Odeston is a synthetic drug that stimulates bile formation, facilitating its entry into the lumen of the duodenum. Bile is produced in liver cells. Stimulation of its entry into the intestines, under the influence of the drug, helps to accelerate the digestion process and activate peristalsis, as well as normalize stool.
General principles and place of Odeston in the treatment of biliary dysfunction
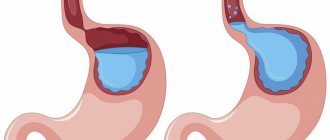
Despite the fact that they try to isolate the biliary system (the system of bile ducts and sphincters that regulate the flow of bile) from the organ (liver), it is part of it and functions in one way or another depending on the condition of the liver. The role of small (intralobular, interlobular) ducts in the formation of dysfunctional disorders is not entirely clear. Clinical equivalents of movement disorders take on reality, starting from the lobar ducts, the common hepatic and common bile duct (CBD), the beginning of which is considered to be the junction of the hepatic duct with the cystic duct. The distal part of the CBD passes through the thickness of the head of the pancreas, and the duct opens on the posterior wall of the descending duodenum 2–10 cm below the pylorus. According to radiological data, the CBD width is from 2 to 9 mm; according to ultrasound data, in the presence of a gallbladder (GB) - from 2 to 6 mm, without a gallbladder - from 4 to 10 mm. At the junction of the gallbladder into the cystic duct, the muscle fibers take a circular direction and form the sphincter of the gallbladder duct (Lutkens). From the hepatic ducts and CBD, bile enters the gallbladder at the moment of closure of the sphincter of Oddi, which consists of: – the actual sphincter BDS (Westphal sphincter), which ensures the separation of the ducts from the duodenum; – the sphincter of the common bile duct (CBD); – sphincter of the pancreatic duct. The motor reaction of the gallbladder and sphincter of Oddi largely depends on the quantity and quality of food, as well as on the emotional state. The direction of bile movement is determined by the interaction of hepatic secretion, the rhythmic activity of the sphincters of the terminal part of the CBD, the sphincter of the gallbladder, the cystic duct valve, as well as the absorptive function of the mucous membrane of the gallbladder and all ducts, which creates a pressure gradient. The work of all departments of the biliary system is strictly coordinated. This coordination is ensured by a nervous and humoral response. The basic principle of the entire regulatory system is multi-level self-regulation (including locally produced hormones and biologically active substances). Motor innervation is carried out by the sympathetic and parasympathetic nervous system. Nerve plexuses are present in all layers of the biliary system. Sensitive fibers of the bile ducts can only perceive stretching. As for opioid peptides, the regulatory mechanisms of their influence have not yet been clarified. Classification, definition of clinical variants of dysfunction, diagnostic approaches Functional diseases of the biliary tract are a set of clinical symptoms that develop as a result of motor-tonic dysfunction of the gallbladder, bile ducts and sphincters. According to the latest International Classification, instead of the term “functional diseases of the biliary tract” (Rome Consensus, 1999), the term “dysfunctional disorders of the biliary tract” has been adopted. At the same time, regardless of the etiology, they are usually divided into two types: • gallbladder dysfunction (GB); • dysfunction of the sphincter of Oddi. In the latest International Classification of Diseases (ICD-10), only “dyskinesia of the gallbladder and bile duct” is identified - under the heading K82.8 and “spasm of the sphincter of Oddi” - under the heading K83.4. It is known that moderate irritation of the vagus nerve causes coordinated activity of the gallbladder and sphincters, and severe irritation causes spastic contraction with delayed bile evacuation. Irritation of the sympathetic nerve promotes relaxation of the gallbladder. Of the gastrointestinal hormones, the maximum effect is exerted by cholecystokinin-pancreazimin (CCK-PZ), which, along with the contraction of the gastrointestinal tract, promotes relaxation of the sphincter of Oddi. The stimulator of CCK-PZ production is fatty foods, and the activator of nervous regulatory effects is the pressure gradient and its changes. The main cause of disorders of