general information
GERD is traditionally considered an adult pathology, but according to statistics, it affects about 15% of children, and the likelihood of developing the problem increases with age. If before the age of 5 the disease is detected, on average, in one child out of a thousand, then between the ages of 5 and 15 years it affects almost every fourth child.
Constant irritation of the esophagus often leads to inflammation. In addition, the reflux of acid provokes damage to the bronchi (in 4 out of 5 cases, GERD is accompanied by the development of bronchial asthma), premature tooth decay, and an increase in diseases of the ENT organs. Lack of treatment significantly increases the risk of developing esophageal cancer in adulthood.
Is it possible to cure gastritis in a child?
Compliance with all doctor’s recommendations and a carefully thought-out nutrition plan for the child gives a good prognosis for the treatment of gastritis. It is especially important to adhere to a therapeutic diet during an exacerbation of the disease.
Signs of exacerbation of gastritis:
- decreased appetite;
- pain and feeling of heaviness after eating;
- belching, etc.
On the first day of exacerbation of the disorder, it is recommended to refrain from eating, and then carefully introduce puree soups, kefir or low-fat broth into the diet. And it is imperative to exclude carbonated drinks, chocolate, dairy products and fruits.
For chronic gastritis, 4 meals a day are recommended, but it is not allowed to give the child fatty meats and foods containing coarse fiber.
Careful monitoring of the response to treatment, as well as regular examination by a pediatric gastroenterologist, allows you to get rid of the disease as quickly as possible and minimize the likelihood of developing complications and relapses of gastritis in children.
2
0
2
Article rating:
4 out of 5 based on 4 ratings
Author: Omelchenko Elena Vladimirovna
Pediatric gastroenterologist. Highest qualification category. Work experience 29 years.
Classification: types and degrees of GERD in children
There are three main types of GERD in children:
- without esophagitis: not accompanied by inflammation of the mucous membrane;
- with esophagitis: accompanied by inflammation of the esophagus; Within this type, 4 degrees of the disease are distinguished depending on the severity of the inflammatory process:
- I degree: slight local redness and/or friability of the mucous membrane;
- II degree: total redness, isolated surface defects (erosions) and areas of plaque;
- III degree: there is a large number of erosions;
- IV degree: bleeding ulcers, narrowing (stenosis), Barrett's esophagus (changes in the structure of the mucosa);
- A: prolapse occurs periodically, and its size does not exceed 1-2 cm;
- B: obvious disruption of the sphincter, prolapse length more than 3 cm;
- C: prolonged or persistent prolapse.
How to relieve pain with gastritis in a child?
The nature and degree of pain in different types of gastritis is different, but all pain impulses come from the muscular layer of the stomach, since there are no pain receptors in the mucous membrane. The origin and source of pain signals determines the scheme for their elimination.
Thus, pain in acute gastritis has a cramping nature (spastic pain), so it is relieved by taking antispasmodics, enterosorbents and mandatory diet.
Pain in acute gastritis caused by intoxication is recommended to be relieved by gastric lavage, as well as by taking an enterosorbent and an antiemetic drug if necessary.
Reducing pain during exacerbation of the chronic form of the disease is achieved by taking analgesics, antispasmodics, enzymes and anticholinergics. However, since these medications can negatively affect the functioning of the gastrointestinal tract, while taking them you need to follow a gentle diet and take gastroprotectors.
Thus, the main types of medications that reduce pain in gastritis are:
- analgesics that lower the tone of the muscle fibers of the stomach and reduce their spasm, blocking the transmission of pain impulses from the stomach to the brain;
- gastroprotectors or astringents, they have a bactericidal effect and form a protective film on the gastric mucosa. These drugs not only prevent irritation, but also relieve inflammation of the mucous layer;
- enzymes that help break down food and improve digestion;
- antacids that neutralize the aggressive effects of hydrochloric acid during its excessive synthesis;
- anticholinergics, which have an antispasmodic effect, reduce the secretion of gastric juice and do not affect the formation of a protective layer of mucus.
The composition of the course of therapy is prescribed exclusively by a gastroenterologist, since the type of medications and their dose depend on the type of disease, its prevalence and the degree of inflammation of the mucous membrane.
Symptoms of GERD in children
All symptoms of GERD in children are divided into those related to the digestive system (esophageal) and not related to it (estraesophageal). Esophageal symptoms are directly related to irritation of the esophageal mucosa and the periodic release of stomach contents into the upper digestive tract. In infancy, the disease usually manifests itself with frequent spitting up and vomiting, sometimes with streaks of blood. If the situation repeats often, the baby may not gain weight quickly enough. If stomach contents enter the respiratory tract, pneumonia, respiratory arrest and death may occur.
As the child grows, the symptoms of GERD begin to resemble the typical course of the disease in adults. A small patient may complain of heartburn, sour or bitter belching, excessive salivation, and even a wet spot appearing on the pillow after sleep. Sometimes after eating there is pain in the chest and/or a feeling of a lump in the throat.
Extraesophageal (extraesophageal) signs of GERD depend on the location of the pathological changes. They can be:
- bronchopulmonary: paroxysmal cough, shortness of breath after eating or at night, as well as other symptoms of bronchial obstruction up to the development of bronchial asthma;
- otolaryngological: hoarseness, ear pain, feeling of a lump in the throat, etc.;
- cardiological: heart rhythm disturbances (arrhythmia, extrasystole);
- dental: premature destruction of tooth enamel.
