Causes of intestinal spasms
There are many reasons for spasms
Intestinal spasm involves contraction of the fibers of the lining of the small or large intestine. There can be many causes of spasm, but correctly identifying the cause will help to correctly prescribe treatment and avoid relapse.
- Eating stale food. Along with spoiled food, various pathogenic bacteria can enter the body, causing the development of infection in the intestines. This can lead to cramps.
- Regular overeating, habit of quickly swallowing food. Those who like to overeat at night and eat in a hurry often experience intestinal spasms, because food entering the stomach is poorly digested, which increases the load on the intestines.
- Stress. Spasms in the intestines, the causes of which lie in stress, are very common. Oddly enough, this is one of the most common causes of painful cramps. It is long-term stress and constant nervous overload that provoke contractions of intestinal muscle tissue.
- Viruses. Various viral infections disrupt the intestinal microflora, causing disruptions in the gastrointestinal tract. Taking antibiotics only makes the situation worse. Dysbacteriosis occurs, accompanied by painful spasms, diarrhea, and sometimes nausea.
- Helminthiasis. Helminthiasis, or simply worms, is a disease accompanied by abdominal pain, intestinal cramps, diarrhea, vomiting, and weight loss. Parasites can enter the body through dirty water, unwashed vegetables and fruits, or in the absence of the habit of washing hands.
- Heavy metal poisoning. Salts contained in heavy metals, when ingested, cause contraction of intestinal smooth muscles.
- Functional disorders. Cramps in the intestines can be symptoms of the development of gallstones, liver diseases and other disorders.
- Sedentary lifestyle. Low physical activity provokes irritable bowel syndrome. In this case, the patient is worried about pain caused by cramps in the intestines, flatulence, and false urge to defecate. The root cause of these disorders is a sedentary lifestyle, rest and computer work.
Causes of severe abdominal pain
The content of the article
There are many possible causes of sudden severe abdominal pain. The most common of these are intra-abdominal or pelvic diseases, for example:
- appendicitis;
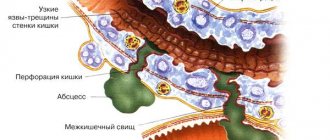
- perforation of the gastrointestinal tract;
- colon diverticulosis;
- acute gastroenteritis;
- biliary colic;
- acute cholecystitis;
- acute cholangitis;
- acute pancreatitis;
- stones in the kidneys;
- acute pyelonephritis;
- acute cystitis;
- mesenteric artery embolism;
- thrombosis of visceral veins;
- abdominal aortic aneurysm.
In addition, in women, acute abdominal pain can cause:
In women, acute abdominal pain can cause
- acute adnexitis;
- ectopic pregnancy;
- torsion or cyst of the appendages.
Sometimes sudden severe abdominal pain is a symptom of metabolic or non-abdominal diseases, such as:
- myocardial infarction;
- inflammation of the heart muscle or pericardium;
- pneumonia and pleurisy;
- pulmonary embolism;
- increased levels of calcium in the blood;
- crisis of the thyroid gland or adrenal glands;
- food hypersensitivity;
- porphyria;
- ketoacidosis.
There are many more causes of acute abdominal pain, so diagnosing the cause of the pain can be quite difficult.
Symptoms accompanying intestinal spasms
Often spasms are accompanied by other symptoms
Depending on the cause of the spasms, they are usually accompanied by other symptoms of a particular disease or disorder. Symptoms appear together or sequentially one after another. The whole picture will allow the doctor to make the correct diagnosis:
- Abdominal pain. Pain is the key symptom that determines intestinal spasm. The pain can be either severe or not very intense, recurring, increasing or constant. Sometimes, due to the nature of the pain, a spasm can be confused with intestinal colic.
- Flatulence. Flatulence and bloating along with intestinal cramps can be symptoms of irritable bowel syndrome. This diagnosis is usually made when these symptoms recur over several months.
- Diarrhea. Diarrhea and cramps may indicate both irritable bowel syndrome and dysbiosis caused by a viral infection. The doctor will make an accurate diagnosis after performing the necessary tests.
- Urge to defecate. Sometimes spasms are accompanied by a false urge to defecate, which does not lead to the desired relief. In fact, the spasm itself is the cause of tenesmus. The smooth muscles of the colon contract, causing a sensation of “twisting” in the abdomen and a false desire to go to the toilet.
