Gallstone disease is a disease that affects a large number of people, mainly the elderly. According to various sources, in developed countries, up to twenty percent of the female population is affected, and up to ten percent of the male population. As its name suggests, this disease involves the formation of gallstones. There are many reasons for the occurrence of cholelithiasis. The main one can be considered a family predisposition; it can also be triggered by other diseases, for example, obesity or gout. A sedentary lifestyle and poor diet increase the risk of developing pathology. In this article we will look at the symptoms of cholelithiasis and methods of treating the pathology.
What factors contribute to the development of gallstone disease?
- Belonging to the female gender. According to statistics, women get sick 2-3 times more often than men. Pregnancy and childbirth also increase the chance of developing this disease.
- Age. The risk of developing the disease increases every year by 1% in women and 0.5% in men
- Hereditary predisposition.
- Excess body weight.
- Excessive nutrition with a predominance of fatty foods.
- Low-calorie diets.
- Lipid metabolism disorders.
- Hormonal disorders.
- Taking medications (fibrates, hormonal contraceptives, octreotide).
- Chronic diseases of the intestines and pancreas.
- Anatomical changes in the biliary system.
- Chronic inflammatory diseases of the biliary tract.
- Functional biliary disorders.
- Endocrinological pathology (diabetes mellitus, hypothyroidism).
If 2 or more points from this list are true for you, then you are at risk.
Don't take risks.
Contact a gastroenterologist for an initial examination.
Why is a doctor's examination necessary?
The first stages of gallstone disease are often not accompanied by pronounced symptoms or are asymptomatic for 10-15 years. The patient feels great and does not suspect that he already needs the help of a specialist.
By ignoring this, you lose the chance to suppress the disease with little effort and without serious consequences for the body.
Detection of violations of the composition of bile (the presence of thick bile in the gallbladder) during this period is perfectly treatable and prevents the formation of stones, which means it minimizes the risk of surgical intervention in the future!
Treating complications and advanced stages is longer, more difficult and more expensive.
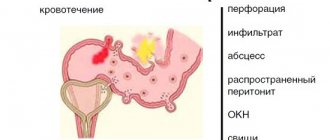
Possible complications
The duration of the disease, blockage of the bladder duct, and concomitant inflammatory processes can lead to dangerous consequences. List of possible complications:
- Pancreatitis;
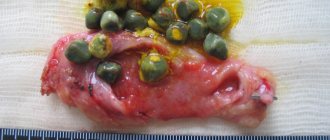
- Dropsy (accumulation of transudate) and empyema (accumulation of pus) of the bladder;
- Obstructive jaundice;
- Acute cholecystitis;
- Secondary biliary cirrhosis;
- Gall scars, fistulas;
- Mirizzi syndrome;
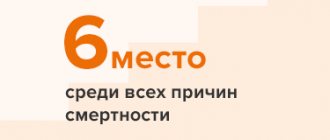
- Gallbladder cancer.
Acute cholecystitis is treated exclusively by surgery. It is caused by stone constipation in the bladder neck area and the onset of inflammation.
Untimely response leads to complications: peritonitis, empyema, gangrene, bladder perforation.
Stages of gallstone disease
Stage I - initial or pre-stone
At this stage, it is possible to identify thick heterogeneous bile in the gallbladder, the formation of biliary sludge, the presence of putty-like bile, and a combination of putty-like bile with microliths.
If you skip treatment at this stage,
gallstones begin to form.
If you start treatment
It becomes possible to normalize the rheological properties of bile. It is possible to prevent the process of stone formation and further development of the disease.
Patients diagnosed with stage I are advised to consult a gastroenterologist-hepatologist:
- to determine treatment tactics
- to control the properties of bile, functions of the gallbladder and biliary system
Stage II - formation of gallstones
At this stage, the examination reveals the presence of gallstones:
- in the gallbladder, in the common bile duct, in the hepatic ducts
- by number of stones: single, multiple
- composition: cholesterol, pigment, mixed
The clinical picture is determined - in what form the disease manifests itself:
- latent (hidden) course of the disease
- painful form with typical biliary colic
- dyspeptic form (the patient complains of a feeling of heaviness or a feeling of fullness in the right hypochondrium)
- gallstone disease occurs under the guise of other diseases
If you skip treatment at this stage,
in the future, surgical intervention will become inevitable.
If you start treatment
It becomes possible to dissolve cholesterol stones without resorting to surgery. Complications can be prevented.
Patients are advised to consult a gastroenterologist-hepatologist to prescribe treatment.
If there are indications, a gastroenterologist-hepatologist will schedule a joint consultation with a surgeon to determine further treatment tactics.
Stage III - chronic recurrent calculous cholecystitis
In case of frequent exacerbations of the disease, a joint consultation with a surgeon and a gastroenterologist-hepatologist is indicated to resolve the issue of surgical treatment and special preparation for surgery.
Stage IV - complications
A joint consultation between a surgeon and a gastroenterologist-hepatologist is indicated.
Principles of treatment of cholelithiasis
In modern biology, there are disagreements in approaches to the treatment of subclinical and asymptomatic forms of cholelithiasis. In such a situation, the doctor and the patient are faced with a dilemma: on the one hand, it is known that the earlier treatment is undertaken, the better the long-term result of cholecystectomy [13], on the other hand, the percentage of development of postoperative complications is high.
When discussing the issue of treatment of asymptomatic cholelithiasis, many authors express the opinion that lithotherapy is not indicated in this case, and the decision to conduct surgical treatment should be made by the patient himself, who should be familiarized with the indications, contraindications and possible complications during and after surgical treatment [14].
The risk of developing colic in patients with gallstones, initially asymptomatic, decreases with age, and cholecystectomy does not lead to a significant increase in life expectancy. In this regard, patients with “silent” stones do not require surgical treatment, but are subject to dynamic observation.
The situations given below are indications for treatment of patients with “silent” stones: • increased risk of developing gallbladder cancer in the presence of “porcelain” gallbladder (bladder wall calcification) and single stones with a diameter of more than 3 cm; • upcoming long stay in areas where there is no qualified medical care.
