Accessory spleen (AS) is a human developmental anomaly that occurs during embryogenesis. Most often, the DS is located in the ligaments of the spleen, less often in the tail of the pancreas (PG) [1–3]. DS in the tail of the pancreas may mimic a neuroendocrine tumor or metastasis of renal cell carcinoma. DS is usually discovered during surgery or a routine medical examination. Preoperative differential diagnosis of DS located in the pancreas tissue with tumors of this organ is difficult. We provide a description of 3 patients with intrapancreatic DS that simulated a neuroendocrine tumor in the 1st observation, metastasis of renal cell carcinoma in the 2nd.
Patient X.
, 43 years old, was hospitalized at the Federal State Budgetary Institution “Institute of Surgery named after. A.V. Vishnevsky" 10/25/17 with a diagnosis of right kidney cancer (T1bN0M0); laparoscopic right nephrectomy in 2010; progression of the disease - metastasis of renal cell carcinoma in the tail of P.Zh. Over the past years, the patient was undergoing follow-up at the oncology clinic; she underwent computed tomography (CT) with contrast every year. A routine follow-up CT scan in July 2022 revealed a hypervascular tumor of the tail of the pancreas with a diameter of 18 mm. Scintigraphy on July 21, 2017 revealed no pathological changes. The X-ray picture differentiated between a neuroendocrine tumor of the pancreas and a metastasis of renal cell carcinoma.
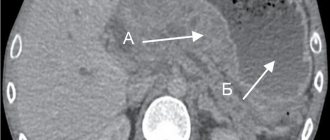
Upon entering the institute, my condition was satisfactory. She made no complaints. Physical and instrumental laboratory examination did not reveal any abnormalities. At the control CT scan on October 10, 2017, in the tail of the pancreas there was a tumor of the same size, accumulating the contrast agent (Fig. 1, a).
Rice. 1. a - CT, axial projection, arterial phase: in the tail of the pancreas there is a rounded hypercontrast tumor-like formation; b - removed specimen after distal resection of the pancreas: in the tail of the pancreas there is splenic tissue surrounded by pancreatic parenchyma. Here and in Fig. 2: CT - computed tomography; Pancreas - pancreas. Considering the history of kidney cancer, the situation was regarded as metastatic lesion of the pancreas. The patient was operated on 10.27.17 - robot-assisted distal resection of the pancreas was performed with preservation of the spleen. During the operation in the tail of the pancreas, instrumental palpation and ultrasound examination (US) revealed a tumor deep in the parenchyma that was not accessible to inspection (see Fig. 1, b). Histological examination of the resected pancreatic tissue revealed DS. In the postoperative period, the patient had a clinically insignificant pancreatic fistula (according to the ISGPS classification, 2016). She was discharged on the 8th day after surgery. The pancreatic fistula closed on its own 20 days after the intervention.
Patient N.
, 61 years old, was hospitalized in the department on November 13, 2017 with a diagnosis of non-functioning neuroendocrine tumor of the tail of the pancreas.
During a routine follow-up examination in July 2022, according to MRI, a hypercontrast tumor with a diameter of 20 mm was discovered in the tail of the pancreas. Insulin and c-peptide levels are normal. The patient underwent CT with intravenous contrast, which confirmed the presence of a hypervascular tumor in the tail of the pancreas (Fig. 2, a,
Rice. 2. a - CT, axial projection, arterial phase: hypercontrast tumor of the tail of the pancreas; b - MRI, axial projection; c — removed specimen: intrapancreatic DS is surrounded by pancreatic parenchyma. MRI - magnetic resonance imaging; DS - accessory spleen. b).
Upon entering the institute, my condition was satisfactory. I made no complaints. No concomitant diseases were identified. Based on the results of radiological diagnostic methods (CT, MRI), a diagnosis of non-functioning neuroendocrine tumor of the tail of the pancreas - cT2N0M0 - was made. The patient was operated on 11/14/17 - robot-assisted distal resection of the pancreas was performed with preservation of the spleen. Histological examination revealed DS in the thickness of the parenchyma of the gland (see Fig. 2, c). 6 days after the operation, a control CT scan revealed a fluid accumulation in the area of the pancreas stump. Drainage was performed under ultrasound control, and 50 ml of pancreatogenic content was obtained. Antisecretory therapy was carried out. The drainage released about 40 ml of pancreatogenic discharge per day. He was discharged with drainage for further outpatient treatment on the 9th day after surgery. The pancreatic fistula closed on its own 29 days after surgery.