the rhythmic activity of the biliary system is considered to be inflammatory processes in the liver, leading to disruption of bile synthesis, a noticeable decrease in pressure in the ductal system and gallbladder, and in connection with this – to a constant spastic contraction of the spicter of Oddi. Various surgical interventions (cholecystectomy, vagotomy, gastrectomy) also lead to significant dysfunction of the biliary system. The formation of bile is a continuous process, but the entry of bile into the intestines occurs only during the digestion process. This is ensured by the reserve function and its rhythmic contractions with sequential relaxation of the sphincters of Lutkens and Oddi. Relaxation of the gallbladder is accompanied by closure of the sphincter of Oddi. There are primary and secondary dysfunctional disorders. Primary – are rare and average 10–15%. In this case, a decrease in the contractile function of the gallbladder may be associated both with a decrease in muscle mass (rarely) and with a decrease in the sensitivity of the receptor apparatus to neurohumoral stimulation (most). Moreover, a small number of receptors can be genetically determined and acquired due to inflammatory, dystrophic and metabolic disorders. Secondary dysfunctional disorders of the biliary tract can be observed with hormonal disorders, treatment with somatostatin, premenstrual syndrome, pregnancy, systemic diseases, diabetes mellitus, hepatitis and cirrhosis of the liver, jejunotomy, as well as in the presence of inflammation and stones in the gallbladder. It should be noted that the presence of these diseases does not imply a stable failure of regulatory systems and the perceptive apparatus, but a varying degree of these disorders in different periods and phases of the course of the diseases. In this regard, there is an “undulation” of disorders, up to periods of rather long stability, but with an “easy” withdrawal of this system from stability to motor disorders. Psycho-emotional overload, stressful situations, and general neuroses are important. The vast majority of patients who have undergone cholecystectomy are characterized by insufficiency of the sphincter of Oddi with continuous flow of bile; spasm is less common. The second most common cause of biliary disorders is distal gastrectomy, leading to weakened hormonal regulation and hypotension of the gastrointestinal tract. The classification of dysfunctional disorders of the biliary tract is presented in Table 1. For ease of perception and for practical purposes, the classification presents unidirectional disorders, although in practice they are often complex in nature with a predominance of one of the components. The clinical manifestations of these disorders are quite well known. With hyperkinetic disorders, colicky pain of varying intensity occurs without irradiation or with irradiation to the right, to the back, sometimes to the left half of the abdomen (with the involvement of the pancreatic ductal system). With hypokinesia, there is dull pain in the right hypochondrium, a feeling of pressure, fullness, which intensifies with changes in body position and with an increase in intra-abdominal pressure, changing the pressure gradient for bile flow. Common to different forms of dysfunction are: bitterness in the mouth, bloating, unstable stool. Thus, the central symptom of gallbladder dysfunction is the biliary type of pain, and the only objective characteristic is delayed gastric emptying. Available diagnostic methods do not explain the cause of this dysfunction (there may be several); Factors such as impaired filling or decreased sensitivity of the sensing apparatus of the gallbladder cannot be excluded. Diagnostic criteria for gallbladder dysfunction are episodes of severe constant pain localized in the epigastrium or in the right upper quadrant of the abdomen, characterized by: – episodes lasting 30 minutes or more; – development at least once in the previous 12 months; – permanent in nature, which reduces the daily activity of patients and requires consultation with a doctor; – lack of evidence of organic pathology; – the presence of a violation of the function of emptying the gallbladder. A very important objective symptom of impaired GB motility is the ultrasonic phenomenon of “sludge” (sediment), which, according to our data, can be presented in two variants: a) diffuse, b) parietal. The latter option, depending on the clinical situation, can be characterized as “inflammatory” or without