Typically, the operating team includes 4–5 surgeons, and the intervention lasts 4–5 hours. The prognosis greatly depends on how correctly the operation is performed. It is important to carefully adhere to modern standards. Surgeries for pancreatic cancer are not the case when improvisation and original techniques are appropriate. Is it always possible to perform the operation?
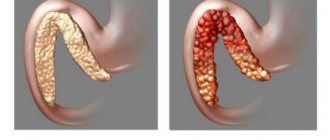
Surgery is the only method that can potentially cure exocrine pancreatic cancer. Unfortunately, in only one out of five patients is surgical treatment possible in principle - in the other four, at the time of diagnosis, the tumor has already managed to grow strongly into the surrounding tissues and give metastases. But even in this one out of five cancers it is not always possible to remove the cancer. Sometimes, having already begun the operation, the surgeon discovers that resection is impossible.
Distal pancreatectomy
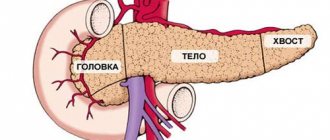
The pancreas consists of three parts: head, tail and body. During distal resection, part of the body and tail are removed. Often the spleen is removed at the same time. Such operations are usually performed for neuroendocrine tumors, which originate from cells that produce insulin and other hormones. By the time of detection, exocrine cancer most often grows into neighboring tissues, gives metastases, and surgical treatment becomes impossible. After removal of the spleen, the body’s defenses are reduced, and the patient becomes more vulnerable to infections.
Relevance of pancreatic body resection
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
Removal of the gland body is sometimes a forced measure, which should not be resisted for the sake of maintaining overall normal health. Unlike the tail and head parts, the body is cut along the line of the lower edge. This means that the posterior side of the peritoneum is taken as the starting point.
This is followed by a bypass from below the pancreas to carefully free it from the built-up fiber. Only after this can we move on to studying the vessels and spleen. As soon as the sphincter is applied, it is allowed to cross the corresponding section of the organ.
To protect the mesenteric vessels, the surgeon will definitely use a Kocher probe. And if there was heavy bleeding during the process, then it is intercepted with the help of so-called mosquitoes, and then completely bandaged.
The distal part is required for resection, after which the doctor cuts a flap from the omentum to cover the proximal segment. This means that the cut out soft fabric should cover the piece located closer to the center. The result is a subtotal operation, when only the problematic part is excised.
For the success of transverse resection, a purse-string suture is used, which perfectly covers even an extensive wound surface.
Pancreaticoduodenectomy (Whipple procedure)
This surgery has traditionally been performed on most patients with exocrine pancreatic cancer. During the intervention, the head of the pancreas (sometimes along with the body), the gallbladder, part of the bile duct and intestines (sometimes along with part of the stomach), and nearby lymph nodes are removed. Then the remaining ends of the intestine are connected to each other or to the stomach, and the end of the bile duct and the pancreas are sutured to the intestine. This is a very difficult operation. In order to perform it successfully, the surgeon must operate on 15–20 such patients annually. But even in this case, 5% of patients die due to complications of the operation. If the surgeon is not experienced enough, the mortality rate is 15%.
The Whipple operation can be performed in different ways:
- Most often, a large incision is made in the middle of the abdomen.
- Some clinics practice laparoscopic interventions through punctures in the abdominal wall. This requires special equipment, and doctors must have the appropriate skills.
Main complications after pancreaticoduodenectomy:
- infections;
- failure of sutures on the intestine;
- bleeding;
- indigestion, which requires taking pancreatic enzyme medications;
- obstruction at the junction of the stomach and intestines;
- bowel dysfunction;
- weight loss;
- diabetes mellitus (when a lot of endocrine tissue is removed, insulin production is disrupted).
Recovery
Surgeries for malignant pancreatic tumors are extensive and traumatic, so the patient will need care. In the first 2-3 days he will be in intensive care. If everything is in order, the patient is transferred to a specialized department.