Symptoms
Very often, especially in the initial stages, cholelithiasis does not make itself felt and does not bother the patient. In more than half of patients, gallstones are discovered incidentally during examination for other diseases.
Symptoms usually appear at more advanced and dangerous stages of the disease. Therefore, if you observe any of the following, you are recommended to consult a gastroenterologist.
Minimal manifestations of cholelithiasis:
- heaviness in the abdomen (heaviness in the right hypochondrium)
- belching
- nausea
- constipation
- flatulence
Gallstone disease develops slowly over years. Her symptoms increase gradually. For several years, you may feel heaviness in the right hypochondrium after eating (especially when eating fatty, fried meat, smoked, salted, pickled foods, as well as wine). In the future, nausea, vomiting and sharp acute cramping pain in the right hypochondrium - hepatic colic - may join the unpleasant sensations.
If you observe a similar situation in yourself, do not put your health at risk and do not expect complications - consult a gastroenterologist.
Methods
1. Conservative treatment of cholelithiasis is possible only at an early stage. The doctor at the medical center prescribes treatment for gallstone disease. The patient's condition and the course of the disease are regularly assessed at follow-up appointments. Treatment of cholelithiasis without the use of drugs includes following a strict diet (Pevzner No. 5), actively reducing the patient’s weight and adding the necessary physical activity. The pharmacological method involves taking analgesics, antispasmodics, special preparations of bile acids and stimulating the regeneration of hepatocytes, under the influence of which the stone in the gall bladder dissolves. The use of litholytic therapy has many contraindications:
- Large diameter of stones (more than 1 cm);
- Obstructive jaundice;
- Acute cholecystitis;
- Kidney and liver dysfunction;
- Pregnancy.
Treatment of cholelithiasis without surgery is possible in an invasive way, thanks to shock wave extracorporeal lithotripsy. This method is suitable for patients whose gallbladder contractility is active, and the stone in the gallbladder is no more than 2 cm. Thanks to the shock wave, sediments and stones in the bladder are destroyed and come out on their own. As a result, the consequences of the disease are eliminated, but it does not work to eliminate the cause; the patient needs supportive therapy. After lithotripsy, a side effect is possible in the form of acute cholecystitis, severe biliary colic and the risk of a particle blocking the lumen of the biliary tract.
Treatment of gallstone disease without surgery, even if it is ultimately effective, does not eliminate the cause of stone formation, and relapse is possible.
2. Treatment of stones in the gall bladder is carried out using a radical surgical method, in the form of surgical removal of the entire gall bladder - cholecystectomy. The method ensures complete recovery of the patient. Cholecystectomy can be laparoscopic or endoscopic (single-port bladder removal).
The operation is performed under anesthesia. To perform laparoscopic cholecystectomy, 4 punctures are made in the abdominal wall, and a laparoscope and surgical instruments are simultaneously inserted into them. Surgical removal of the bladder is carried out in different ways - from the neck or from the bottom. The operation leaves minor damage and allows you to quickly restore your previous rhythm of life.
Treatment of calculous cholecystitis, in its uncomplicated form, can be carried out using single-port removal of the bladder (endoscopic cholecystectomy). The operation is performed through the smallest possible incision in the umbilical area, leaving a slight cosmetic effect.
The method of percutaneous cholecystolithotomy is also known - destruction and removal of stones through a single puncture in the abdominal wall. This option is relevant in some cases; stone formation often occurs repeatedly and with greater intensity.
Serious manifestations of cholelithiasis
This may be severe pain in the upper abdomen, which is accompanied by nausea and vomiting that does not bring relief (biliary or hepatic colic).
The symptoms described above may include: jaundice (mucous membranes and skin turn yellow), itching, change in urine color to a darker color, lightening of stool (blockage of the common bile duct with a stone is the most common complication of biliary colic)
If you experience these symptoms, it is highly likely that you have gallstone disease at an advanced stage.
The described complications require surgical intervention, because lead to death.
Unfortunately, some of the negative consequences of the disease will last a lifetime - even if you receive the highest quality medical care. After surgery to remove the gallbladder (cholecystectomy), approximately half of patients experience persistent pain, nausea and other unpleasant symptoms. This condition is called postcholecystectomy syndrome (PCES), and finding the cause of its development is the task of a gastroenterologist and ultrasound doctor. To solve this problem, an ultrasound method is used - dynamic echo-choledochography (ultrasound of the bile ducts).
Do not delay your visit to a gastroenterologist.
Take care of your health today!
Complications of gallstone disease
Patients often know that they have stones in their gall bladder. However, if the stones do not cause any symptoms, or these symptoms appear rarely and do not affect the quality of life, patients prefer not to pay attention to it.
If you do not pay attention to this, the very first attack of biliary colic can lead to very serious complications:
- Obstructive jaundice - stones from the gallbladder enter the ducts and prevent the flow of bile into the duodenum. Accompanied by acute, excruciating pain in the upper abdomen, yellowing of the eyes and skin, darkening of urine, and lightening of feces. This condition is dangerous because stagnation of bile occurs in the system of intrahepatic and extrahepatic bile ducts. Against this background, the liver is affected, and its cells begin to destroy (hepatitis develops). If bile stagnation continues for a long time, it leads to impaired liver function and subsequently to liver failure.
- Choledocholithiasis is the formation of stones in the bile ducts or their entry into the ducts from the gallbladder. A common complication, accompanied by increased pain, nausea, and vomiting, which does not bring relief.
Biliary colic is accompanied by the condition:
- Biliary pancreatitis. The pancreatic duct, through which enzymes are secreted, connects with the common bile duct and together, through one opening (the major duodenal papilla), they flow into the duodenum. The entry of stones into the common bile duct below the level of the confluence of the pancreatic duct is accompanied by the occurrence of inflammation of the pancreas.