- Feeling of insufficient bowel movements. Many people are familiar with this feeling of unfinished bowel movement when in fact the process has already been completed. If this is accompanied by cramps, there is a possibility of developing irritable bowel syndrome. However, if there are other symptoms, such as bleeding during bowel movements, pain in the anus, this may be a sign of more serious diseases: polyps in the intestines, tumors, internal hemorrhoids.
- Nausea. Nausea itself is a sign of gastrointestinal dysfunction. Nausea and cramps can be symptoms of two different diseases that accompany each other (gastritis and dysbiosis) or one disease that combines them (irritable bowel syndrome, colitis).
- Menstrual pain. Pain in the lower abdomen during menstruation in women is often accompanied by cramps in the intestines and even diarrhea. Typically, such disorders are observed in young nulliparous women. With the birth of the first child, the pain often stops.
How does a doctor diagnose sudden severe abdominal pain?
How a Doctor Diagnoses Sudden Severe Abdominal Pain
A doctor diagnoses acute abdominal pain based on patient-reported symptoms and a physical examination of the abdomen.
Sudden severe abdominal pain is just a nonspecific symptom of many diseases. Therefore, it is necessary to diagnose the cause of the pain. This usually requires performing laboratory tests (including morphology, C-reactive protein, urinalysis, and others depending on the specific clinical situation) and imaging tests.
The main imaging study is abdominal ultrasound. Sometimes other tests, such as a CT scan of the abdomen, or an X-ray of the abdomen or chest, may also need to be done.
Ask and choose
How can a pharmacy client choose an over-the-counter antispasmodic from the extensive list of drugs for abdominal pain? Guiding questions will help:
- Does a person have a chronic organic gastrointestinal disease - peptic ulcer of the stomach or duodenum, chronic cholecystitis, chronic pancreatitis, biliary colic, biliary dyskinesia? As a rule, the patient already knows what helps him or what drug the doctor recommended for him during an exacerbation.
- Patient's age? Selective M-anticholinergics are not suitable for the elderly due to the risk of developing intestinal obstruction. Also, antispasmodics have age restrictions for children: mebeverine can be used from twelve years of age, hyoscine butylbromide and drotaverine - from six, trimebutine - from three.
- For women - pregnancy, lactation? The use of antispasmodics during pregnancy is possible only as prescribed by a doctor. PDE inhibitors and trimebutine are contraindicated during lactation. Anticholinergics and sodium channel blockers can be used during lactation.
- Pain in the upper abdomen, possibly accompanied by nausea or vomiting? A selective M-anticholinergic drug is suitable for adults, in the absence of contraindications described in the instructions for a particular drug.
- Pain in the lower abdomen? Type IV PDE inhibitors and sodium channel blockers are suitable.
Sources
- Abdominal pain syndrome in the practice of general practitioner T. M. Benz “News of medicine and pharmacy.” Gastroenterology (239), 2008.
- Pchelintsev M. V. “Anspasmodics: from clinical pharmacology to pharmacotherapy.” Attending Physician 7 (2008): 74–77.
- Mikhailov I. B. Clinical pharmacology (textbook for students of medical universities) - 5th ed., revised. and additional - St. Petersburg: publishing house "Sotis-Med", 2013. - 588 p.
- Yakovenko E. P., et al. "Opiate receptor agonist trimebutine in the treatment of functional disorders of the gallbladder and sphincter of Oddi." Journal "Attending Physician" 2–2014 (2017): 56.
- Tytgat GN. Hyoscine butylbromide: a review of its use in the treatment of abdominal cramping and pain. Drugs 2007; 67:1343–57.
Acute stomach
Symptoms : sudden cramping or constant abdominal pain (local or diffuse), nausea, vomiting, dry mouth, severe tension in the abdominal muscles.
Article on the topic Emergency call. When should you not hesitate to see a doctor?
Diseases that cause similar symptoms:
Acute appendicitis, strangulated hernia, acute cholecystitis, perforated ulcer of the stomach and duodenum, acute intestinal obstruction, acute pancreatitis, ectopic pregnancy, peritonitis.
Acute abdomen is the most dangerous condition, which indicates a catastrophe in the abdominal cavity. Most diseases that cause symptoms of an acute abdomen require immediate medical attention. With peritonitis, acute appendicitis, perforated gastric ulcer, the clock counts. Therefore, patients with an acute abdomen are immediately sent to the surgical department of the hospital.
Remember:
- in case of acute pain, food and liquid intake is prohibited;
- painkillers can blur the picture, making diagnosis difficult;
- any amateur activity in the form of enemas and laxatives can lead to a tragic outcome.