In order to avoid complications such as thrombosis, adhesions and pneumonia, early mobilization is recommended if there are no contraindications. At first, the patient simply needs to turn over in bed and perform special exercises and breathing exercises. To reduce the load on the seam area, they can be supported with a pillow. After the patient gets stronger, he is allowed to sit and get out of bed for short walks. At this stage, you can already use a postoperative bandage. On average, hospitalization varies between 2-4 weeks, depending on the method of surgery (laparoscopic and laparotomy).
After pancreatectomy, all patients lose weight. It takes 1.5–3 months for the digestive system to adapt to new working conditions. Throughout this period, you must strictly follow the recommendations regarding diet. If the gland is completely removed, these restrictions will have to be adhered to for life, as well as taking hormone replacement and enzyme medications.
Extended gastropancreaticoduodenectomy
Recently, the attitude of doctors towards the Whipple operation has changed, not for the better. It is not effective enough because micrometastases often remain in the lymph nodes, which the surgeon does not remove during the intervention. In the USA, Japan and Europe, another operation is now more often performed: extended gastropancreaticoduodenectomy. During it the following is removed:
- pancreas;
- part of the stomach and small intestine;
- gallbladder;
- part of the bile ducts;
- nearby lymph nodes;
- part of the portal vein and artery affected by cancer;
- retroperitoneal lymph nodes.
Severtsev Alexey Nikolaevich
Doctor of Medical Sciences, Professor, Surgeon-Oncologist
“You need to operate as soon as the diagnosis is made. Pancreatic cancer is very aggressive, it quickly becomes inoperable, and the prognosis deteriorates sharply. Unfortunately, in Russia there are not many clinics that perform radical operations for pancreatic cancer, and not everywhere the complication rates and survival rates correspond to American and European ones.”
Rehabilitation period
After removal of the pancreas, a person’s life changes dramatically. Even if only the tail of the organ or another part of it was removed, and the operation itself went without complications, the patient will need a lot of time and effort to fully recover.
If the patient follows all the doctor’s recommendations, the rehabilitation period in 90% of cases proceeds without serious complications
If the pancreas is removed, the patient will have to follow a strict diet, take special medications and use insulin injections to ensure control of blood sugar levels.
Many patients complain for a long time that they have pain in the operated area, and the pain is severe. And to minimize them, doctors usually prescribe painkillers as additional therapy. Full recovery of the body after pancreatic surgery takes about 10–12 months.
Palliative operations
If pancreatic cancer cannot be removed, some surgical interventions are available to help improve the patient's condition:
- If the outflow of bile into the bile ducts is impaired, a stent can be installed - a hollow frame with a mesh wall made of metal or plastic. Stenting can be performed during percutaneous transhepatic drainage
or
retrograde cholangiopancreatoduodenography
(RPG). - Biliodigestive anastomosis
is the creation of a communication between the bile duct and the intestine, bypassing the pancreas. - Gastrojejunostomy
- creation of a connection between the stomach and jejunum.
Medical indications
Many victims of destabilized pancreatic function do not agree to undergo partial excision - resection until the very end, believing that the resulting disability will ruin their life. Doctors insist that modern pharmacology, coupled with a competent approach to the recovery period, works almost miracles. If the victim adheres to a certain set of rules of behavior and nutrition, then after the operation he will come to his senses quickly and will again be able to work and do what he loves.
Many people are frightened by the fact that diabetes mellitus is among the possible side effects of surgery. But, according to statistics, this complication occurs only in 50% of clinical cases.
Before referring a person for resection, the doctor will definitely do everything to avoid radical measures. This even applies to situations where the patient is diagnosed with a neoplasm. First, the treating specialist must make sure whether it is benign or malignant. For this purpose, auxiliary diagnostic formats are used, such as computed tomography with contrast or biopsy. The latter allows you to determine the exact type of tumor found. Pancreatectomy also helps determine the type of treatment.