- Stenosing pappilitis. This is a cicatricial narrowing of the large duodenal papilla, most often occurring against the background of its traumatization by small stones passing through it. The development of such a complication is accompanied by severe symptoms: frequent painful attacks, possible development of jaundice, pancreatitis, inflammation of the gallbladder and bile ducts.
- Cholangitis. This is an inflammation of the common bile duct. In this case, intoxication and fever are added to all the symptoms described above.
- Cholecystitis. Inflammation of the gallbladder. The most common complication. Accompanied by acute pain, nausea, vomiting, fever, intoxication
Other complications
Duspatalin in the treatment of patients with gallbladder pathology
When deciding on the prescription of myotropic therapy, we were faced with the need to use drugs that, on the one hand, would selectively relieve the pathological spasticity of the sphincter of Oddi without causing its atony, and on the other hand, would not aggravate the hypomotor dysfunction of the gallbladder. The myotropic antispasmodic mebeverine (Duspatalin) was chosen as such a drug. The advantages of the drug based on mebeverine hydrochloride, which influenced its choice, were: • relaxing selectivity with respect to the sphincter of Oddi, significantly (20–40 times) greater than the effect of papaverine, which is achieved by reducing the permeability of smooth muscle cells to Na+; • normalizing eukinetic effect on the smooth muscles of the intestine, helping to eliminate functional duodenostasis, hyperperistalsis, spasmophilia without the development of secondary hypotension due to an indirect decrease in the outflow of K+.
The effect after taking mebeverine occurs quickly (within 20–30 minutes) and lasts for 12 hours, which makes it possible to take it twice a day (prolonged form), while for elderly patients no dose adjustment is required. Thus, Duspatalin can be used for a long time in these patients , which is especially important for patients with sphincter of Oddi dysfunction after undergoing cholecystectomy.
Duspatalin in patients with dyskinesias of the gallbladder, especially of a cholestatic nature (primary spasms of the sphincter of Oddi, hyperkinesia of the gallbladder and their combination, dysfunction of the sphincter of Oddi after cholecystectomy), is usually prescribed 1 capsule (200 mg) 2 times a day 20 minutes before meals. The drug is almost completely metabolized in the intestinal lumen and absorbed in the form of inactive metabolites, so it does not give any secondary effect on smooth muscles, including the biliary tract.
In patients with pathology of the gastrointestinal tract, and cholelithiasis is no exception, concomitant dyskinesia of the stomach and duodenum, the phenomenon of duodenogastric reflux associated with gastroesophageal reflux, are often found. The high selectivity and tropism of Duspatalin to the sphincter of Oddi and intestinal smooth muscles make it possible to use it for the correction of duodeno-gastric and bile reflux. This is facilitated by the fact that mebeverine, by correcting gastro-duodenal motility, reduces the symptoms of duodenostasis, improving the passage of chyme and bile through the small intestine. However, it does not affect the tone of the lower esophageal sphincter, like other non-selective antispasmodics.
An important circumstance is that mebeverine does not act on the cholinergic system, and therefore does not cause side effects such as dry mouth, blurred vision, tachycardia, urinary retention, constipation and weakness. Mebeverine is effective and safe for long-term use in both young and elderly patients. The effect of the drug develops quickly (20–30 minutes after taking the capsule) and lasts for a long time (it is enough to take 1 capsule 2 times a day).
According to O.N. Minushkin (2002), a positive response to Duspatalin therapy is observed in 90% of patients with dysfunctional disorders of the biliary tract [15]. While taking the drug, relief of pain in the right hypochondrium is observed after 14 days in a significant proportion of patients with cholelithiasis (85%) and post-cholecystectomy syndrome (40%). According to ultrasound data, out of 11 patients with postcholecystectomy syndrome, who initially had a dilated (from 9 to 14 mm) common bile duct, in five, after 14 days of treatment with Duspatalin, normalization of its lumen was observed.
In our study, we carried out a clinical and functional assessment of the effect of mebeverine in 155 patients of all the groups listed above. In most patients, the clinical effect - relief of abdominal pain and dyspeptic (nausea) syndromes - was achieved when using the drug at a dose of 200 mg 2 times a day during the first days of treatment. By the end of the first week, there was a decrease in the severity of flatulence (which can be explained by the normalization of the outflow of bile, intestinal motility and digestion, primarily of fats). With repeated dynamic ultrasound of the abdominal organs, performed on the 10th day of treatment, in 68% of patients there was a decrease or normalization of the size of the gallbladder with a significant restoration of its contractility.
Analysis of the motor activity of the biliary tract, according to fractional sounding data during the use of Duspatalin, revealed a significant increase in the frequency of normosecretion of bile, as well as an improvement in the motor-tonic function of the gallbladder and sphincter apparatus: a significant increase in the frequency of registration of the phenomena of normokinesia of the gallbladder and normotonia of the sphincters of Oddi and Lutkens.
After a course of treatment with Duspatalin in the cystic and hepatic portions of bile, we observed a significant increase in the concentration of cholic acid, a slight decrease in the concentration of cholesterol and, accordingly, an increase in the cholate-cholesterol coefficient. In addition, during the use of Duspatalin in all patients, including cholelithiasis, an increase in the concentration of phospholipids and the phospholipid-cholesterol ratio was noted. This also indicated the positive effect of normalizing the motor-tonic function of the biliary tract, in this case with the help of the drug Duspatalin, on the positive dynamics of the main biochemical parameters of bile.
In what cases is it necessary to be examined?
- For chronic diseases of the gastrointestinal tract.
- If one of your close relatives suffers from cholelithiasis.
- With excess body weight.
- For rapid weight loss (for example, for the purpose of losing weight).
- In case of poor nutrition (eating 1-2 times a day, taking insufficient amounts of liquid, preferring fatty, fried, spicy, smoked, salty foods).
- In case of lipid metabolism disorders (hypercholesterolemia, dyslipidemia).
- With long-term use of fibrates, hormonal contraceptives.
- For anatomical abnormalities in the biliary system.
- For diabetes mellitus, thyroid diseases.
- After pregnancy and childbirth.
