoms of gallbladder diseases;
- Bitterness in the mouth. If this symptom occurs, you should immediately undergo a full examination; such a signal can be caused by a serious disease not only of the gallbladder, but also of the liver;
- Redness of the tongue. It is redness that indicates possible problems with the gallbladder;
- Darkening of urine. Due to insufficient filtration, certain substances accumulate in the urine, which affect its color;
- Change in stool color. If there are problems with the gallbladder, the supply of stercobilin is disrupted, which causes stool discoloration;
- Jaundice. One of the most common symptoms of gallbladder problems. Due to the disruption of bile circulation, it begins to enter the blood and, as a result, acid enters the mucous membrane. This causes the whites of the eyes, mouth, and, if left untreated, the skin to turn yellow.
To prescribe effective treatment for the gallbladder, it is necessary to correctly establish the cause and an accurate diagnosis; this can only be done by a specialist. Do not engage in self-diagnosis and self-medication; the symptoms of many diseases are very similar and if you start taking the wrong medicine, there is a high risk of harming your body. Listen to your body and at the first signs of possible problems, get diagnosed.
BILIARY DYSFUNCTION: definition, classification, diagnosis, treatment
Definition (pathomorphological background)
Despite the fact that they try to consider the biliary system (the system of bile ducts and sphincters that regulate the flow of bile) separately from the main organ (liver), it is part of it and functions in accordance with this.
The hepatocyte is conventionally divided into 3 independent units: sinusoidal, lateral and canalicular parts. The apical (canalicular) part of the cytoplasmic membrane of the hepatocyte differs in histological and biochemical properties and is involved in the formation of the lumen of the bile capillary. Each liver cell takes part in the formation of several bile canaliculi (BCs). At the periphery, the bile duct lobules merge into the bile ducts themselves, which pass at the exit into the interlobular connective tissue into interlobular tubules, which, merging, form interlobular ducts of the first order (second - when they are already lined with prismatic epithelium). Tubular-acinous mucous glands, a connective tissue membrane, and elastic fibers appear in their walls. The interlobular ducts, merging, form large hepatic ducts - lobar, leaving the liver and, in turn, forming the common hepatic duct, the continuation of which is the common bile duct, its beginning is considered to be the junction of the hepatic duct with the cystic duct. The common bile duct is divided into supraduodenal, retroduodenal, retropancreatic, intrapancreatic and intramural sections.
The distal part of the common bile duct passes through the thickness of the head of the pancreas, and the duct opens on the posterior wall of the descending duodenum, 2–10 cm below the pylorus. According to various authors, the width of the ducts can vary: common bile duct (GC) - from 2 to 4 mm; hepatic - from 0.4 to 1.6 mm; cystic - from 1.5 to 3.2 mm. According to x-ray data, the width of the coolant duct is from 2 to 9 mm; according to ultrasound - in the presence of a gallbladder (GB) - from 2 to 6 mm, and without a gallbladder - from 4 to 10 mm. The capacity of the gallbladder ranges from 30 to 70 ml. At the junction of the gallbladder and the cystic duct, the muscle fibers take a circular direction, forming the sphincter of the gallbladder duct (Lutkens). Motor innervation is carried out by the sympathetic and parasympathetic nervous system. Nerve plexuses are present in all layers of the biliary system. Sensitive fibers of the gallbladder can only perceive stretching.
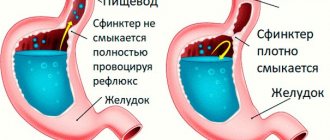
Bile secretion occurs continuously throughout the day, with some fluctuations. From 0.5 to 2.0 liters of bile are secreted per day. The direction of bile movement is determined by the interaction of hepatic secretion, the rhythmic activity of the sphincters of the terminal part of the common bile duct, the sphincter of the gallbladder, the cystic duct valve and the absorptive function of the mucous membrane of the gallbladder and all ducts, which creates pressure gradients. From the hepatic ducts and the common bile duct, bile enters the gallbladder at the moment of closure of the sphincter of Oddi (it plays a decisive role in creating the pressure gradient). The sphincter of Oddi outside of digestion is not constantly closed, and small portions of bile systematically enter the duodenum. After the end of the digestive phase, bile enters the gallbladder for 3 or more hours. Most researchers believe that the extrahepatic bile ducts are never at rest, and their active peristalsis is considered from the point of view of regulation of bile flow; duodenal tone (intraluminal pressure) also affects the output of bile. The motor reaction of the gallbladder and sphincter of Oddi is directly dependent on the quantity and quality of food, as well as on the emotional state of a person.