Not always gastritis. When does abdominal pain indicate problems with blood vessels? More details
What to do:
— The patient needs to be laid down, put ice wrapped in a towel on his stomach (any product from the freezer will do), and wait for the doctor to arrive.
There are a number of diseases that simulate acute abdomen. These are pneumonia (when the focus is in the lower part of the lung), renal colic, pyelonephritis, heart failure, injuries to the ribs, spine, and pelvic bones.
Functional pathology accompanied by smooth muscle spasms
00:00
Alexander Sergeevich Trukhmanov , professor, doctor of medical sciences:
— The floor to Valery Mikhailovich Makhov for a report on the topic: “Functional pathology accompanied by spasms of smooth muscles.”
Valery Mikhailovich Makhov , professor, doctor of medical sciences:
— Thank you, dear Alexander Sergeevich, dear Oksana Mikhailovna, dear listeners.
The end of the twentieth century was marked by the fact that functional pathology of the gastrointestinal tract (GIT) received citizenship rights. This is a situation where the symptoms of the disease and clinical manifestations are completely inexplicable when conducting modern endoscopic and biochemical studies.
The complexity of this situation lies in the fact that it is difficult not only for the doctor to understand how the clinical symptoms do not correspond to the generally accepted cellular theory, and why certain manifestations are not reflected in biochemical and other studies.
It is especially difficult for patients who cannot understand how their anxiety and suffering are not at all associated with certain abnormalities identified during instrumental studies.
Functional pathology in its classification gradation is based precisely on symptoms. Based on these data, we can say for sure that approximately 40–60% of patients seeking help from gastroenterologists and general practitioners, with careful clinical, biochemical, and instrumental studies, demonstrate that they have a functional pathology.
The most basic functional pathology that occurs with complaints coming from the intestines is irritable bowel syndrome (IBS).
Please note that a mandatory criterion for the presence of IBS is pain or what patients perceive as discomfort when they cannot articulate that it is pain.
Recent recommendations have lowered the time criteria required before this diagnosis can be made. It is very important that these pains stop after passing stool or gas. This patient necessarily has some kind of deformation of the stool. Either it is oak-shaped, hard stool, or liquid stool.
03:19
(Slide show).
IBS is a very, very common phenomenon. These numbers are somewhat outdated. Now it is believed that 15 - 20%. But these statistics are not very accurate. Based on the data of the American Gastroenterological Association, the statistics of this association showed that:
• in the USA, 20 million patients are diagnosed with IBS;
• a third of them turn to gastroenterologists;
• 12% or more percent are patients of general practitioners.
Recently, the criteria have paid a lot of attention to changes in stool quality. This, of course, is not a very aesthetic conversation with the patient. But you need to ask very carefully how often bowel movements occur. It is very important what character the chair has.
It makes sense to emphasize to the patient that normal bowel movements are considered to be 1-2 bowel movements every 24 to 48 hours. When a patient complains of constipation, be sure to ask what he means. In the previous post we got the criteria for constipation very clearly.
(Slide show).
It is probably very useful to have the Bristol Stool Rating Scale in front of you so that the patient can figuratively explain what kind of stool he has. Those stools that can be regarded as stool corresponding to constipation are types 1 and 2. Types 5 and 7 are the types that correspond to diarrhea.
In addition to these complaints, it is very important that patients can talk very colorfully about the presence of imperative urges. These imperative urges, which are reflected not only in medical literature, but also in fiction, are called “bear disease.”
A significant proportion of patients say that they cannot restrain the passage of feces when excited. Students - before exams. Clerks - before going to the authorities and so on.
It is very important to interpret such a symptom as a feeling of incomplete emptying. This is a very scary symptom, because this can hide a very serious pathology, ranging from intestinal tumors and even hemorrhoids. Sometimes it is necessary to differentiate this particular symptom.
06:17
In IBS, this symptom is caused by increased sensitivity of the rectal mucosa to the pressure exerted by feces. A very frightening symptom for our patients is the release of mucus during bowel movements. With their characteristic sense of fear and increased impressionability, they can say that they are secreting worms. They may even say that their gut has prolapsed when the mucus is cylindrical in shape.
In addition to these symptoms, there are a number of others that characterize these patients as people with a fantastic sensitivity to these symptoms.