Any of the listed factors is a reason to consult a gastroenterologist-hepatologist. Don't expect complications.
Diagnosis of cholelithiasis
First diagnostic stage:
Consultation with an experienced gastroenterologist-hepatologist who will listen to you carefully, find out your medical history, conduct an objective examination, and determine the scope of the necessary additional examination.
Second diagnostic stage:
Laboratory and instrumental studies:
- general blood and urine test
- biochemical blood test
- scatological research
- fibrogastroduodenoscopy
The leading role in diagnosis belongs to ultrasound examination of the gallbladder, which makes it possible to determine the size and shape of the gallbladder, the thickness of its wall, the number of stones and their size.
Third diagnostic stage:
Based on the data obtained, the gastroenterologist will provide extended recommendations on diet, maintaining a healthy lifestyle, planned drug therapy, and, if necessary, refer you for a consultation with a surgeon.
Such diagnostics in our clinic helps the patient resolve the following issues:
- determining the stage of gallstone disease
- diagnosis and treatment of concomitant diseases
- Based on the results of the study, recommendations will be made on following a diet, maintaining a healthy lifestyle, and planned drug therapy, which will improve well-being and lead to recovery
- determination of indications for surgical treatment
Treatment - the possibilities of modern medicine
Meanwhile, today it is quite possible to prevent the development of complications of cholelithiasis. However, a cure can only be achieved through surgery, during which the gallbladder is removed along with the stones. Our clinic uses effective, low-traumatic techniques that allow you to quickly get rid of the disease. But you should know that currently existing methods for removing stones without damaging the organ itself are not effective.
The operation can be performed in two ways: using open cholecystectomy or laparoscopy. It is laparoscopic cholecystectomy that is recognized as the “gold” standard in the treatment of cholelithiasis. There are several types of laparoscopy, which differ from each other in the way they access the intervention area.
- Laparoscopic cholecystectomy - performed through several small, no more than a centimeter, punctures of the anterior abdominal wall;
- Transvaginal cholecystectomy using the NOTES method - access is performed through a centimeter incision in the posterior vaginal vault;
- Single-port laparoscopic cholecystectomy SILS - performed through a single puncture in the periumbilical area using a special port through which 3 instruments are inserted;
- Minilaparoscopic cholecystectomy - laparoscopy using mini-instruments up to 3 mm in diameter.
Each technique has its own advantages, but the common ones are low trauma, painlessness in the postoperative period and excellent cosmetic results. Thanks to the ability to visualize using modern video endoscopic equipment, intraoperative complications are minimized. Our patients return to their normal lifestyle within two weeks.
I actively use all of these methods in the surgical treatment of cholelithiasis. But for each patient, I choose the most suitable option, taking into account not only the size and number of stones, but also age, the presence of concomitant diseases, previous surgeries, etc.
Since 1994, I have performed more than 6,000 laparoscopic cholecystectomies, including more than 150 using the NOTES technique and more than 300 through a single puncture in the umbilical region. The experience I have accumulated is summarized in more than 30 peer-reviewed scientific publications, which are published in academic domestic and foreign publications. I described in detail the indications and technique of all types of operations for cholelithiasis in a monograph published in 2022 - SURGERY FOR GALLSTONIS: laparoscopy, minilaparoscopy, single port, transvaginal access, simultaneous operations. -M.: Publishing House "MEDPRACTIKA-M", 2022, 312 p. For more than 25 years, I have regularly conducted master classes on the surgical treatment of cholelithiasis.
Treatment of cholelithiasis
Treatment tactics depend on the stage of the disease
The most effective treatment method is treatment in the early stages, when the disease can be controlled by both non-drug (regimen, diet) and drug treatments.
In later stages, there is a high risk of developing serious complications that can lead to disability or even death. At these stages, surgical treatment is inevitable.
In stage I of cholelithiasis the following are indicated:
Consultation and observation of a gastroenterologist-hepatologist, during which you will receive prescriptions and recommendations:
- for an active lifestyle - physical exercise promotes the outflow of bile, eliminates its stagnation, and reduces hypercholesterolemia
- to normalize body weight
- for the correction of endocrine disorders (hypothyroidism, diabetes mellitus, estrogen metabolism disorders, etc.)
- to stimulate the synthesis and secretion of bile acids by the liver, normalize the physicochemical composition of bile.
In stage II of cholelithiasis the following are indicated:
Consultation and observation of a gastroenterologist-hepatologist, during which you will receive prescriptions and recommendations:
- in clinical nutrition
- to normalize body weight, combat physical inactivity
- for correction of lipid metabolism
- on medicinal dissolution of stones using bile acid preparations
In stage III of cholelithiasis the following are indicated:
Consultation and observation of a gastroenterologist-hepatologist, during which you will receive prescriptions and recommendations:
- on therapeutic nutrition and normalization of body weight
- for correction of lipid metabolism and drug dissolution of stones
- for relieving an attack of biliary colic
The decision on surgical treatment is made during a joint consultation with a gastroenterologist-hepatologist and a surgeon.
Stage VI of cholelithiasis - surgical treatment
To prescribe surgical treatment, a joint consultation with a surgeon and a gastroenterologist-hepatologist is required. During this consultation, tactics for such treatment will be developed and issues related to preparation for treatment will be resolved.
Indications for surgical treatment of patients with cholelithiasis are:
- acute calculous cholecystitis
- common bile duct stones
- gallbladder gangrene
- intestinal obstruction
- chronic calculous cholecystitis with a non-functioning gallbladder (“disabled” gallbladder)
The operation is also indicated in cases where early clinical symptoms of calculous cholecystitis appear (colic, fever, lack of stable remission between attacks).
The following types of treatment are currently used:
- open and laparoscopic cholecystectomy
- choledistolithotomy
- cholecystostomy
- papillosphincterotomy
The choice of treatment tactics is determined by the coordination of actions between the gastroenterologist-hepatologist and the surgeon.
Stages of treatment in stage IV gallstone disease
Non-surgical stage
A gastroenterologist guides the patient from the moment the very first asymptomatic signs of the disease are identified.