If the treatment program with standard medications did not produce the expected results, or was rejected from the very beginning due to insufficient productivity, then resection is prescribed. Before her, the victim is sent to undergo a series of tests:
- electrocardiogram;
- radiography;
- coagulogram;
- blood tests, including biochemical;
- ultrasound examination of the abdominal cavity;
- endoscopy.
Having received the results of all the listed examinations, the expert takes note of the current complaints of the applicant, his medical history and other data from the medical card, including hereditary disposition. Based on the information collected, a person may be prescribed a partial resection, which is a mandatory measure if:
- exacerbation of chronic pancreatitis;
- mechanical injury;
- destruction of the integrity of the organ, which is associated with rupture and crushing;
- neoplasms of a malignant nature such as carcinoma;
- cyst formation;
- the presence of a fistula;
- necrotic tissue pathologies.
Sometimes the reason for transfer to the inpatient gastroenterology department for surgery is some rare acquired or congenital disease, which is more related to atypical manifestations.
Library
POSSIBILITIES OF SURGICAL TREATMENT OF PATIENTS WITH CANCER OF THE PANCREAS AND PERIAMPULAR ZONE
Patyutko Yu.I., Kotelnikov A.G., Mikhailov M.M., Kosyrev V.Yu. FSBI "National Medical Research Center of Oncology named after. N.N. Blokhin" of the Ministry of Health of Russia
The authors work in the surgical department of liver and pancreatic tumors of the Federal State Budgetary Institution "National Medical Research Center of Oncology named after. N.N. Blokhin" of the Russian Ministry of Health. For any questions you may have, please contact the leading researcher of the department, Ph.D. Kotelnikov Alexey Gennadievich tel. 324-17-70
Surgical treatment of patients with cancer of the pancreas and organs of the periampullary zone (distal common bile duct, major duodenal papilla, duodenum) is represented by the following main types of surgical operations:
- standard gastropancreaticoduodenectomy (subtotal pancreaticoduodenectomy, Whipple operation);
- pancreatectomy (total pancreaticoduodenectomy);
- distal (left-sided) resection of the pancreas;
- extended gastropancreaticoduodenectomy (extended subtotal or total pancreaticoduodenectomy, regional subtotal or total pancreaticoduodenectomy).
In addition, a number of operations have been developed: pylorus-sparing pancreaticoduodenectomy, resection of the head of the pancreas with preservation of the duodenum and biliary tract, economical (wedge-shaped) pancreaticoduodenectomy, duodenectomy, transduodenal papillectomy, distal pancreatic resection with preservation of the spleen (3, 8, 11, 13 , 14). All of them are performed for functional reasons, their oncological adequacy is extremely doubtful, and they are classified as relatively rare operations.
Standard GPDR (gastropancreatoduodenal resection), performed for biliopancreatoduodenal cancer, is an operation that has become the property of many surgical and oncology clinics. Standard GPDR includes: resection of the common bile duct, resection of the gastric outlet with the adjacent lesser and right half of the greater omentum, removal of the head of the pancreas and the entire duodenum. The removed complex includes the tissue adjacent to the head of the pancreas and the fascial-cellular sheaths of the common and proper hepatic artery, the upper mesenteric and portal veins. Lymph nodes of the following regional groups are removed:
- No. 1 - pyloric, No. 2 - around the common bile duct, No. 3 - along the upper edge of the head of the pancreas, No. 4 - along the lower edge of the head of the pancreas, No. 5 - anterior pancreaticoduodenal, No. 6 - posterior pancreaticoduodenal, No. 7 - proximal mesenteric lymph nodes.
The technique for performing all stages of standard GPDR has now reached a certain limit and is well presented in the literature (2, 3, 4, 9). Mobilization of the removed complex, the reconstructive stage of the operation, a set of surgical and conservative measures aimed at preventing complications from the pancreatic stump and pancreatic anastomosis - all this currently determines the postoperative period with a minimum number of fatal complications.
Without dwelling in detail on the methodology for performing standard GPDR in the Russian Cancer Research Center, it is advisable to note the features of the operation, which mainly determine the absence of complications in the postoperative period from the pancreatic stump and pancreaticojejunostomy.