The musculature of the sphincter of Oddi is independent of the musculature of the duodenum. The sphincter of Oddi consists of: the actual sphincter BDS (Westphal sphincter), which ensures the separation of the ducts from the duodenum; the sphincter of the common bile duct itself; sphincter of the pancreatic duct.
The work of the entire biliary system is strictly coordinated, which is ensured by nervous and humoral regulation. The regulatory influence of endogenous peptides from the endorphin group is still not entirely clear. The basic principle of the entire regulatory system is multi-level self-regulation (including locally produced hormones and biologically active substances).
The regulatory component is very complex under physiological conditions and is not completely clear in various pathologies of this system.
Classification, identification of clinical variants of dysfunction, diagnostic approaches
Functional diseases of the biliary tract are a complex of clinical symptoms that develop as a result of motor-tonic dysfunction of the gallbladder, bile ducts and sphincters.
According to the latest International Classification, instead of the definition of “functional diseases of the biliary tract” (Rome Consensus, 1999), the term “dysfunctional disorders of the biliary tract” has been adopted. Moreover, regardless of the etiology, they are usually divided into 2 types: gallbladder dysfunction and sphincter of Oddi dysfunction.
In the latest International Classification of Diseases (ICD-10), under the heading K82.8 only “dyskinesia of the gallbladder and cystic duct” is highlighted and under the heading K83.4 – “spasm of the sphincter of Oddi”.
The parasympathetic and sympathetic parts of the autonomic nervous system, as well as the endocrine system, take part in the regulation of the motor activity of the biliary system, providing a synchronized sequence of contraction and relaxation of the gallbladder and sphincter apparatus.
It has been shown that moderate irritation of the vagus nerve causes coordinated activity of the gallbladder and sphincters, and severe irritation causes spastic contraction with delayed bile evacuation. Stimulation of the sympathetic nerve helps relax the gallbladder. Of the gastrointestinal hormones, cholecystokinin-pancreazimin (CCK-PZ) has the maximum effect, which, along with contraction of the gallbladder, helps relax the sphincter of Oddi. The incentive for the production of CCK-PZ is fatty foods, and the nervous regulatory influences are the pressure gradient and its change.
The main cause of disorders of the rhythmic activity of the biliary system is inflammatory processes in the liver, leading to disruption of bile synthesis, a noticeable decrease in pressure in the ductal system and gall bladder and, in connection with this, to constant spastic contraction of the sphincter of Oddi.
Various surgical interventions (cholecystectomy, vagotomy, gastrectomy) also lead to significant dysfunction of the biliary system. Unlike the processes occurring in other digestive organs, the formation of bile occurs continuously, but the flow of bile into the intestines is noted only during certain phases of digestion. This is ensured by the reserve function of the gallbladder and its rhythmic contractions with sequential relaxation of the sphincters of Lutkens and Oddi. Relaxation of the gallbladder is accompanied by closure of the sphincter of Oddi.
There are primary and secondary dysfunctional disorders. Primary ones are rare and average 10–15%. In this case, a decrease in the contractile function of the gallbladder may be associated both with a decrease in muscle mass (rarely) and with a decrease in the sensitivity of the receptor apparatus to neurohumoral stimulation. Moreover, a small number of receptors can be genetically determined and acquired, due to inflammatory, dystrophic and metabolic disorders. Secondary dysfunctional disorders of the biliary tract can be observed with hormonal disorders, treatment with somatostatin, premenstrual syndrome, pregnancy, systemic diseases, diabetes, hepatitis, liver cirrhosis, jejunostomy, as well as with existing inflammation and gallstones. Moreover, the presence of these diseases does not imply a stable failure of regulatory systems and the perceptive apparatus - we are talking about varying degrees of disorders in different periods, phases of the course of diseases; in connection with this, there is an “undulation” of disorders, up to periods of rather long stability, but with an “easy” transition of this system from stability to motor disorders. Psycho-emotional overload, stressful situations, and general neuroses are important. The vast majority of patients who have undergone cholecystectomy are characterized by insufficiency of the sphincter of Oddi with continuous flow of bile; spasm is less common. Another common cause of biliary disorders is distal gastrectomy, which leads to decreased hormonal regulation and hypotony of the gallbladder.