Why does the gastroenterologist together with the surgeon make the decision to remove the bladder?
At the EXPERT Polyclinic, a joint consultation is held between a surgeon and a gastroenterologist and further tactics are jointly determined.
Only a gastroenterologist has complete information about the condition of the patient’s gallbladder. When prescribing treatment (including prescribing surgery), factors such as:
- clinical manifestations
- duration of the disease and its stage
- size of stones, their number, factor of the presence of stones in the gallbladder ducts
- the number of biliary colics in the anamnesis, the presence of complications and concomitant pathologies
After clarifying all the above factors, it is possible to determine the treatment tactics for a particular patient.
Surgical stage
Removal of the gallbladder is carried out on a planned or emergency basis.
Planned surgical treatment
It is carried out after appropriate preoperative preparation, relief (suspension) of cholelithiasis complications using conservative therapy. The purpose of preparation is to adapt the patient’s body to the upcoming operation (remove inflammation in the gallbladder). In this case, removal of the gallbladder will occur with minimal consequences for the patient (the risk of postoperative complications is greatly reduced).
On an emergency basis
Surgeries are performed when complications of cholelithiasis develop, which without urgent intervention will lead to death. This type of intervention is considered the most traumatic for the body and recovery may take longer.
When deciding on planned surgical treatment, the gastroenterologist carries out the preoperative preparation stage.
Preparation minimizes the risks of complications and facilitates the course of a surgical procedure that is traumatic for the body.
Post-surgical stage
Accompanying the patient after surgery.
Periodic examinations are recommended during which a gastroenterologist monitors the patient’s condition and disease activity. This will allow the doctor to adjust treatment in time if post-surgical complications occur.
Why do you need the help of a gastroenterologist at the postoperative stage?
First of all, a specialist:
- will stop the development of complications of the postoperative stage (medication)
- will help the patient adapt to life without gallstones
- will create an individual diet for the patient
- will give recommendations regarding lifestyle
- will monitor the patient's condition using routine diagnostics. If complications recur, the gastroenterologist will prescribe appropriate treatment.
With the gallbladder removed, the patient needs constant regular monitoring, as this affects his quality of life.
Without the help of a gastroenterologist or if his recommendations are not followed, the life of a patient with postcholecystectomy syndrome can turn into a hellish series of diarrhea and unbearable abdominal pain.
In order not to fall into a wave of complications and further problems, these patients should not forget about the need for constant regular monitoring by a gastroenterologist.
If after surgical treatment the symptoms of cholelithiasis persist, this is an alarming sign in which it is necessary to consult a gastroenterologist as soon as possible. Most often, this is due to already developed complications of cholelithiasis and require timely diagnosis and proper treatment.
If the surgical intervention is performed on time (not for emergency reasons, before serious complications develop), then no discomfort will arise. However, this does not mean that after surgery there is a cure for cholelithiasis. Therefore, in order to prevent the re-formation of stones, only not in the gallbladder, but in the bile ducts, it is necessary to be observed by a gastroenterologist, undergo an annual examination, first of all, an ultrasound examination of the bile ducts (dynamic echo-choledochography) and, if necessary, conduct courses therapy.
Consequences after gallbladder removal
Why do you need the help of a gastroenterologist at this stage?
After cholecystectomy (removal of the gallbladder), postcholecystectomy syndrome may develop.
Occurs in 10-30% of patients undergoing surgery. This syndrome greatly affects the patient’s quality of life. For example, improper food intake provokes severe bouts of diarrhea and abdominal pain. People suffering from postcholecystectomy syndrome have to follow a strict diet and adjust their rhythm of life to it.
At this stage, the help of a gastroenterologist will make the patient’s life much easier. However, following all the doctor’s recommendations, in any case, requires enormous effort from the patient throughout his life.
More about postcholecystectomy syndrome
The development of postcholecystectomy syndrome is influenced by many factors, including the timeliness and quality of surgical treatment.
Postcholecystectomy syndrome includes functional disorders, organic lesions associated with relapse of the disease or concomitant diseases (chronic pancreatitis, peptic ulcer). Most often it manifests itself as persistent pain, sometimes nausea, bloating, belching, bitter taste in the mouth, heartburn, and diarrhea.
The risk of developing this syndrome is very high in those who had a complicated course of cholelithiasis and were operated on against the background of an inflammatory process as an emergency for health reasons. Moreover, the syndrome is organic in nature, and choosing adequate therapy to eliminate disturbing symptoms is usually not easy. To find out the exact cause of the development of PCES, dynamic echo-choledochography (ultrasound of the bile ducts) is used as the start of the examination.
If the gallbladder is removed as planned, after appropriate preoperative preparation, then the chance of developing postcholecystectomy syndrome is sharply reduced. And if disturbing symptoms arise, most likely they will be functional in nature, proceed more favorably and, if all the recommendations of the gastroenterologist are followed, will not affect well-being and quality of life.
Why is it recommended to treat cholelithiasis at the EXPERT Polyclinic?
What will you get by contacting us:
- effective and safe treatment
- modern diagnostic equipment
- gastroenterologists of the highest category, specializing in the treatment of this type of disease.
- joint consultation with a surgeon and a gastroenterologist
- an individual treatment program, in accordance with the condition of the disease and the characteristics of your body
When treating cholelithiasis, the doctor-curator of the EXPERT Polyclinic is ready to accompany you at all stages of treatment. From the initial consultation to the period of post-surgical intervention, you can always count on the help and support of your supervisor.
Treatment tactics for cholelithiasis
Therapy for the conservative management of patients with cholelithiasis, taking into account its pathogenetic features, should be determined in the following areas: • measures aimed at changing lifestyle, dietary nutrition, normalizing body weight; • drug litholysis using chenodeoxycholic (CDCA) and/or ursodeoxycholic (UDCA; Ursofalk) acids; • normalization of the outflow of bile, motility and digestion in the intestines.