These features are as follows:
- refusal to suture the pancreatic stump tightly or introduce filling materials into the pancreatic duct
- the most gentle manipulations on the pancreatic stump
- separate suturing of the pancreatic duct into the wall of the jejunum (the method for forming the anastomosis is presented below) with a minimum number of sutures without external pancreaticojejunostomy.
The method of forming pancreaticojejunostomy in the Russian Cancer Research Center: the anastomosis is formed “end to side”, the jejunum closer to its mesenteric edge is fixed with three separate sutures to the posterior wall of the pancreatic stump, a hole is formed in the intestinal wall, equal in diameter to the pancreatic duct, then only 4 threads are inserted through the walls of the pancreatic duct, capturing the corresponding walls of the intestine over the edge of the opening in the intestine.
After passing the last, 4th thread through the anterior wall of the duct and the anterior edge of the opening in the intestine, the stitched structures are brought together and the threads are tied in the sequence in which they were passed. Those. The last one to tie is the 4th, front, ligature.
A synthetic, slowly absorbable suture material 4/0, 5/0 on an atraumatic needle is used. The pancreatic stump is covered with the wall of the intestine involved in the anastomosis with separate atraumatic sutures using 3/0 thread. The pancreatic duct is not sutured into the intestine only in rare cases when it is not visualized without magnifying optics. Then the pancreatic stump is sewn into a hole in the wall of the jejunum of a slightly larger area and is also covered with a second row of separate sutures. A small number of sutures between the pancreatic duct and the opening in the intestine ensures reliable sealing of the anastomosis without disturbing its trophism and the unhindered flow of pancreatic secretions into the intestine.
In the surgical department of liver and pancreas tumors of the Russian Cancer Research Center, from 1990 to 1999, 135 standard GPDR were performed for tumors of the biliopancreaticoduodenal zone of various origins. The immediate results of the operation do not depend on the histological structure and localization of malignant tumors in the organs of the bipancreatoduodenal region.
Complications developed in 56 patients (41.5%), 10 patients died (7.4%). Among the last 55 patients operated on under standard GPDR since 1995, 1 patient died, mortality rate 1.8%. The nature and frequency of individual complications after standard GPDR: failure of pancreaticojejunostomy - 11 (8.1%) patients, failure of choledochojejunostomy - 8 (5.9%), bleeding from acute ulcers of the gastrointestinal tract - 8 (5.9%), intra-abdominal abscess - 6(4.4%), pneumonia - 6(4.4%), acute postoperative pancreatitis - 5(3.7%), external jejunal fistula - 5(3.7%), erosive bleeding in the surgical area - 5(3.7%), external pancreatic fistula - 4(2.9%), pancreatic necrosis - 2 (1.5%), adhesive intestinal obstruction - 2 (1.5%), pnvmatorax - 2 (1.5% ), myocardial infarction, pulmonary embolism, sepsis, mesenteric thrombosis, acute cardiovascular failure - 1 (0.7%) complication each. The causes of death in 10 patients were: pancreatic necrosis - 2 patients, acute postoperative pancreatitis, bleeding from acute ulcers of the gastrointestinal tract, bleeding in the surgical area, abscess pneumonia, myocardial infarction, pulmonary embolism, mesenteric thrombosis, acute cardiovascular failure.