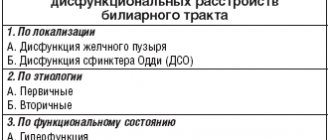
The classification of dysfunctional disorders of the biliary tract is presented in the table.
For ease of perception and more convenient application in practice, the classification presents unidirectional disorders, although in life they are more often complex in nature, with a predominance of one of the components.
Clinical manifestations are quite well known: with hyperkinetic disorders, colicky pain of varying intensity occurs without irradiation or with irradiation to the right, to the back, sometimes to the left half of the abdomen (with the involvement of the pancreatic ductal system). With hypokinesia - dull pain in the right hypochondrium, a feeling of pressure, fullness, increasing with changes in body position and with an increase in intra-abdominal pressure, changing the pressure gradient for bile flow. Common to different forms of dysfunction are bitterness in the mouth, bloating, and unstable stools.
So, the central symptom of gallbladder dysfunction is the biliary type of pain, and the only objective characteristic can be considered delayed emptying of the gallbladder. Available diagnostic methods do not explain the cause of this phenomenon. There may be several causative factors. It is impossible to exclude such moments as a violation of filling or a decrease in the sensitivity of the gall bladder’s receiving apparatus.
Diagnostic criteria for gallbladder dysfunction are episodes of severe constant pain localized in the epigastrium or in the right upper quadrant of the abdomen, with the following features characteristic:
- episodes lasting 30 minutes or more;
- symptoms occur 1 or more times in the previous 12 months;
- constant nature of pain, decreased daily activity of patients and the need to consult a doctor;
- lack of evidence of organic pathology causing symptoms;
- presence of dysfunction of gallbladder emptying.
A very important objective symptom of impaired gallbladder motility is the ultrasound phenomenon of “sludge” (sediment), which, according to our data [1], can be presented in 2 variants: a) diffuse; b) near the wall. The parietal variant, depending on the clinical situation, can be characterized as “inflammatory”. If there is no inflammation, then the sediment elements that form it are quite large. The entire clinical symptom complex should also be analyzed: nausea and vomiting, irradiation, provoking factors (food, its quality, etc.).
With regard to sphincter of Oddi dysfunction, 4 clinical and laboratory types are distinguished (3 types of biliary dysfunction and 1 type of pancreatic dysfunction). The diagnostic criteria are based on an attack of biliary pain and 3 laboratory and instrumental signs: an increase in AST and/or alkaline phosphatase by 2 or more times with double determination; slower removal of contrast agents during ERCP (more than 45 minutes); expansion of the common bile duct more than 12 mm (studies are carried out during an attack).
The first type of dysfunction is characterized by pain and 3 signs.
The second type of dysfunction is characterized by pain and 1 or 2 signs.
The third type is only an attack of pain.
The fourth type - pancreatic - is characterized by “pancreatic” pain and an increase in the level of amylase or lipase (with mild pain); an increase in enzymes (amylase, lipase) may be absent.
In cases where endoscopic retrograde pancreatic cholangiography excludes the absence of stricture pathology, monometry of the biliary and pancreatic sphincters is indicated.
The World Congress of Gastroenterology (Bangkok, 2002) determined that evidence-based medicine does not require consensus, but rather evidence. Congress participants concluded that sphincter of Oddi dysfunction should not be classified as a clearly defined disease, but as a condition with a variable dysfunction/symptom relationship. It was particularly emphasized that impaired gallbladder emptying is well known as a consequence of inflammatory damage, mechanical obstruction or autonomic denervation. In the absence of these conditions, it is unclear whether delayed gallbladder emptying can be considered a specific clinical problem (nosological entity).
Some principles of treatment of dysfunctional biliary disorders
Considering the above, it should be noted that the main goal of treating patients with dysfunctional disorders of the biliary tract is to restore the normal flow of bile and pancreatic secretion through the biliary and pancreatic ducts. In this regard, treatment objectives include:
- restoration, and if impossible, replenishment of bile production (with the development of chronic biliary insufficiency, which is understood as a decrease in the amount of bile and bile acids entering the intestine 1 hour after the introduction of an irritant. Patients after cholecystectomy almost always develop dysfunction of the sphincter of Oddi, since from normal functioning of the biliary system excludes the gallbladder, and in connection with this, there is an irreplaceable loss of bile acids with the development of chronic biliary insufficiency, which causes both digestive disorders and dysfunctional disorders);
- increased contractile function of the gallbladder (if it is insufficient);
- decreased contractile function of the gallbladder (with its hyperfunction);
- restoration of the tone of the sphincter system;
- restoration of pressure in the duodenum (on which an adequate pressure gradient in the biliary tract depends).