The mechanism of action of UDCA is somewhat different from CDCA. If the first causes the dissolution of stones through the formation of liquid crystals (non-micellar dissolution of cholesterol), then the second - due to direct participation in the synthesis of bile acid-phospholipid micelles. UDCA slows down the absorption of cholesterol from the intestines and thereby reduces its pool in the body. In addition, when UDCA is prescribed, the amount of cholesterol used for excretion into bile clearly decreases. It is indicated that the drug affects litholysis in a “non-micellar” way and it undoubtedly turns out to be more effective than CDCA, in addition, it is better tolerated. Unlike CDCA, UDCA affects the formation of lecithin/cholesterol liquid crystals, which form in cholesterol-rich bile in the form of a “sandwich” and are located on the surface of a formed or forming stone. It is believed that cholesterol is used to form liquid crystals. With the combined use of CDCA and UDCA, their action is summed up and a clearer therapeutic effect is achieved. Some features of the clinical action of UDCA deserve attention. It turned out that it clearly reduces the manifestations of “biliary dyspepsia”, reduces the frequency and severity of attacks of hepatic colic and eliminates dyspeptic symptoms, which are sometimes quite pronounced in such patients. Treatment with litholytic agents can be effective only in the presence of floating, radiolucent (X-ray negative, calcium-free) stones with a diameter of less than 20 mm, mild symptoms and no signs of acute cholecystitis. In cases of complete and successful litholysis, patients require annual monitoring, with relapses more often occurring in the first 2–3 years. It is recommended to repeat courses of litholytic therapy periodically.
Conservative management of patients with cholelithiasis involves not only an impact on the quality of bile, but also an impact on the main pathogenetic moment - impaired bile secretion, which in most cases is functional in nature and is associated with concomitant dysfunction of the gallbladder, causing clinically significant manifestations of the disease (pain syndrome and dyspeptic symptoms).
We have sufficient experience (more than 300 patients) in studying the motor-tonic function of the biliary tract in patients with various pathologies (cholesterolitis, chronic cholecystitis, biliary dysfunction). All examined patients underwent fractional chromatic duodenal intubation, followed by examination of bile for lithogenicity and dynamic ultrasound of the biliary tract.
As a result of the studies, it was found that, regardless of the form of the disease, an increase in the lithogenicity of bile directly correlated with a violation of its outflow, detected during fractional probing. Moreover, the lithogenicity of bile significantly increased in the early stages of the development of biliary pathology - in 80% of patients with hypomotor functional disorders of the gallbladder. The presence of chronic cholecystitis, especially associated with opisthorchiasis, also significantly increased the lithogenicity of bile and was simultaneously accompanied by a deterioration in the motor-evacuation function of the gallbladder. It is characteristic that in almost all cases, hypomotor dysfunction of the gallbladder was observed against the background of hypertensive dysfunction of the sphincter of Oddi. The identified pathological motor-tonic relationships of the main functional links of the biliary tract predetermined the direction of treatment - an attempt to normalize these disorders using the existing therapeutic arsenal of myotropic drugs.
Prevention and lifestyle recommendations
- Compliance with the regime, diet: eating every 3-4 hours, excluding long periods of fasting, drinking enough liquid per day. A nutritionist will help you create the right nutrition program.
- Avoid fatty and fried foods, smoked foods, and strong alcohol.
- Include dietary fiber in your diet.
- Maintain an active lifestyle, exercise.
- Bring your body mass index to a normal value.
- Don't lose weight quickly, do it gradually.
- If possible, avoid taking medications that promote stone formation (oral contraceptives, antibiotics, fibrates).
- If you have diabetes, try to keep it in the compensation stage.
Dietary recommendations
- Sugar is a source of endogenous cholesterol and should be avoided.
- Increase your intake of proteins balanced in amino acid composition.
- Increase your intake of plant proteins: oatmeal and buckwheat, seaweed.
- Accustom yourself to regularly eating plant fibers.
- Avoid eating legumes, animal fats, and coffee.
- Skipping breakfast increases the risk of developing gallstones.
- Vitamins E and C reduce the likelihood of gallstone formation.
Unfortunately, in order to forget about gallstone disease in later stages, it is not enough just to follow the correct regimen and diet. Any doctor will tell you that “this is only an additional therapy, not the main treatment.”
If you have:
Nothing hurts. A deformation in the gallbladder was accidentally discovered
Deformation of the gallbladder is often related to anatomical features and can be asymptomatic for a long time. At the same time, there may be a violation of the outflow of bile from the gallbladder, oversaturation of bile with cholesterol, the formation of sediment, putty-like bile, and the formation of biliary sludge, which is the most important condition for the formation of gallstones. Over time, complaints may arise:
- for a periodic feeling of discomfort or dull pain in the right hypochondrium
- bitterness in the mouth
- flatulence
- unstable stool with a tendency to diarrhea.
In this case, an active lifestyle, physical exercise, and normalization of body weight are recommended. A consultation with a gastroenterologist is necessary in order to select drug therapy (if necessary), recommendations for proper nutrition, and further observation.
Nothing hurts. We accidentally discovered flakes, thick bile, and biliary sludge in the gallbladder
In approximately half of patients, biliary sludge does not cause any symptoms and is detected only by ultrasound of the gallbladder. Many patients do not attach importance to this pathology and do not consult a doctor. Meanwhile, the long-term existence of biliary sludge in more than half of patients can be complicated by biliary pancreatitis, dysfunction or stenosis of the sphincter of Oddi, acute cholecystitis, cholangitis, and gallbladder shutdown. 20% develop gallstones. To prevent the development of cholelithiasis and complications, timely consultation with a gastroenterologist-hepatologist is recommended. As a result, the causes that contribute to the formation of biliary sludge and the development of complications will be identified and eliminated.
There are complaints. Deformation of the gallbladder, flakes, thick bile, biliary sludge in the gallbladder were detected
If complaints arise, it is often not enough to make do with recommendations for lifestyle changes, moderate physical activity, and normalization of body weight. A consultation with a gastroenterologist is necessary in order to select drug therapy that will improve the excretion of bile from the gallbladder, relieve pain, prevent the formation of gallstones and the development of complications in the future, and, as a result, avoid surgical treatment in advanced cases.