Long-term results of standard GPDR were assessed based on the median life expectancy after surgery. Survival for 1, 2, 3, 4, 5 years was calculated by a direct method based on tracking of patients over different periods. Actuarial calculation methods were not used due to overestimation of survival rates. Survival was studied only among patients with histologically proven adenocarcinoma. Moreover, histological data were reviewed in patients with pancreatic cancer whose life expectancy was about or more than 2 years. In three cases, this allowed us to reject the diagnosis: adenocarcinoma of the head of the pancreas. Long-term results of patients with cystadenocarcinomas, tumors of a neuro-endocrine nature, metastatic and non-epithelial tumors of the biliopancreaticoduodenal region have not been assessed. Of the 135 patients who underwent standard GPDR, 23 patients were operated on for cancer of the head of the pancreas. Of these, 3 patients died in the early postoperative period from complications; in 4 patients, surgery was performed for macroscopically detectable liver metastases or extensive retroperitoneal tumor invasion, i.e. was obviously palliative in nature; finally, in one patient the tumor was cystadenocarcinoma, which, as is known, determines a more favorable course of the disease. In the remaining 15 patients, the tumor of the head of the pancreas had the structure of adenocarcinoma. A routine pathological examination of the removed specimen made it possible to qualify the extent of the disease as follows: pT 1-2 N 0-1M 0 (in accordance with the TNM classification adopted by the International Union Against Cancer until 1997). The median life expectancy of 15 patients operated on for adenocarcinoma of the head of the pancreas was 9 months. (See Table 1). There is no three-year survival rate. All patients died from disease progression.
Of the 135 operated patients, only 4 patients underwent standard GPDR for cancer of the distal common bile duct. A routine pathological examination of the surgical material revealed that in all cases the tumor had the structure of adenocarcinoma and grew into the head of the pancreas; only one patient (25%) had a metastatic lymph node adjacent to the common bile duct. The median life expectancy in this group was 8 months. There is not even one-year survival rate yet (see Table 1).
Of the 135 patients who underwent standard GPDR, 58 were operated on for cancer of the major duodenal papilla. Of these 58 patients, 7 patients died in the early postoperative period; in 2 patients, surgery was performed in the presence of liver metastases. Finally, the last 6 patients were operated on within the last six months and were also excluded from the long-term survival analysis. A planned pathological examination of the removed specimen made it possible to qualify the prevalence of cancer among 42 patients as follows: pT 1-2N 0M 0 - 22 patients, pT 3-4N 0M 0 - 12 patients, pT 2N 1M 0 - 2 patients, pT 3N 1M 0 - 6 patients . Those. in 43% of patients the tumor spread to the pancreas, only 19% had metastases to regional lymph nodes. The median survival rate in the entire group of patients was 27 months, 5-year survival rate was 23% (see Table 1).
14 patients were operated on for duodenal cancer. Of these 14 patients, long-term survival was analyzed in 11, since in 2 patients standard GPDR was obviously palliative in nature, and 1 patient still has a short follow-up period after surgery. A routine pathological study found that in 64% of those operated on the tumor infiltrated the head of the pancreas, and in 9% metastases were found in regional lymph nodes. The median life was 34 months, 5-year survival rate was 33% (see table No. 1).
Table 1
Life expectancy after standard GPDR for cancer of the head of the pancreas, distal common bile duct, major duodenal papilla, and duodenum.
| Localization of cancer | Median (months) | 1 year | 2 years | 3 years | 4 years | 5 years |
| Head of the pancreas | 9 months | 33% | 27% | — | — | — |
| Distal common bile duct | 8 months | — | — | — | — | — |
| Major duodenal papilla | 27 months | 85% | 50% | 30% | 27% | 23% |
| Duodenum | 34 months | 100% | 60% | 56% | 38% | 33% |
The above data demonstrate the acceptable tolerability of standard GPDR. Long-term survival depends on the location of adenocarcinoma: unsatisfactory survival after standard GPDR for resectable cancer of the head of the pancreas and distal common bile duct, relatively good survival for cancer of the major duodenal papilla and duodenum, which is consistent with some literature data (10).
For cancer of the body and tail of the pancreas, a so-called distal, or left-sided, resection of the pancreas is performed. The operation is accompanied by the removal of the spleen. The volume of the pancreas removed varies from resection of the tail of the pancreas, which corresponds to 25% of the volume of the organ, to subtotal resection - 75-90% of the volume of the pancreas is removed. Given the extraorgan spread of pancreatic cancer, surgery may involve resection and removal of surrounding organs. This allows the intervention to be classified as non-standard combined operations. The procedure for performing the operation is covered in sufficient detail in the literature (1, 4, 5).