inflammation, but then the sediment elements that form it turn out to be quite large. In addition, the entire clinical symptom complex should be analyzed: nausea and vomiting, irradiation, provoking factors (food intake and its nature). As for sphincter of Oddi dysfunction, there are 4 types (3 types of biliary dysfunction and 1 type of pancreatic dysfunction). Diagnostic criteria are - an attack of biliary pain and 3 laboratory and instrumental signs: - an increase in AST and/or alkaline phosphatase by two or more times with a 2-fold determination; – slowdown in the removal of contrast agents during endoscopic retrograde cholangiopancreatography – ERCP (more than 45 minutes); – expansion of the common bile duct (CBD) more than 12 mm. Type I dysfunction is characterized by pain, accompanied by all three laboratory and instrumental signs; Type II – pain and 1–2 signs; Type III – only an attack of pain. Type IV – pancreatic, characterized by “pancreatic” pain and increased levels of amylase or lipase. However, with mild pain, hyperfermentation may be absent. In cases where ERCP allows us to exclude the absence of stricture pathology, monometry of the biliary and pancreatic sphincters is indicated. The World Congress of Gastroenterology (Bangkok 2002) determined that evidence-based medicine does not require consensus, but evidence. It was also stated there that dysfunction of the sphincter of Oddi should not be classified as a clearly defined disease, but as a condition with a variable “dysfunction-symptom” relationship. In addition, it was emphasized that impaired gastric emptying is well known as a consequence of inflammatory damage, mechanical obstruction or autonomic denervation. In the absence of these conditions, it is not entirely clear whether delayed gastric emptying can be considered as a separate clinical problem (nosological form). These are important provisions that guide further search for understanding the clinical situation under consideration. Principles of treatment of dysfunctional biliary disorders The main goal of treatment of patients with dysfunctional biliary tract disorders is to restore the normal flow of bile and pancreatic secretions through the biliary and pancreatic ducts. In this regard, the objectives of the treatment of these disorders are: • Restoration, and if impossible, replenishment of bile production during the development of chronic biliary insufficiency, which is understood as a decrease in the amount of bile and bile acids entering the intestine 1 hour after the introduction of the irritant. After cholecystectomy, almost without fail, dysfunction of the sphincter of Oddi develops, since the gallbladder is excluded from the normal functioning of the biliary system. In this regard, there is also an irreplaceable loss of bile acids with the development of chronic biliary insufficiency, which supports both digestive disorders and dysfunctional disorders. • Increased contractile function of the gallbladder (if it is insufficient). • Decreased contractile function of the gallbladder (with its hyperfunction). • Restoration of the tone of the sphincter system. • Restoration of pressure in the duodenum (which determines the adequate pressure gradient in the biliary tract). Until now, diet therapy plays a significant role in the system of treatment measures. Its general principle is a diet with frequent meals of small amounts of food (5-6 meals a day), which helps normalize pressure in the duodenum and regulates the emptying of the gallbladder and ductal system. Excluded from the diet: alcoholic drinks, carbonated water, smoked, fatty and fried foods, seasonings, as they can cause spasm of the sphincter of Oddi. The dietary diet takes into account the influence of individual nutrients on the normalization of the motor function of the gallbladder and biliary tract. Thus, with the hyperkinetic type of dysfunction, the consumption of foods that stimulate the reduction of the gallbladder should be sharply limited - animal fats, vegetable oils, rich meat, fish and mushroom broths. With hypotension of the gallbladder, patients, as a rule, tolerate weak meat and fish broths, cream, sour cream, vegetable oils, and soft-boiled eggs well. Vegetable oil is prescribed in a teaspoon 2-3 times a day 30 minutes before meals for 2-3 weeks. To prevent constipation, dishes that promote bowel movement are recommended (carrots, pumpkin, zucchini, greens, watermelons, melons, prunes, dried apricots, oranges, pears, honey). This