To understand why we don’t like GERD, let’s discuss the definition of the disease.
Reflux disease differs from ordinary physiological reflux in two fundamental ways - it causes symptoms that interfere with normal life and it causes complications.
Complications can be directly related to damage to the esophageal mucosa and extra-esophageal ones.
I have already talked about extra-esophageal manifestations from time to time - they can affect the respiratory system and oral cavity.
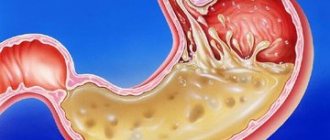
What happens to the mucous membranes of the esophagus?
The most common option is the non-erosive form of GERD . During gastroscopy, the endoscopist sees swelling and redness, although it must be admitted that these signs are quite subjective.
A more severe manifestation is the appearance of erosions of the esophageal mucosa .
If non-erosive GERD can be compared to abrasion on the skin, then erosive esophagitis is real abrasions, that is, a deeper and longer-healing damage.
Detection of erosions indicates more severe reflux and often erosions are found again and again after stopping treatment.
Sometimes repeated erosions cause anemia - chronic anemia due to small but frequent bleeding from erosions.
In rare cases, the damage is so severe that ulcers .
There is a small chance that repeated damage will cause scarring and narrowing (stricture) of the esophagus.
With a stricture, difficulties arise when swallowing, first denser and then liquid food.
Causes of GERD in children
The development of GERD is based on insufficiency of the sphincter that separates the esophagus and stomach. Due to its incomplete closure, a backflow of digestive juices and/or semi-digested food occurs. A similar condition can occur against the background of excess body weight, hiatal hernia, or connective tissue dysplasia. Partially influence reflux:
- periodic increase in intra-abdominal pressure (due to frequent bending forward, coughing, constipation);
- excess nutrition;
- excessive production of gastric juice;
- taking certain medications.
Diagnosis of GERD in children
The diagnosis of GERD is made to a child by a gastroenterologist after analyzing complaints and anamnesis (history of the development of the disease, the patient’s life history, including features of pregnancy and childbirth, etc.), as well as undergoing an examination. To confirm gastroesophageal reflux disease and clarify its type and degree, the following studies are prescribed:
- esophagoscopy: endoscopic examination that allows you to visually assess the condition of the mucosa; carried out using a flexible probe with a camera, usually combined with gastro- and duodenoscopy (EGDS);
- intraesophageal pH-metry: assessment of acidity on the surface of the mucosa;
- esophageal biopsy: taking a small section of the mucosa for examination under a microscope; the sample is taken during the EGD process;
- radiography with contrast;
- general blood test (detects signs characteristic of anemia and/or bronchial asthma).
Manometry, scintigraphy, esophageal impedance testing, as well as studies and tests to identify extraesophageal lesions can be used as additional diagnostic methods. If necessary, specialists from related specialties are involved in the diagnosis.
Risk factors for severe GERD:
- serious neurological impairment
- obesity
- condition after esophageal atresia
- diaphragmatic hernia
- achalasia of the esophagus
- prematurity
- cystic fibrosis
- bronchopulmonary dysplasia
- idiopathic pulmonary fibrosis
- condition after lung transplant
Children with risk factors require more careful monitoring by a gastroenterologist and they are more likely to require surgical treatment of GERD.
There will be a separate discussion about treatment.
The photo of Rusty [email protected]
1, total, today
Treatment of GERD in children
Depending on the age of the child, the severity of GERD and the characteristics of its course, various methods are used to treat the disease.
Non-drug correction is based on normalizing nutrition, feeding in an elevated position, and sleeping with the head of the head elevated. In young children, special antireflux mixtures are used. For schoolchildren and adolescents, it is important to reduce the daily amount of food, increase the amount of protein in the diet, as well as reduce body weight in case of obesity.
If these measures are ineffective, drugs that reduce the acidity of gastric juice are prescribed, and in severe cases, surgical treatment in a specialized institution is required.
Doctor's opinion
Gastroesophageal reflux disease can cause a lot of trouble for the child and his parents. Frequent regurgitation in infancy can cause milk or stomach acid to enter the respiratory tract. At older ages, there is a significant risk of developing bronchial asthma and other associated pathologies. A timely visit to an experienced gastroenterologist and following all his recommendations will help you avoid problems and keep the disease under control.
It is important to pay attention to all aspects of treatment, including dietary adjustments and correct sleeping position. In this case, the child will quickly forget about the unpleasant symptoms and will be able to live a full life. The habit of controlling your diet and not overeating will be very useful in adulthood. If the doctor recommends surgery, you should not be afraid of intervention. Modern laparoscopic technologies can significantly reduce the recovery period. The operation allows you to completely get rid of GERD and forget about the need to take medications.
Question answer
Is it possible to treat heartburn with folk remedies?
Traditional methods are not suitable for treating GERD, especially when it comes to a child. You shouldn’t waste time looking for the right product; at best, you’ll just waste time. At worst, you will encounter an unpredictable reaction from the body.
What sports are contraindicated for GERD?
The ban is imposed only on activities related to lifting weights, bending the body forward, or significant tension in the abdominal muscles. Other sports are not contraindicated and will even be beneficial.