Since 1990, the Russian Cancer Research Center has performed 36 distal pancreatic resections. Based on the volume of resection of pancreatic tissue, all of them can be classified as half left-sided and subtotal resections of the organ. In the first case, the transection of the pancreas is carried out along the left contour of the superior mesenteric vein, at the level of the body of the pancreas, with subtotal resection - at the level of the head, to the right of the superior mesenteric vein. The operation was always accompanied by splenectomy. Distal resection of the pancreas, splenectomy with removal or resection of adjacent organs was performed in 11 patients. In this case, the following were removed or resected: the left kidney, left adrenal gland, stomach, colon, diaphragm. In 2 patients, the operation included resection of the superior mesenteric vessels. The operation was accompanied by complications in 7 (19.4%) patients, mortality - 2.7%. Frequency and nature of individual complications: subphrenic abscess - 3 (8.3%) patients, bleeding from acute ulcers of the gastrointestinal tract, acute postoperative pancreatitis, pancreatic necrosis, pneumonia, acute postoperative psychosis - 1 (2.7%) complication each. The cause of death in the only patient who died was bleeding from acute ulcers of the gastrointestinal tract. Of the 36 patients operated on, 15 patients had pancreatic cancer. Of the latter, in 3 patients the histological structure of the tumor corresponded to neuroendocrine cancer, in 1 patient it corresponded to cystadenocarcinoma. These 4 patients, due to the biologically more favorable structure of the tumor, were excluded from the analysis of long-term survival. One more patient was not included in the survival analysis due to the significant prevalence of pancreatic cancer and the obviously palliative surgery. The median life expectancy among 10 patients was only 6.6 months, 33% of patients lived for 1 year, and no one lived for 2 years. All patients died from disease progression. The minimum life expectancy among those who underwent resection of the superior mesenteric vessels and adjacent organs was 4 months.
Thus, from the presented data it is clear that distal resection of the pancreas for adenocarcinoma of the body or tail of the pancreas is a rather complex, but completely tolerable operation. Long-term survival is unsatisfactory.
Unsatisfactory long-term results of surgical treatment in the form of standard GPDR for patients with cancer of the pancreatic head and distal common bile duct, a significant incidence of locoregional relapses after surgery, indication in the literature of good long-term results after extended GPDR for cancer of the pancreatic head and periampullary zone, reported by Japanese researchers (6,7,12) - all this was the basis for the accumulation of their own experience of expanded GPDR in Russia.
Extended GPDR, in addition to the pancreaticoduodenal complex with regional lymph nodes removed during standard GPDR, involves resection of the pancreas at the border of the body and tail of the organ, removal in a single block of connective tissue adjacent to the pancreaticoduodenal complex, lymphatic vessels and nodes, nerve plexuses, fascial-cellular sheaths of all large vessels within the following boundaries: upper - the level of the aortic opening in the diaphragm, lower - the level of the inferior mesenteric artery, right - the gate of the right kidney, left - the left renal pedicle. Within these limits, skeletonization of all large arteries and veins is carried out. In this case, the preparation contains lymph nodes of both the regional and juxtaregional lymph collectors. The latter includes groups of lymph nodes: No. 8 - along the upper edge of the body of the pancreas, No. 9 - along the lower edge of the body of the pancreas, No. 10 - around the common hepatic duct, No. 11 - around the celiac trunk, No. 12 - around the superior mesenteric artery, No. 13 - around the middle colonic vessels, No. 14 - para-aortic group of lymph nodes. If invasion of the superior mesenteric vein is suspected, the latter is resected with its simultaneous plasty. The reconstructive stage of the operation does not differ from that of standard GPDR. Similar operations have been performed at the Russian Cancer Research Center since 1997. 13 extended GPDRs were completed. In three cases, the operation was accompanied by resection of the superior mesenteric vein.