Until now, diet therapy plays a significant role in the system of treatment measures. The general principles of the diet are a diet with frequent meals of small amounts of food (5-6 meals a day), which helps normalize pressure in the duodenum and regulates the emptying of the gallbladder and ductal system. Alcoholic drinks, carbonated water, smoked, fatty and fried foods, and seasonings are excluded from the diet - due to the fact that they can cause spasm of the sphincter of Oddi. When selecting a dietary diet, the influence of individual nutrients on the normalization of the motor function of the gallbladder and biliary tract is taken into account. Thus, with the hyperkinetic type of dysfunction, the consumption of foods that stimulate contraction of the gallbladder should be sharply limited - animal fats, vegetable oils, rich meat, fish and mushroom broths. With hypotension of the gallbladder, patients usually tolerate weak meat and fish broths, cream, sour cream, vegetable oils, and soft-boiled eggs well. Vegetable oil is prescribed in a teaspoon 2-3 times a day 30 minutes before meals for 2-3 weeks. To prevent constipation, dishes that promote bowel movement are recommended (carrots, pumpkin, zucchini, greens, watermelons, melons, prunes, dried apricots, oranges, pears, honey). This is especially important, since a normally functioning intestine means normalization of intra-abdominal pressure and the presence of normal movement of bile into the duodenum. The use of dietary bran (with sufficient water) is important not only for the functioning of the intestines, but also for the motility of the biliary tract, especially the gallbladder, which has sediment.
Among the drugs that affect the motor function of the gastrointestinal tract, the following are used: anticholinergic drugs, nitrates, myotropic antispasmodics, intestinal hormones (CCC, glucagon), choleretics, cholekinetics.
Anticholinergics , by reducing the concentration of intracellular calcium ions, lead to muscle relaxation. The intensity of relaxation depends on the initial tone of the parasympathetic nervous system, but when using drugs in this group, a wide range of side effects are observed: dry mouth, difficulty urinating, blurred vision, which significantly limits their use.
Nitrates (nitroglycerin, nitromint, sustonite, nitro-time, nitrong forte, nitro poppy, nitrocor, nitrosorbide, cardonite) through the formation of free nitric oxide radicals in smooth muscles, which activate the cGMP content, lead to their relaxation. However, these drugs have significant cardiovascular and other side effects. The development of tolerance makes them unsuitable for long-term therapy.
Non-selective calcium channel blockers (nifedipine, verapamil, diltiazem, etc.) are able to relax smooth muscles, including the biliary tract, but this requires the highest possible doses, which practically excludes the use of these drugs due to pronounced cardiovascular effects.
Some antispasmodics selectively block calcium channels (dicetel, panaveria bromide, spasmomen) and primarily act at the level of the colon, where they are metabolized. 5–10% of these drugs are absorbed and metabolized in the liver and can work at the level of the biliary tract. This aspect requires further research, and indirect effects associated with the restoration of the pressure gradient have been noted and can be used.
Currently, among the myotropic antispasmodics, the drug hymecromone (odeston) attracts attention, which has a selective antispasmodic effect on the sphincter of Oddi and the sphincter of the gallbladder. Odeston is effective in patients with dysfunction of the biliary tract, has a choleretic effect, eliminates biliary insufficiency, as well as dysfunction of the sphincter of Oddi, its hypertonicity, including in patients after cholecystectomy.
Among other myotropic antispasmodics, duspatalin should be noted, which selectively affects the tone of the sphincter of Oddi (directly and indirectly); it lacks a universal antispasmodic effect (and, therefore, side effects), but does not have a choleretic effect and in this is inferior to odeston.
For hypofunction of the gallbladder, the main approach to treatment should be pharmacotherapeutic.
The use of drugs that enhance gallbladder motility.
Choleretics:
- preparations containing bile or bile acids: allochol, dehydrocholic acid, lyobil, cholenzyme;
- synthetic drugs: oxafenamide, nicodine, cyclone;
- herbal preparations: hofitol, flamin, holagogum, corn silk, etc.