The stones were identified a long time ago, but nothing bothers me
Latent (asymptomatic) stone carriage requires long-term observation by a gastroenterologist-hepatologist:
- to determine indications for gene therapy - medicinal dissolution of stones using bile acids (in the presence of cholesterol stones)
- for an ultrasound scan, which will determine the size and shape of the gallbladder, the thickness of its wall, the number of stones and their size
- to determine the dynamics of these indicators over time
If necessary, a joint consultation with a surgeon is held and indications for surgical treatment are determined.
There are complaints. Gallstones detected
Immediately consult a gastroenterologist, where a specialist will determine:
- indications for drug dissolution of stones
- will select therapy to relieve the patient’s complaints
- will reveal metabolic disorders underlying stone formation.
The success of conservative therapy for cholelithiasis is determined by strict adherence to recommendations and the correct selection of litholytic therapy. The effectiveness of treatment is monitored by a gastroenterologist-hepatologist using ultrasound examination, which must be carried out throughout the entire course of treatment. After completing the drug course of dissolving stones, in rare cases, relapse of stone formation is possible. Therefore, to prevent relapse, the gastroenterologist creates supportive and preventive therapy.
Heaviness, discomfort, pain under the “spoon” and in the right hypochondrium
These complaints are quite nonspecific and may be present in diseases of the liver, pancreas, stomach, duodenum, gall bladder (including cholelithiasis).
If you are concerned about heaviness, discomfort, pain in the pit of the stomach and in the right hypochondrium, you need to seek help from a gastroenterologist-hepatologist who:
- will find out the history of the disease
- will conduct objective research
- will determine the scope of necessary additional examination
There are stones, there was 1 colic
Mandatory observation by a gastroenterologist-hepatologist:
- to prescribe the necessary treatment
- to control the situation and constant monitoring
This simple measure:
- reduces the risk of recurrent colic
- prevents the development of disease and complications
There are stones, there were 2 colics
Repeated biliary colic, a relapsing course of the disease, increases the risk of complications and the risk of death by almost 4 times.
In this case, mandatory observation by a gastroenterologist-hepatologist together with a surgeon is indicated:
- to determine treatment tactics
- if necessary – to resolve the issue of surgical treatment
It is necessary to remove the gallbladder - what to do?
When preparing for a planned cholecystectomy, a joint consultation with a gastroenterologist-hepatologist and a surgeon is necessary:
- to determine the presence of indications and contraindications for surgical intervention
- if necessary - to draw up a plan for additional examination
In case of a decision on surgical treatment, it is important to perform a number of instrumental and laboratory tests, which are included in the standard examination before surgery.
The gallbladder has already been removed. Do I need to see a doctor, and which specialist should I see?
The gallbladder is an important organ of the gastrointestinal tract. In its absence, the following are often observed:
- change in hormonal function
- change in concentration function
- disorders associated with changed conditions of food absorption in the intestines.
This leads to disturbances in motility and secretory function of the stomach, ulcerative lesions of the stomach or duodenum, duodenitis, pancreatitis, intestinal lesions, disturbances in the metabolism of fat-soluble vitamins, protein and carbohydrate metabolism, fat metabolism and calcium metabolism.
Patients who have undergone cholecystectomy (that is, surgical removal of the gallbladder) require constant monitoring by a gastroenterologist-hepatologist.
In most cases, removal of the gallbladder does not relieve the patient of metabolic disorders underlying stone formation. The separated bile contains many cholesterol crystals and remains thick and viscous. After surgery, the pathological processes underlying cholelithiasis occur in new conditions: due to the absence of the gallbladder, the physiological function it performs is no longer possible, the motility of the biliary tract is impaired, and there is no regulation of the processes of bile formation and bile excretion.
Loss of the physiological role of the gallbladder, namely the lack of concentration of bile during the interdigestive period and its release into the duodenum during meals, is accompanied by impaired excretion of bile and indigestion. Changes in the chemical composition of bile and its chaotic entry into the duodenum disrupt the digestion and absorption of lipids, reduce the bactericidal properties of intestinal contents, which leads to microbial contamination of the duodenum and weakened growth of normal intestinal microflora.
In this regard, the patient may be concerned about:
- nausea
- vomit
- heartburn
- bitter feeling in the mouth
- flatulence
- unstable chair
- constipation
- frequent loose stools
- stomach ache
Excessive bacterial growth in the intestines leads to disturbances in protein, carbohydrate and fat metabolism, calcium metabolism and fat-soluble vitamins. This results:
- to frequent heavy diarrhea
- to weight loss
- to osteoporosis (disorders of bone mineralization)
- to vitamin deficiencies, which are manifested by loss of skin elasticity, fine wrinkles, peeling, depigmentation, dry skin, damage to the lips (hyperemia, swelling, peeling, formation of cracks and crusts, weeping in the corners of the mouth), damage to the tongue (ulceration of the papillae, the appearance of cracks), damage to gums (looseness and bleeding, weakening of teeth and their loss)
At least once every 4 months - with this frequency, regular observation by a gastroenterologist-hepatologist and ultrasound of the bile ducts (dynamic echo-choledochography) after cholecystectomy are recommended for early diagnosis of possible complications.
A year after removal of the gallbladder, the same symptoms appeared: pain in the right side, nausea, loose stools
In patients after removal of the gallbladder, the existing clinical manifestations may be associated with a number of factors:
- changes in the chemical composition of bile
- impaired excretion of bile into the duodenum
- impaired motility of the biliary tract
- excessive growth of pathogenic microflora in the intestines
- disruption of food digestion and nutrient absorption
In this case it is necessary:
- consultation with a gastroenterologist-hepatologist
- specialized ultrasound examination (dynamic echo-choledochography)
- subject examination
- complex treatment
- further long-term follow-up
Pathogenesis of cholelithiasis
According to modern concepts, the formation of gallstones is mainly the result of destabilization of the physicochemical state of bile. The process of stone formation requires the presence of three factors: 1) secretion of “lithogenic” (supersaturated with cholesterol, calcium or bilirubin) bile by the liver; 2) the presence of “nuclei” for subsequent crystallization; 3) stagnation of bile in the gallbladder (GB), providing conditions for the growth and fusion of crystals with the formation of stones.