is especially important due to the fact that a normally functioning intestine ensures normal intra-abdominal pressure and normal passage of bile into the duodenum. The use of food bran (with sufficient water) is necessary not only (and not so much) for adequate intestinal function, but also to maintain motility of the biliary tract, especially the gastrointestinal tract if there is sediment in it. Among the drugs that affect the motor function of the gastrointestinal tract, the following are used for dysfunctional biliary disorders: • anticholinergic drugs; • nitrates; • myotropic antispasmodics; • intestinal hormones (CCC, glucagon); • choleretics; • cholekinetics. Anticholinergics, by reducing the concentration of intracellular calcium ions, lead to muscle relaxation. The intensity of relaxation depends on the initial tone of the parasympathetic nervous system, but when using drugs in this group, a wide range of side effects develops, including dry mouth, difficulty urinating, and blurred vision, which greatly limits their use. Nitrates (nitroglycerin, nitrosorbide) cause relaxation of smooth muscles due to the formation of free radicals of nitric oxide (NO), which contribute to an increase in cGMP content. Their use, however, is accompanied by the development of pronounced cardiovascular effects and other adverse reactions. In addition, the development of tolerance makes nitrates unsuitable for long-term therapy. Calcium channel blockers are divided into non-selective and selective. – Non-selective calcium channel blockers (nifedipine, verapamil, diltiazem, etc.) can relax smooth muscles, incl. and biliary tract, but this requires the use of the highest possible doses, which practically excludes their use due to pronounced cardiovascular effects. – Selective calcium channel blockers (panaveria bromide, otilonium bromide) act primarily at the level of the colon, where they are metabolized. About 5–10% of the dose of these drugs can work at the level of the biliary tract. This aspect of their action, however, requires further study. There is evidence that these drugs help restore the pressure gradient in the biliary system. Among the myotropic antispasmodics, attention is drawn to hymecromone (7-hydroxy-4-methylcoumarin) - Odeston (Pabyanitsky Pharmaceutical Plant Polfa JSC). It has a selective antispasmodic effect on the sphincter of Oddi and the sphincter of the gallbladder, and also has a choleretic effect. Combining antispasmodic and choleretic properties, Odeston ensures harmonious emptying of intra- and extrahepatic bile ducts, timely and unhindered flow of bile into the duodenum. Odeston does not have a direct choleretic effect, but, by facilitating the flow of bile into the digestive tract, it enhances the enterohepatic recirculation of bile acids, which are involved in the first phase of bile formation. The advantage of Odeston over other antispasmodics is that it has virtually no effect on other smooth muscles, in particular those of the cardiovascular system and intestines. Odeston simultaneously relaxes the sphincters of Oddi and Lütkens, therefore, unlike many choleretic drugs, it does not increase pressure in the bile ducts and, as a result, which is very important, does not provoke “biliary colic.” By increasing the flow of bile into the intestinal lumen, Odeston helps improve digestion (eliminate mild and moderate chronic biliary insufficiency) and activates intestinal motility, which leads to normalization of stool. The drug has undergone fairly extensive clinical testing in Russia. So, in 2000 S.V. Nasonova and L.I. Tsvetkova published the results of a study assessing the effectiveness of treatment with Odeston in 50 patients, of whom 20 suffered from inflammatory diseases of the biliary tract, 15 from cholelithiasis, 15 from biliary tract dysfunction with hypertonicity of the sphincter of Oddi. A two-week course of treatment was carried out with good effect in the majority of patients in the first two groups and in all patients in the third group. This was expressed in the normalization of the contractility of the gallbladder, the normalization of the tone of the sphincter of Oddi, and the reduction of ultrasound signs of inflammation. The drug was well tolerated, there were no toxic effects and, very importantly, there were no provocations of biliary colic in patients with cholelithiasis (GSD). In another work, S.V. Nasonova and O.I. Lebedeva (2001) evaluated the drug Odeston in patients with various disorders of the