The average duration of extended GPDR was 7 hours 27 minutes ± 1 hour 32 minutes, the average blood loss was 3233 ± 1067 ml. For comparison: standard GPDR time is 4 hours 48 minutes ± 36 minutes, blood loss is 1815 ± 632 ml
Complications developed in 12 patients—92%; no one died from complications in the early postoperative period. The nature and frequency of individual complications: failure of pancreaticojejunostomy - 4 (31%), postoperative diarrhea - 12 (92%), failure of hepaticojejunostomy, external small intestinal fistula, external pancreatic fistula, erosive bleeding in the surgical area, diabetes mellitus - 1 each (7.7 %) complication, bleeding from acute ulcers of the gastrointestinal tract - 2 (15.4%), subphrenic abscess - 2 (15.4%). When comparing complications among patients who underwent GPDR in two variants, a significantly higher level of complications was noted among those who underwent extended GPDR (t = 5.8). The significant difference is due to the higher incidence of postoperative diarrhea among those who underwent extended surgery. Diarrhea is a consequence of intestinal denervation during skeletonization of the superior mesenteric vessels. The incidence of pancreaticojejunostomy failure is also higher after extended than after standard surgery, although the difference is not statistically significant. It can be assumed that the high incidence of complications (31%) is associated with distal transection of the pancreas and deterioration of the blood supply to its stump.
The low quality of life of operated patients in the late stages after surgery is noteworthy: poorly corrected diarrhea, severe weight loss, and edema syndrome are inevitable companions of patients for at least six months after extended GPDR. Of the 5 patients who died after extended GPDR for more than 2 months, three had high intestinal obstruction caused by locoregional relapse and peritoneal carcinomatosis.
The implementation of extended GPDR was accompanied by a more in-depth pathological study of the complex removed during the operation.
Five extended GPDRs were performed for cancer of the head of the pancreas. In 3 patients there was tumor invasion of the mesenteric vessels, in 2 of the 5 operated patients, resection of the superior mesenteric vein was performed. On average, 35 regional and juxtaregional lymph nodes were subjected to microscopic examination. In all (100%) patients operated on for cancer of the head of the pancreas, metastases were detected in regional lymph nodes; in 80%, metastases were found in the lymph nodes of the juxtaregional collector. Of the 5 patients operated on for cancer of the head of the pancreas, 4 died within the following periods: 2, 6, 7, 14 months. The median life expectancy was thus 6.5 months. One patient lives after surgery for 6 months without signs of disease progression. Of the deceased, only one patient died 2 months after surgery from liver abscesses. Three others died from progression of the disease. A pathological examination of one of them revealed a relapse in the surgical area and multiple liver metastases.
For cancer of the distal common bile duct, extended GPDR was performed in one patient. A thorough pathological examination of the removed specimen revealed tumor invasion into the head of the pancreas and cancer metastases into the lymph nodes of the regional and juxtaregional groups. The patient died from generalization of the disease after 8 months.
For cancer of the major duodenal papilla, 5 extended GPDRs were performed. In 2 out of 5, the tumor spread to the head of the pancreas, the N1-regional lymph collector was affected by metastases in 80%, the N2-juxtaregional lymph collector was affected by cancer metastases in 60% of those operated on. Of the 5 operated patients, one patient died after 19 months. The rest live: 18, 14, 6, 2 months. Moreover, the first of them had a locoregional relapse and metastases to the mediastinal and peripheral lymph nodes.
Based on the above, it can be stated. The effectiveness of surgical treatment of patients with biliopancreatoduodenal cancer depends: firstly, on the histological structure of the tumor, and secondly, on its location. Gastropancreatoduodenal resection, both standard and extended, performed for adenocarcinoma of the pancreas and distal common bile duct, does not lead to any significant increase in the life of patients. The results of a thorough, unusual, pathological study of removed specimens, the presence of locoregional relapse and distant metastases in patients after surgery indicate the already widespread nature of the disease at the time of surgery and cast doubt on the capabilities of extended GPDR as a method of preventing locoregional relapse. This also applies to distal pancreatic resections for adenocarcinoma of the organ.