Patient M.
, 38 years old, was hospitalized on August 27, 2012 with a preliminary diagnosis of a tumor of the tail of the pancreas, which was detected on an outpatient basis by ultrasound. The patient underwent a contrast-enhanced CT scan, which revealed the formation of a heterogeneous structure with clear uneven contours measuring up to 10×18 mm and a density of up to 71 units in the distal parts of the tail of the pancreas along the posterior surface. N and 108 units. N, which is similar to spleen tissue. In order to clarify the diagnosis, an MRI was performed, which confirmed the diagnosis of the presence of DS. The patient was recommended to undergo dynamic monitoring and undergo an MRI of the abdominal cavity after 6 months. During the control examination, according to MRI data dated January 16, 2018, the existing tumor-like formation of the tail of the pancreas was without any dynamics.
Treatment of the disease
Treatment, regardless of the size and localization (location) of the aberrant pancreas, is always surgical , since there is a risk of malignancy (degeneration of the accessory pancreas into a cancerous tumor). The volume and methods of surgery are decided individually depending on the location and size of the additional gland.
When the organ is located superficially, endoscopic electroexcision is performed. If there are cysts in the organ, then cyst fenestration surgery is indicated. Conservative treatment is also possible if there is no risk of the process becoming malignant. Long-acting drugs are prescribed - somatostatin analogues. In parallel, symptomatic therapy is carried out.
This anomaly is not dangerous until pathological processes develop, therefore, if an aberrant pancreas is detected, treatment may not be carried out, but the patient should be under the supervision of a specialist.
Life after resection or removal of the pancreas
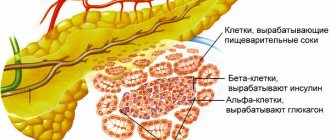
The pancreas, as already mentioned, is a very important and unique organ for our body. It produces a number of digestive enzymes, and only the pancreas produces hormones that regulate carbohydrate metabolism - insulin and glucagon.
However, it should be noted that both functions of this organ can be successfully compensated by replacement therapy. A person cannot survive, for example, without a liver, but without a pancreas, with the right lifestyle and adequate treatment, he can live for many years.
What are the rules of life after surgery on the pancreas (especially for resection of part or the entire organ)?
- Strict adherence to diet for the rest of your life. You need to eat small portions 5-6 times a day. Food should be easily digestible with a minimum fat content.
- Absolute exclusion of alcohol.
- Taking enteric-coated enzyme preparations prescribed by a doctor.
- Self-monitoring of blood sugar levels. The development of diabetes mellitus during resection of part of the pancreas is not a necessary complication. According to various sources, it develops in 50% of cases.
- When a diagnosis of diabetes mellitus is made, insulin therapy is prescribed according to the regimen prescribed by the endocrinologist.
Typically, in the first months after surgery, the body adapts:
- The patient usually loses weight.
- There is discomfort, heaviness and pain in the abdomen after eating.
- Frequent loose stools are observed (usually after each meal).
- There is weakness, malaise, and symptoms of vitamin deficiency due to malabsorption and dietary restrictions.
- When insulin therapy is prescribed for the first time, frequent hypoglycemic conditions are possible (therefore, it is recommended to keep sugar levels above normal values).
But gradually the body adapts to new conditions, the patient also learns self-regulation, and life eventually returns to normal.
Diagnosis of the disease
Detection of an abnormal pancreas largely depends on its location. If it is located in the wall of the duodenum, stomach or large intestine, then in this case diagnosis, as a rule, does not cause difficulties. Most often, its detection occurs accidentally during a screening examination, and the age of patients with such an anomaly is usually from 40 to 70 years.