biliary tract and confirmed the effectiveness of the drug. The data of Polish researchers were confirmed, which showed that the maximum concentration of the Odeston is reached after 2.5-3 hours, the therapeutic level of the drug in the blood is preserved for 6-8 hours, and its effective dose is 400 mg (2 tablets) 3 times a day. E.P. Yakovenko and co -authors (2000) studied Odeston in patients with dysfunction of the Oddi sphincter associated with cholecystectomy. Patients received the drug at a dose of 200-400 mg 3 times a day for 1-3 weeks, which provided a good regulatory effect on the tone of the Oddi sphincter. Therapy had a combined character (enzyme preparations were added with pancreatic insufficiency, with dysbiosis - probiotics, etc.). We also evaluated the effectiveness of Odeston in 30 patients, 15 of which suffered from non -channel cholecystitis with biliary dysfunction, and 15 chronic calculent cholecystitis with dysfunctional disorders. The clinical parameters (pain and dyspeptic symptom complex) were evaluated, the effect of the drug on the phenomenon of the “lithogenicity” of bile was studied, as well as on the contractile ability of the ANP and the tone of the Oddi sphincter according to ultrasound. Patients received Odeston 200-400 mg 3 times a day 30 minutes before meals for 2-4 weeks. It was established that pain and dyspeptic symptom complexes stopped, on average by the 7th day; The elimination of the dysfunction of the GP (both hypo- and hypertonicity) took place without a significant impact on its normal contractile ability; The sphincter of Oddi was effectively suppressed and the disappearance of the phenomenon of the “non -brownness” of bile was observed. The study also confirmed good tolerance of the drug and the lack of side effects. ON THE. Korovina et al. (2001) published data from an Odestonia treatment of 25 children with dysfunction of the biliary tract (the dose of the drug amounted to 300 mg/day of children under 10 years of age and 600 mg/day of children 11-14 years old). The duration of treatment was 1-3 weeks. Almost all children noted the high efficiency of the drug, which was expressed in the relief of constipation, eliminating biliary failure, reducing sediment in the LSP and eliminating pain. The drug Odeston was well tolerated, toxic phenomena and side effects were absent. The overall conclusion of the studied studies is that Odeston is effective in patients with dysfunction of the biliary tract (adults and children), has a choleretic effect, eliminates biliary insufficiency, dysfunction of the sphincter of Oddi and its hypertonicity, including after cholecystectomy. Of other myotropic antispasmodics, it should be noted of the furnitureurin, which selectively affects the tone of the sphincter of Oddi (directly and indirectly) and, therefore, is deprived of the side effects due to the universal antispasmodic effect. In the treatment of hypofunction of the GOP, drugs are used that enhance its motor skills. For this purpose, horners can be used, which include drugs containing bile or biliary acids (allochol, dehydrochular acid, cholenzim); synthetic preparations (Osalmid, hydroxymethylnicotinamide, cyclovalon); some herbal preparations (flaming, corn stigmas, etc.); As well as cholelfate, such as magnesium sulfate, olive oil and other oils, sorbiti, xylitol, etc. The choice of the drug is very important, if not the main issue. It, in particular, depends on the required speed of the effect. If the effect should be fast, then it is better to use cholecinetics (the dose of the drug has a value), and if a long course treatment is necessary, then preference should be given to yellow -containing drugs. In cases where it is required to provide an anti -inflammatory effect, the choice should be made in favor of synthetic drugs, but they should not be long -term treatment. In the presence of concomitant liver pathology, the prescribing of artichoke -based preparations that have holleret and hepatoprotective effects is preferable. In therapy, HP hypofunction can also be used with prokinetic effects, for example, Domperidon and Trimbutin. This group may also include selective calcium channel blockers (Pinaveria Bromide, Otilonia bromide) and myotropic antispasmodics (furniturer). It should be remembered that the effect of these drugs, as a rule, has an indirect nature (either the tone of the Oddi sphincter or the pressure in the duodenum is reduced) and dose -dependent, which requires the selection of an effective