The classification of IBS, like other functional pathologies, is entirely based on symptoms. Divided by:
• IBS with constipation;
• IBS with diarrhea;
• Mixed IBS, when half is half;
• Unclassified IBS, when it is impossible to clearly determine the predominance of a particular syndrome.
Despite the ease of diagnosis, it is impossible to diagnose IBS without conducting studies that would confirm the absence or presence of organic pathology. This is an irrigoscopy or colonoscopy with a biopsy, regardless of whether anxiety syndromes appeared, like blood in the stool, and so on. These studies are required. Without this, it is impossible to make a diagnosis of functional pathology.
(Slide show).
We have already noticed that these patients are very impressionable. This situation is reflected in the results of a study of the quality of life of these patients. All the quality of life scales—pain, general health, psychological health—are significantly different from what we might find in the population.
08:34
Our department conducted research together with psychiatrists from the Institute of General and Forensic Psychiatry. With the consent of the patients, they underwent psychiatric consultation and testing of their mental status. A significant proportion of patients had mental disorders. They were not part of the circle of big psychiatry.
But this suggests that IBS is a complex symptom complex that includes both motor and secretory disorders of intestinal function. The most important thing is that there are all kinds of psychopathological deviations.
In addition to the fact that patients' complaints about stool disorders are the main ones, these patients have a number of characteristics. First of all, the variety and colorfulness of complaints. It is these patients who may complain that their stool is ugly.
It should be noted that these patients have a peculiar dynamics of well-being during the day. It is this dynamic that is probably the factor that irritates nursing staff.
These patients (usually female patients) feel unwell in the morning. They often demand that food be served in bed and so on. By the evening they literally become different people - cheerful, cheerful, efficient.
This situation is entirely consistent with what we find in endogenous or reactive depression. It is due to the fact that the production of serotonin is impaired in these patients. Perhaps this is why antidepressants, especially selective serotonin reuptake inhibitors, work so well on them.
Although IBS has gained citizenship rights now, it is a disease that has been known for a long time. It appeared under different names in both the 19th and 20th centuries. Moreover, each position that predominated in the clinical picture gave its name.
Everywhere it is reflected that spasms, dyskinesia, and disturbances in stool character predominated. It is very important that changes in mental status were observed in the clinical picture.
All this is explained by the fact that it is in IBS that the leading pathogenesis is visceral hypersensitivity. The main point that leads to the fact that these patients have visceral hypersensitivity is a decrease in pain sensitivity. This correlates with the fact that their endorphin production is impaired.
In addition, these patients have increased sensitivity to the action of gastrointestinal hormones and neurotransmitters. Especially, for example, to cholecystokinin.
11:55
Cholecystekinin, in addition to its effects on gallbladder and intestinal motility, has sensitive effects on the central nervous system (CNS). Its overproduction involuntarily leads to changes such as panic attacks, feelings of fear, anxiety, and so on.
Recently, another position has appeared. It turned out that approximately 30–35% of patients with IBS are associated with an intestinal infection. This connection and the high concentration of intestinal infection antigens in the blood made it possible to identify another form of IBS - post-infectious IBS.
In these patients, visceral hypersensitivity is thought to be due to damage to the intrinsic visceral nervous system resulting from exposure to infection. An example is the observation that E. coli was shown to produce gamma-aminobutyric acid and glutamate.
These biologically active substances are involved in the development of anxiety-phobic disorders and the development of depressive disorders. It has been noted that correction of the concentration of E. coli in the intestine normalizes mental status.
As already mentioned, this is primarily pain in the colon. The pain is the stronger in those parts of the intestine where there is more muscle mass. Mostly, patients complain of pain in the left side of the colon.
Most patients associate these pains not so much with a diet disorder, but with so-called stress. Moreover, their stress level is very low. This level of stress can, for example, be a bad grade received by a child in class.
But in any case, the symptom leading to pain is spasm, that is, contraction of smooth muscles that is not accompanied by relaxation.
14:17
Smooth muscle spasm determines almost all the symptoms of IBS. This includes pain, constipation, and flatulence. Left hypochondrium syndrome or splenic angle syndrome, when gases accumulated in this place cause severe pain due to spasm of the sigmoid colon. The fight against spasm, the severe spastic state of smooth muscles, is one of the main principles in the treatment of IBS.
If we talk about the principles of treatment of IBS, then with regard to diet the issue is resolved very simply. Patients often find a diet themselves. For diarrhea, this is a mechanically gentle diet. For constipation, they use plant fibers. It is very important that the second most important thing is the use of antispasmodics, which normalize intestinal motor function.