This anomaly can be detected using various methods:
- Endoscopic. Such a gland looks like a large island of glandular tissue, often having the appearance of a polyp and located on a wide base. Often there may be a depression at the top of such a polyp, which is an endoscopic sign of an aberrant gland. If a superficial biopsy is taken during an endoscopic examination, it may not be informative enough.
- X-ray. The abnormal gland in this case can be visualized as a fairly large formation, which is noticeable in the form of an accumulation of contrast agent. In this case, the presence of the mouth of the duct of an additional gland may be noted (it is also contrasted).
- Ultrasonography. It is possible to notice an additional pancreas during ultrasound diagnostics; characteristic signs will help with this - the hypoechoic structure of the formation, the presence of additional cavities (not always detected), as well as the anechoic duct of the gland.
- Computed tomography of the abdominal organs. Using this diagnostic method, it is possible to identify a formation if it is located in the wall of a hollow organ. This method also allows for differential diagnosis from malignant tumors. In the case of cancer, there is tumor invasion into adjacent abdominal organs and metastases. In this case, differential diagnosis with submucosal tumors (leiomyoma, lipoma, myosarcoma) may be difficult.
Types of operations on the pancreas
- Necrectomy (removal of dead tissue).
- Resection (removal of part of an organ). If removal of the head is necessary, pancreaticoduodenectomy is performed. If the tail and body are affected, distal resection is performed.
- Total pancreatectomy.
- Drainage of abscesses and cysts.
Surgeries for acute pancreatitis
It must be said that there are no uniform criteria for indications for surgery for acute pancreatitis. But there are several serious complications where surgeons are unanimous in their opinion: non-intervention will inevitably lead to the death of the patient. Surgical intervention is used when:
- Infected pancreatic necrosis (purulent melting of gland tissue).
- Ineffectiveness of conservative treatment within two days.
- Abscesses of the pancreas.
- Purulent peritonitis.
Suppuration of pancreatic necrosis is the most dangerous complication of acute pancreatitis. With necrotizing pancreatitis it occurs in 70% of cases. Without radical treatment (surgery), mortality approaches 100%.
Surgery for infected pancreatic necrosis is open laparotomy, necrectomy (removal of dead tissue), and drainage of the postoperative bed. As a rule, very often (in 40% of cases) there is a need for repeated laparotomies after a certain period of time to remove re-formed necrotic tissue. Sometimes, for this purpose, the abdominal cavity is not sutured (left open); if there is a risk of bleeding, the site of removal of necrosis is temporarily tamponed.
However, recently, the operation of choice for this complication is necrectomy in combination with intensive postoperative lavage: after removal of necrotic tissue, silicone drainage tubes are left in the postoperative field, through which intensive rinsing is carried out with antiseptics and antibiotic solutions, with simultaneous active aspiration (suction).
If the cause of acute pancreatitis is cholelithiasis, cholecystectomy (removal of the gallbladder) is performed simultaneously.
left: laparoscopic cholecystectomy, right: open cholecystectomy
Minimally invasive methods, such as laparoscopic surgery, are not recommended for pancreatic necrosis. It can only be carried out as a temporary measure in very sick patients to reduce swelling.
Pancreatic abscesses occur against the background of limited necrosis due to infection or in the long term when the pseudocyst suppurates.
The goal of treatment, as with any abscess, is opening and drainage. The operation can be performed in several ways:
- Open method. A laparotomy is performed, the abscess is opened and its cavity is drained until completely cleansed.
- Laparoscopic drainage: under the control of a laparoscope, the abscess is opened, non-viable tissue is removed, and drainage channels are installed, just as in case of extensive pancreatic necrosis.
- Internal drainage: the abscess is opened through the posterior wall of the stomach. This operation can be performed either by laparotomy or laparoscopically. The result is that the abscess contents exit through the formed artificial fistula into the stomach. The cyst is gradually obliterated, the fistula opening is tightened.
Surgeries for pancreatic pseudocysts
Pseudocysts in the pancreas form after resolution of the acute inflammatory process. A pseudocyst is a cavity without a formed membrane, filled with pancreatic juice.