Cholekinetics: magnesium sulfate, olive oil and other oils, sorbitol, xylitol, holosas, etc.
The choice of drug, which is a very important, if not the main issue, depends on how quickly the effect of therapy is needed. If the fastest possible effect on the patient’s body is required, then it is better to use cholekinetics, and the effect depends on the dose of the drug; if a long course of treatment is necessary, then bile-containing drugs are used; if an anti-inflammatory effect is also required, then the choice should be made in favor of synthetic drugs, but the course of treatment with them will be short-lived; when the patient simultaneously has liver pathology, the choice should be made in favor of hophytol, which has a choleretic and protective effect.
Use of drugs with prokinetic effects
(motilium, debridate). This may also include myotropic antispasmodics: dicetel, spasmomen, duspatalin, halidor, no-spa. It should be remembered that their effects, as a rule, are indirect (they reduce either the tone of the sphincter of Oddi or the pressure in the duodenum). Their effectiveness is dose-dependent, so selection of an effective dose is necessary.
The use of drugs that reduce inflammation and visceral hyperalgesia. Nonsteroidal anti-inflammatory drugs: anopyrin, upsarin UPSA, dikloberl, naklofen, ketanov, solpaflex, brustan, ketonal, movalis, donalgin, ambene, celebrex and low doses of tricyclic antidepressants (amizol, saroten, elivel, melipramine, coaxil).
It is necessary to pay attention to other aspects of treatment. For dysfunction of the sphincter of Oddi: when establishing the first type, papillosphincterotomy is required; type two or three - the possibility of prescribing drug therapy is allowed. It should be borne in mind that hormones (CKC, glucagon) can temporarily reduce the tone of the sphincter of Oddi; Nitrates give a very short-term effect. Botulinum toxin is a strong inhibitor of acetylcholine release. Using it as an injection into the sphincter of Oddi reduces its pressure, improves bile flow and brings relief, but the effect of treatment is transient. For the pancreatic type of dysfunction of the sphincter of Oddi, the standard therapy is surgical sphincteroplasty and pancreatic lithoplasty (drug treatment is carried out only at the stage of absence of complications).
Conclusion
Recently, the attention of the medical community has been drawn to functional disorders of the gastrointestinal tract in general and the biliary system in particular. This is largely due to the fact that with regard to functional disorders there is still hope for their cure, as well as for successful prevention or delay in time of the development of organic pathology (including oncology) that is more severe in prognosis. Today, diagnostic approaches to the treatment of the diseases we have discussed, presented in this article, are being developed. In addition, this work reflects the large arsenal of medications at the disposal of the doctor, who has the opportunity to choose a drug or complex depending on the pathogenetic characteristics of a particular disorder.
Literature
- Sokolov L.K., Minushkin O.N. et al. Clinical and instrumental diagnosis of diseases of the organs of the hepatopancreatoduodenal zone. - M., 1987.
- Minushkin O. N. Dysfunctional disorders of the biliary tract (pathophysiology, diagnosis and treatment approaches). - M., 2002.
- Kalinin A.V. Functional disorders of the biliary tract and their treatment//Clinical perspectives of gastroenterology, hepatology. - 2002. - No. 3. - P. 25–34.
- Yakovenko E. P. et al. Dysfunction of the sphincter of Oddi associated with cholecystectomy (diagnosis, treatment) // Practitioner. - 2000. - No. 17. - P. 26–30.
- Nasonova S.V., Tsvetkova L.I. Experience of using odeston in the treatment of chronic diseases of the gallbladder and biliary tract // Ros. and. gastroenterology, hepatology, coloproctology. - 2000. - No. 3. — P. 87–90.
- Nasonova S.V., Lebedeva O.I. Odeston in the treatment of chronic diseases of the hepatobiliary system // Military Med. magazine. - 2001. - No. 3. P. 49–53.
- Yakovenko E. P. et al. Odeston in the treatment of diseases of the biliary tract // Practicing physician. - 2001. - No. 19. - P. 30–32.
O. N. Minushkin , Doctor of Medical Sciences, Professor, Medical Center of the Administration of the President of the Russian Federation, Moscow
Diagnosis and treatment
To make an accurate diagnosis, the gastroenterologist will need the results of the following studies: general and biochemical blood tests, ultrasound diagnostics of the liver and gallbladder, duodenal intubation, drug tests, cholecystography.