The second principle is literally right at hand - this is the normalization of the function of the central and autonomic nervous system with the use of psychotropic drugs and a decrease in visceral sensitivity.
Quite important is the normalization of the enzyme composition of the intestine. Impaired motility is accompanied by a disruption in the ability of enzymes to carry out their necessary enzymatic efficiency in the intestines.
It must be remembered that IBS is different in that there is a significant amount of concomitant pathology, also of functional origin. These are gallbladder dyskinesia, sphincter of Oddi dysformia, cardiospasm, pylorospasm. Naturally, all these concomitant comorbid conditions are caused by this spasm.
In the recommendations that are currently used, antispasmodics and antidepressants are used together to combat pain. It is especially emphasized that these are antidepressants, selective serotonin reuptake inhibitors.
Antispasmodics used in the treatment of IBS are mainly myotropic. They affect the biochemical processes that cause smooth muscle contraction. Antispasmodics are divided into phosphodiesterase inhibitors, calcium channel blockers, and sodium channel blockers. All of them are aimed at changing the concentration of calcium in the blood.
17:12
The Sami's first drug that was used in the treatment of spastic intestinal conditions was Papaverine, an opium derivative. Then, since 1961, there was the phosphodiesterase inhibitor “Drotaverine” or “No-shpa”. Its effectiveness is, of course, its effect on phosphodiesterase. Inhibition of this enzyme causes calcium concentration to change.
Phosphodiesterase is involved in inhibiting the entry of calcium from intracellular stores, thereby not being associated with membrane metabolism.
Phosphodiesterase is a universal enzyme that is present in almost any smooth muscle. The use of such a universal remedy as “Drotaverine” may involuntarily raise the question: whether vasodilation will occur, an effect on cardiomyocytes, and so on.
In this regard, it should be noted that “Drotaverine” has a rather specific effect on the phosphodiesterase enzyme, which is called phosphodiesterase-4. It is this isoenzyme that predominates in smooth muscles.
Other variants of phosphodiesterase: phosphodiesterase-3 is in cardiomyocytes, phosphodiesterase-5 is in blood vessels. This drug is quite specific.
One more thing. The effect of phosphodiesterase-4 is associated not only with the contraction of smooth muscle, but also its positive effect on the inflammatory process and on edema. We can say that this is a fairly universal drug.
Doctors appreciated this drug. It has been shown in a fairly large number of clinical studies that this drug is easily and well absorbed. Peak concentrations approximately 35 minutes after oral administration. Half the dose is absorbed after 12 minutes.
Emergency doctors note that intramuscular administration of Drotaverine has an effect of 70–80% and does not require the use of analgesics.
One very important phenomenon is worth highlighting. If you first administer No-shpu, and then, for one reason or another (for example, during myocardial infarction), morphine is administered to the patient, then this combination does not lead to spasm of the sphincter of Oddi. ICU doctors often use this.
In the treatment of functional pathology, which is accompanied by spasm (this is not only IBS, but also dyskinesia of the gallbladder, sphincter of Oddi, functional constipation), this drug has proven to be an effective antispasmodic. Its use does not depend on the predominance of one or another part of the parasympathetic nervous system. It is quite safe and economical.
During 1961, more than 70 clinical trials were conducted. The safety of the drug has been demonstrated in a large number of patients. Side effects were observed in no more than 1% of cases.
Thank you for attention.
First aid for a woman with pain in the lower abdomen
First of all, a woman needs complete rest; it is important to help her lie down or sit down so that she chooses a position that is more comfortable for her, in which the least discomfort will be felt. Next, apply cold - ice to the suspected source of pain; any cold that is at hand will do. Wrap the cold in a cloth so as not to increase discomfort and immediately call for medical help. Before doctors arrive, it is better to avoid changing the patient’s position so as not to provoke a worsening of the situation, and not to take painkillers - this will cause a possible worsening of the situation, and in the future will prevent the correct establishment of the cause of pain and an accurate diagnosis. It is forbidden to use the shower, and it is undesirable to eat or drink. It is strictly forbidden to use a hot heating pad for pain in the lower abdomen in women - this provokes a deterioration in well-being and will increase pain and cause complications. The visiting doctors will make their own further actions and decisions during the examination and examination. Doctors' prescriptions depend on the degree of complexity of the disease. The doctor prescribes medications: antibiotics or painkillers. Or hospitalization is required with a full diagnosis and possible surgical intervention to quickly remove the pathological change, which will quickly eliminate the source of pain and relieve the woman from pain, discomfort and unpleasant sensations. But situations arise when it is better to use complex, combined treatment. It often happens that the count of time goes against a person, when surgical intervention is the only way to help a person and save his life. Take care of yourself, be healthy, your health is in your hands!