dose. Finally, sometimes in the treatment of HP hypofunction, drugs that reduce inflammation and visceral hyperalgesia (non -steroidal anti -inflammatory drugs, tricyclic antidepressants in low doses) can be used. Apparently, retains its role in the treatment of discinesia (hypokinesia) of the GP and cholecystectomy. However, the issue of surgical intervention should be resolved very carefully, since indications for cholecystectomy are relative in nature, and the final result is always unpredictable. Let us dwell on some other aspects of treatment of dysfunctional biliary disorders. With the dysfunction of the sphincter of Oddi, in the case of its type I, the conduct of papillosfinchesterotomy is indicated, and with type II and III, it is possible to use drug therapy. It should be borne in mind that hormones (CCC, glucagon) can only temporarily reduce the tone of the Oddi sphincter, nitrates also provide a very short effect. A strong inhibitor of the release of acetylcholine is botulinum toxin. When using this drug in the form of injections, its pressure decreases, the bile current and the clinical condition of the patient are reduced, but the response to the treatment is transient. In the pancreatic type of sphincter dysfunction (type IV) standard therapy, surgical sphincteroplasty and pancreatic lithoplasty is (drug effects are carried out only at the stage of lack of complications). Thus, recently, the attention of the medical public has been attracted to functional disorders of the gastrointestinal tract as a whole and to the biliary system, in particular. To a large extent, this is due to the fact that the treatment of functional disorders leaves hope for their cure and prevents or moves away the more severe in prognostic terms of organic pathology (including oncological). Currently, diagnostic approaches to violations by the biliary system are optimized, the arsenal of drugs used for their therapy is expanding. This provides the possibility of choosing the most effective and safe drug or combination of drugs, depending on the pathogenetic characteristics of a particular disorder. An important place in the treatment system for biliary dysfunction is occupied by the drug Odeston, with its combined effect of action, restoring most of the upset pathogenetic mechanisms (normalization of sphincter tone, normalization of the pressure gradient).
Literature 1. Sokolov L.K., Minushkin O.N. and others. “Clinical and instrumental diagnosis of diseases of the organs of the hepatopancreatoduodenal zone”, Moscow, 1987. 2. Minushkin O.N. “Dysfunctional disorders of the biliary tract (pathophysiology, diagnosis and treatment approaches)”, Moscow, 2002. 3. Korovina N.A. and others. “Biliary dyskinesia in children: modern approaches to therapy,” g. "Agna Vitae", 2001, no. 1, 32–34. 4. Kalinin A.V. "Functional disorders of the biliary tract and their treatment." Clinical perspectives of gastroenterology, hepatology, 2002, No. 3, 25–34. 5. Yakovenko E.P. and others. “Dysfunction of the sphincter of Oddi associated with cholecystectomy (diagnosis, treatment).” and. "Practitioner", 200, no. 17, 26–30. 6. Nasonova S.V., Tsvetkova L.I. “Experience of using Odeston in the treatment of chronic diseases of the gallbladder and biliary tract”, w. "Ros.zh.gastroenterology, hepatology, coloproctology." 2000, no. 3, 87–90. 7. Nasonova S.V., Lebedeva O.I. “Odeston in the treatment of chronic diseases of the hepatobiliary system,” Military Medical Journal, 2001, No. 3, 49–53. 8. Yakovenko E.P. and others. “Odeston in the treatment of diseases of the biliary tract”, g. "Practitioner", 2001, No. 19, 30–32.
What is it used for?
The main diseases for the treatment of which Odeston is used:
- Dyskinesia of the bile ducts
- Chronic noncalculous cholecystitis
- Cholelithiasis
- Cholangitis
In addition, the drug will be useful for patients who have undergone surgery on the gallbladder and its ducts. In the presence of bile hyposecretion, manifested by nausea, vomiting, loss of appetite and prolonged constipation, the prescription of this medication is also necessary.
When not to
Contraindications to the use of the medicinal substance:
- Presence of hypersensitivity to components in the composition
- Obstruction of the ducts of the biliary system
- Liver or kidney failure
- Ulcerative colitis
- Crohn's disease
- Hemophilia
Also, the drug is contraindicated for persons under 18 years of age. The use of the drug in pregnant and lactating women is possible only for health reasons.