The therapeutic process of dyskinesia includes the use of drugs that stabilize the motor activity of the biliary tract. In addition, for a complete cure, it is necessary to follow a diet and normalize the psycho-emotional state.
Neurotic disorders can be corrected by creating comfortable conditions at home and at work, maintaining the correct daily routine, observing a psychotherapist, and taking sedatives or psychostimulants.
Nutritional Features
For the hypokinetic form of dyskinesia, it is recommended to consume foods rich in magnesium and plant fibers:
- buckwheat;
- bran;
- cottage cheese;
- cabbage;
- carrot;
- apples;
- vegetable oil;
- fatty dairy products.
You should also not forget about products that have a choleretic effect: sour cream, cream, vegetables, black bread, vegetable and butter, hard-boiled egg.
Compliance with dietary nutrition is the key to a speedy recovery
During an exacerbation of the disease, it is better to exclude the following foods: fatty meat and fish, smoked, fatty, fried, alcoholic drinks, confectionery, canned food, marinades, whole milk, legumes.
Products are best consumed boiled or baked. Steaming food is also beneficial. It is allowed to eat yesterday's bread, fermented milk products, lean meats and fish, cereals, vegetables, and vegetable soups.
Types of dyskinesia of the gallbladder
When bile moves quickly, we talk about hyperkinetic biliary dyskinesia; when bile moves slowly, we talk about hypokinetic dyskinesia. These types differ in symptoms, causes, and approaches to therapy. The hyperkinetic form is more typical for young patients, the hypokinetic form is more typical for people over 40 years of age.
There is another classification based on the characteristics of the tone of the duct sphincters. Hypermotor dyskinesia is observed in cases where the tone is increased, hypermotor - when there is a decrease in the contractile function of the circular muscles. Most often, the hypertensive type of disease corresponds to hyperkinetic, and the hypotonic type corresponds to hypokinetic.
It is important to understand that dyskinesia of the gallbladder is often not accompanied by organic changes in the ducts or gallbladder; only a disturbance in the movement of bile is observed. However, with this disease, the likelihood of developing secondary diseases, for example, inflammatory ones, increases.
Reasons for the development of dyskinesia
Consumption of excess fatty foods and irregular eating habits can lead to dyskinesia.
Disturbances in the functioning of the gallbladder and ducts develop over a long period of time. and in many ways they are associated with a violation of a healthy lifestyle. Among the main factors leading to dyskinesia are:
- Irregular meals, lack of breakfast and hot lunch. Most often, if there is no time to eat during the day, in the evening a person tries to catch up and overloads the digestive system.
- Consumption of excess fatty foods. It is fats that are broken down during bile processing, and its deficiency leads to various digestive disorders. These are constipation, diarrhea, other stool disorders, nausea, vomiting and other negative manifestations.
- Frequent consumption of so-called “junk food”: chips, sweet soda, fast food, etc. Such food gives practically nothing to the body, additionally burdens the digestive tract and negatively affects the functioning of the liver and gall bladder.
- Infestation with parasites. Giardia is a particularly common cause of damage to the gallbladder; if infection is detected, it is necessary to first eliminate the cause of the disease, and then deal with the symptoms.
Taking medications. The use of a large number of medications negatively affects the digestive system, the microflora is disrupted, and the load on the liver increases. All this leads to inhibition of the functions of the gallbladder.
Dyskinesia in children
Immaturity and lability of the nervous system can cause the development of ADHD in childhood. In children under one year of age, the disease is often a consequence of damage to the central nervous system during pregnancy or childbirth.
If we talk about older children, dyskinesia can be caused by stress, emotional overload, poor nutrition, physical inactivity, and food allergies. JVP in children manifests itself in the form of the following symptoms:
- the appearance of a white coating on the tongue;
- yellowness of the sclera;
- the appearance of cracks in the corners of the mouth;
- the skin acquires a white or even grayish tint;
- heartbeat disturbance.
The hypomotor form is treated with massage, water procedures and physical therapy. Tonic medicines have a good effect: Ginseng, Wild pepper extract, Aralia tincture, as well as magnesium preparations.
Basic methods of treating biliary dyskinesia
Small meals are necessary to normalize the patient's condition.