Apparently, real improvement in long-term results of treatment of patients with cancer of the pancreas and distal common bile duct should be sought by combining surgical and chemoradiotherapy methods of treatment.
Bibliography
1. Buriev I.M., Ikramov R.Z. Distal pancreatectomy. Annals of surgical hepatology. 1997, volume 2, pp. 136-138.
2. Egiev V.I., Rudakova M.N. Pancreatoduodenal resection for periampullary cancer. Annals of surgical hepatology. 1997, volume 2, pp.82-87.
3. Lapkin K.V., Pautkin Yu.F. Biliopancreatoduodenal cancer. M., publishing house UDN, 1991, 112 p.
4. Patyutko Yu.I., Kotelnikov A.G. Pancreatic cancer: diagnosis and surgical treatment at the present stage. Annals of surgical hepatology. 1998, volume 3, no. 1, pp. 96-111.
5. Dalton RR, Saar MG, van Heerden JA, Colby TV Carcinoma of the body and the tail of the pancreas: is curative resection justified? Surgery, 1992, v.111, p.489-494
6. Ishikawa O., Ohhigashi H., Sasaki YO et al. Practical usefulness of Lymphatic and Connective Tissue Clearance for the Carcinoma of the Pancreas Head. Ann.Surg., 1988, v.208, p.215-220
7. Ishikawa O. Surgical Technique, Curability and Postoperative Quality of life in an Extended Pancreatectomy for Adenocarcinoma of Pancreas. Hepatogastroenterology, 1996, v.43, No. 8, p.320-325
8. Kimura W., Morikane K., Futakawa N. et al. A new method of Duodenum-Preserving Subtotal Resection of the Head of the Pancreas based on the Surgical Anatomy. Hepatogastroenterology, 1996, v.43, p.463-472
9. Lygidakis NJ Reconstruction of Alimentary Continuity after Subtotal Duodenopancreatectomy. Hepatogastroenterology., 1996, v.43, p.971-979
10. Michelassi F., Erroi F., Dawson PJ et al. Experience with 647 Consecutive Tumors of the Duodenum, Ampulla, Head of Pancreas and Distal Common Bile Duct. Ann.Surg., 1989, v.210, No. 4, p.544-556
11. Pradere B., Julia CH, Rimailho J., Bloom E. Et al. Pancreatectomies gauches avec conservation de la rate sans son pedicle. Ann. Chir., 1992, v.46, No. 7, p.620-624
12. Shirai Y., Tsukada K., Ohtani T., Hatakeyama K. Carcinoma of the Ampulla of Vater: Is Radical Lymphadenectomy Beneficial to Patients with Nodal Disease? Journal of Surgical Oncology. 1996, 61, p.190-194
13. Takada T., Yasuda H., Uchiyama K., Hasegawa H. Duodenum-preserving pancreatoduodenostomy. A new technique for complete excision for head of the pancreas with preservation of biliary and alimentary integrity. Hepatogastroenterology, 1993, 40(4): 356-359
14. Traverso LW, Longmire WP Preservation of the pylorus in pancreaticoduodenectomy. Surg. Gynecol. Obstet., 1978, v. 146, p.959-962.
Possible consequences in the postoperative period
The consequences of removing the pancreas can vary. Any surgical intervention has a high risk of developing inflammatory or infectious processes in the tissues of the body in the postoperative period. And to avoid them, the doctor prescribes a course of antibiotics before and after the operation. If the patient takes them strictly according to the prescribed regimen, the risks of such complications are reduced several times.
After removal of the gland, diabetes mellitus develops, because after the operation there is an acute lack of insulin in the body, which is why the person is forced to constantly take insulin injections. If you skip them or use them incorrectly, this is also fraught with various consequences, among which is hypo- and hyperglycemic coma.
In addition, even the removal of a small part of the pancreas disrupts its exocrine functions responsible for digestion. Therefore, the patient will also have to constantly take enzyme preparations (they are prescribed on an individual basis).
Drugs used as replacement therapy after removal of the pancreas