Spasms, cramps in the abdomen in children without diarrhea: causes
- Abdominal cramps in a child manifest themselves in the form of severe pain. The main cause of this disease is the child’s disrupted diet or overeating. Sometimes the cause of spasms can be diseases of the digestive system.
- Colic , which is caused by spasm, is not a separate disease. They are considered a sign of certain pathologies or some kind of malfunction of the whole body.
- Before you begin treatment for the disease, you must visit a specialist. He will determine the real reason for this condition. The doctor will carefully examine the child, ask for tests, and undergo the necessary studies.
In a child without diarrhea,
abdominal cramps may appear due to:
- Overeating.
- Worms.
- Poisoning with mushrooms or toxic substances.
- Poor quality, bad, exotic or stale food.
- Intestinal obstruction.
- Damage to the gastrointestinal tract by bacteria.
- Ailments that originate in the pancreas and stomach.
- Nervous strain, excitement or stressful situation.
Folk remedies for abdominal cramps
As a supplement to medications, be sure to use an alternative direction - folk remedies.
- Chamomile tea. Take 1 tsp. dry chamomile. Brew in 1 tbsp. boiling water Take 3 times a day.
- A decoction using centaury, St. John's wort and cucumber. Mix the herbs. Take 1 tbsp. composition, pour a glass of boiling water. When the product is infused, take 100 ml 3 times a day.
- Mint tea. Pour boiling water over mint (1 tbsp). Take every day up to 4 times.
- Decoction with gooseberries. Pour boiling water (300 g) over the gooseberries. Boil, cook for no more than 10 minutes. Drink 250 ml 3 times a day.
- Tincture made from calendula. To relieve spasms, dissolve the tincture in 50 g of water (add 50 drops in total).
Chamomile
The following methods will help you relieve pain from abdominal cramps and get rid of them completely:
- Drink a decoction of berries every day. To prepare, use blueberries, blackcurrant leaves, plums and gooseberries.
- Drink vegetable oil every 2 hours (1 tsp is enough). After this, drink a mint or chamomile infusion.
- Take meadowsweet, St. John's wort, walnut partitions, nettle. All components must be the same. Fill with water, boil, leave until completely cool. Drink after 1 hour. One dose is equal to half a glass.
Decoction
If spasms are not a symptom of some pathology, then you need to go on a diet. Balance your diet, exclude fatty, spicy, fried foods. To get rid of cramps forever, divide your diet into 5 meals. Portions should be of such a size that after them you feel a slight feeling of hunger. We also advise you to be less nervous and avoid stressful situations.
We hope you will be interested in other useful health topics:
- Somniloquy or why people talk out loud in their sleep
- How and when to tell your first child about your mother’s pregnancy
- Gestosis in pregnant women: causes, symptoms, treatment
- Fear of getting sick is what a phobia
- Eating every other day: rebooting your metabolism and losing weight
How to relieve abdominal spasms: medications
The main medications that can be taken during abdominal cramps are the following:
- Atropine or Platifilin. Coping with acute inflammatory bowel diseases. It is also recommended to take for renal colic. To relieve an attack of spasm, you need to give an injection - 1 ml of the drug.
- Mebeverine . Relieves intestinal inflammation. The medicine is taken orally, 2 times every day. One tablet in the morning, the other in the evening.
- Spasmomen . The drug is prescribed during bloating, muscle spasms, and impaired peristalsis. It is prescribed to take one tablet 3 times a day.
- No-Shpa . Recommended dosage: 1 tablet 3 times a day.
- Phenobarbital. Must be taken during severe cramps. Dosage for 1 day – 1 tablet 2 times.
The rescue
How to treat sudden severe abdominal pain?
Treatment for acute abdominal pain depends on the underlying cause.
- Symptomatically, each patient can be prescribed pain medication.
- In addition, antibiotic therapy or other causative measures may be required. For example, treatment of a heart attack manifested as epigastric pain.
- Some diseases that manifest as acute abdominal pain require surgical treatment. For example, abdominal aortic aneurysm, gastrointestinal perforation or acute appendicitis.