There are many known factors that contribute to stone formation. Endogenous factors include primarily gender and age. An important role in the formation of cholelithiasis is played by impaired metabolism, in particular calcium, which is involved in the regulation of all types of metabolism (protein, carbohydrate and fat), and excess body weight, which is detected in the vast majority of patients. It is known that overweight individuals suffering from cholelithiasis have increased activity of the enzyme hydroxymethylglutaryl-coenzyme A reductase (HMG-CoA reductase), which is involved in the biosynthesis of cholesterol in the liver [7]. GSD is often associated with various congenital anomalies of the biliary tract (BDT) and duodenum (DU), which impede the outflow of bile. Opisthorchiasis, functional disorders of the biliary tract, chronic hepatitis of various etiologies, liver cirrhosis, and dyslipidemia increase the risk of developing GSD. Diseases accompanied by chronic hemolysis (hemolytic, sickle cell anemia, spherocytosis, hemolytic activity of Escherichia coli) are of great importance in the formation of pigment stones [8].
Of the exogenous factors, the main role is played by dietary habits, mainly associated with an increase in the consumption of highly refined foods, rich in fat and animal proteins, but depleted in indigestible dietary fiber. A certain role in the formation of cholelithiasis should be assigned to certain medications, such as fibrates, contraceptives, estrogens during menopause, progesterone, octreotide, ceftriaxone. According to many authors, when the regulation of the activity of the hepatic microsomal enzyme acetyl-Co-A-cholesterol acetyltransferase is impaired, the esterification of hepatic cholesterol decreases. Contraceptives, hormonal drugs, clofibrate, as well as increased estrogen levels in women during pregnancy are potential inhibitors of this enzyme [9].
The supposed “trigger mechanisms” are also numerous: an imbalance in the system of the enzymes HMG-CoA reductase and 7α-hydroxylase, which regulate the synthesis of cholesterol and its conversion into bile acids; a decrease in the level of cytochrome P450, which is involved in hydroxylation processes; changes in the content of lysolecithin, cholesterol, mucin, taurocholate, etc. [9]. The classical theory of lithogenesis, based on a complex including lipid metabolism disorders, inflammation and bile stagnation, has not lost its significance [10].
Among the endogenous factors of stone formation, great importance has recently been attached to mutations and polymorphism of several genes, in particular the mutation of the MDR3 gene for the phospholipid transport ATPase. This mutation is especially common in young patients (under 40 years of age) with recurrent choledocholithiasis after cholecystotomy, low levels of serum phospholipids and, as a consequence, a reduced intake of phospholipids into the bile, leading to impaired stability of cholesterol-containing micelles and stone formation. In addition to the described mutation, anomalies of other genes are also found in cholelithiasis: CYP7A1; ABCC7(CFTR); SLC10A2(IBST); APO-E4;CCKAR, as well as the so-called lithogenic genes (Lith 1–5), found in chromosomal loci and capable of causing cholelithiasis [11]. The growth of microcrystals is a long process, takes a long time, it is facilitated by a pronounced decrease in the motor function of the gallbladder (in 70% of patients), as a rule, a weakened response to cholecystokinin , as well as increased secretion of mucin by the mucous membrane of the gallbladder. Gallstones are formed by a combination of exogenous and endogenous factors.
Treatment stories
Story No. 1
Patient T., 42 years old, contacted a gastroenterologist at the EXPERT Clinic with complaints of decreased appetite, nausea, bitterness in the mouth, heaviness and pain in the right hypochondrium after eating. From the medical history it is known that after giving birth 15 years ago, she gained 23 kg in body weight, eats irregularly, loves sweets and fatty foods. For the last 3 years she has been taking hormonal contraceptives. From the life history it was possible to find out that the patient’s mother and grandmother suffer from cholelithiasis (GSD). Both were operated on. When examining the patient, attention was drawn to grade 2 obesity, mild pain on palpation of the right hypochondrium, and a coated tongue. During the consultation, an ultrasound of the abdominal organs was performed, where it was established that there was a single cloud-like formation occupying 1/3 of the volume of the gallbladder with its compaction
Clinical manifestations of chronic calculous cholecystitis
Primary chronic calculous cholecystitis is an inflammatory disease that affects the walls of the gallbladder and is associated with the presence of stones in it. The disease may not be clinically manifested, but more often there are dyspeptic disorders, pain in the right hypochondrium with radiation to the back, right shoulder blade, right shoulder, provocation of pain by fatty and fried foods, as well as an accompanying constant feeling of bitterness in the mouth. Associated changes in the oral cavity are characteristic in the form of changes in the color of the tongue, the appearance of areas of desquamation, the growth of individual areas of the epithelium of the tongue, the appearance of grooves on the back of the tongue. Eating large amounts of fat may be accompanied by the presence of a thick coating on the tongue and a decrease in taste. In addition to changes in the tongue, chronic pathology of the gallbladder and gallbladder in cholelithiasis is often accompanied by bleeding gums and various forms of gingivitis.
All of the listed symptoms, while not being specific in themselves, can serve as an indication for cholecystectomy in the detection of stones in the gallbladder, but do not exclude the possibility of conservative treatment, including with the help of agents that improve the motor-tonic function of the gallbladder and affect the lithogenicity of bile.
The progressive course and danger of complications are indicated by the frequent recurrence of clinical symptoms, their protracted nature and high intensity. Eventually, the symptoms of the disease become permanent.
If a progressive course of cholelithiasis is suspected, certain data can be obtained during a clinical examination: • upon palpation or percussion of the abdomen in the area of the right hypochondrium, increased pain and a symptom of muscle protection; • positive symptoms of Ortner, Kehr, Murphy, etc.