Treatment of hypotonic type DVT is carried out in several directions. Its goal: to stimulate the functioning of the biliary system; this requires a special diet. Products that help increase tone are mainly vegetables and fruits. A positive effect will be achieved by eating carrots, cabbage, apples, etc., in addition, tomatoes and green vegetables will help.
They are recommended to be consumed boiled or pureed: the food should not put a lot of stress on the digestive system. At the same time, indigestible foods are excluded from the diet: carbonated drinks and beer, spicy and fatty foods, etc.
Drug therapy will be aimed at increasing the tone and increasing the contractile function of the biliary tract: tincture of lemongrass, strychnine preparations, and sulpiride may be prescribed. In addition, sunflower and olive oil can be used for a relaxing effect. In case of exacerbation and sharp deterioration of the condition in the first 1-2 days, a gentle diet may be prescribed: the patient is given only drink - this can be rosehip decoction, weak tea, sweet natural juices. After this, for several days you can give only food that is most easily digested: pureed cereals and soups, boiled vegetables.
Small meals are necessary: the patient must be fed 5-6 times a day, but the portions should be small, and at least 2-2.5 liters of liquid must be drunk during the day. When the condition returns to normal, a simple gentle diet will be enough. For biliary dyskinesia, treatment with mineral waters is prescribed. In the hypokinetic form, highly mineralized waters have a healing effect: this is Morshyn water, as well as Essentuki No. 17 and some others.
To increase the effect of mineral waters, patients may be offered spa treatment. Therapy methods based on natural sources have successfully proven their effectiveness. They can be combined with physiotherapy: patients are prescribed electrophoresis or low-intensity ultrasound treatment.
Prevention
Do not forget to periodically undergo physical examinations
In order to prevent the development of the disease, it is necessary:
- Adhere to the principles of proper nutrition, eat only healthy, natural, high-quality products, and follow a meal schedule.
- Don't forget about physical activity.
- If you are overweight, you need to get rid of it.
- It is important to protect yourself from stress and negative emotions.
- Treat chronic diseases in a timely manner.
Characteristics of the disease
Gallbladder dysfunction is a fairly common problem.
Gallbladder dysfunction is a disease in which the organ's motility, that is, its ability to contract, is impaired.
As a result of these deviations, bile enters the duodenum in excess or insufficient quantities, which leads to disruption of the digestive process as a whole.
Excessive amounts of bile corrode the intestinal mucosa, contributing to the development of the inflammatory process.
With insufficient bile supply, incomplete digestion of food is observed, as a result of which undigested food is less well transported through the intestines, which also causes inflammation.
Bile is an important digestive element that helps break down complex fat molecules into simpler components. If the quantity is insufficient, this process is not fully carried out.
Brief medical history
Gallbladder dysfunction was first described in the scientific literature at the beginning of the 20th century by doctors who performed surgery on a patient suffering from severe pain in the right hypochondrium. Scientists were interested in the fact that when opening the patient’s abdominal cavity, no stones or other signs of pathology were found. After the operation, a thorough study of the disease began, which was ultimately identified as an independent disease.
There was some information about gallbladder dysfunction in earlier periods of time. In particular, even in ancient times, a connection was established between the symptoms of the disease and the emotional state of a person. Ancient scientists said that a person prone to aggression suffers from an excess amount of bile (dysfunction of the hypermotor type), and in people prone to melancholy and depression, on the contrary, insufficient production of this digestive element was detected (dysfunction of the hypomotor type).
Prevalence and significance
According to statistics, this disease accounts for about 12-13% of all organ diseases. It has been noticed that the disease develops more often in women; the fair sex faces the problem 10 times more often than men. Age and body characteristics also matter. The disease is more common in young women with insufficient body weight. Most often, the pathology develops against the background of other diseases of the digestive system. The most common form is hypomotor dysfunction.
Risk factors
Unfavorable factors that increase the risk of developing the disease include:
- Stress, emotional disturbances.
- Pregnancy.
- Inflammatory processes occurring in the organs of the digestive system.
- Surgical operations in the abdominal area.
- Hereditary factor.
- Chronic infectious diseases.
How to prevent violations?
Prevention of motor disorders of the biliary tract is as follows:
- A proper diet in which you should limit baking and fried foods, too much animal fat. You should not drink these foods with cold drinks. You cannot eat fast food, sauces and heavy soups, for example, with added cream.
- Avoiding stress and nervous situations.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.