Pseudocysts can be quite large in size (more than 5 cm in diameter), and are dangerous because:
- They can compress surrounding tissues and ducts.
- Cause chronic pain.
- Possibility of suppuration and abscess formation.
- Cyst contents containing aggressive digestive enzymes can cause vascular erosion and bleeding.
- Finally, the cyst may rupture into the abdominal cavity.
Such large cysts, accompanied by pain or compression of the ducts, must be surgically removed or drained. The main types of operations for pseudocysts:
- Percutaneous external drainage of the cyst.
- Cyst excision.
- Internal drainage. The principle is to create an anastomosis of the cyst with the stomach or intestinal loop.
Pancreatectomy
Resection is the removal of part of an organ. Resection of the pancreas is most often performed when it is affected by a tumor, in case of trauma, and less often in case of chronic pancreatitis.
Due to the anatomical features of the blood supply to the pancreas, one of two parts can be removed:
- The head together with the duodenum (since they have a common blood supply).
- Distal section (body and tail).
Pancreaticoduodenectomy
A fairly common and well-established operation (Whipple operation). This is the removal of the head of the pancreas along with the duodenum that surrounds it, the gallbladder and part of the stomach, as well as nearby lymph nodes. It is most often performed for tumors located in the head of the pancreas, cancer of the papilla of Vater, and also in some cases for chronic pancreatitis.
In addition to removing the affected organ along with the surrounding tissues, a very important step is the reconstruction and formation of the outflow of bile and pancreatic secretions from the pancreatic stump. This section of the digestive tract seems to be reassembled. Several anastomoses are created:
- The outlet of the stomach with the jejunum.
- Pancreatic stump duct with intestinal loop.
- Common bile duct with the intestine.
There is a technique for removing the pancreatic duct not into the intestines, but into the stomach (pancreatogastroanastomosis).
Distal pancreatectomy
Performed for tumors of the body or tail. It must be said that malignant tumors of this location are almost always inoperable, as they quickly grow into the intestinal vessels. Therefore, most often such an operation is performed for benign tumors. Distal resection is usually performed in conjunction with removal of the spleen. Distal resection is more associated with the development of diabetes mellitus in the postoperative period.
Distal pancreatectomy (removal of the tail of the pancreas along with the spleen)
Sometimes the size of the operation cannot be predicted in advance. If examination reveals that the tumor has spread very much, complete removal of the organ is possible. This operation is called total pancreatectomy.
Surgeries for chronic pancreatitis
Surgery for chronic pancreatitis is performed only as a method of alleviating the patient’s condition.
Drainage of the ducts (in case of severe obstruction of the ducts, an anastomosis with the jejunum is created).- Resection and drainage of cysts.
- Resection of the head for obstructive jaundice or duodenal stenosis.
- Pancreatectomy (with severe persistent pain syndrome, obstructive jaundice) in case of total organ damage.
- If there are stones in the pancreatic ducts that obstruct the outflow of secretions or cause severe pain, a virsungotomy operation (dissection of the duct and removal of the stone) or drainage of the duct above the level of obstruction (pancreatojejunostomy) may be performed.
Prices
| Disease | Approximate price, $ |
| Prices for examinations for stomach cancer | 5 730 |
| Prices for diagnosing Crohn's disease | 3 560 — 4 120 |
| Prices for diagnosing gastrointestinal cancer | 4 700 — 6 200 |
| Prices for hepatitis C diagnostics | 5 700 — 6 300 |
| Prices for treatment of Vater's nipple cancer | 81 600 — 84 620 |
| Prices for colorectal cancer treatment | 66 990 — 75 790 |
| Prices for treatment of pancreatic cancer | 53 890 — 72 590 |
| Prices for treatment of esophageal cancer | 61 010 — 81 010 |
| Prices for treatment of gallbladder cancer | 7 920 — 26 820 |
| Prices for treatment of nonspecific ulcerative colitis | 5 670 |
| Prices for treatment of stomach cancer | 58 820 |
| Prices for diagnosis and treatment of gallstone disease | 9 000 — 11 950 |
| Prices for the treatment of gastroenterological diseases | 4 990 — 8 490 |
| Prices for diagnosing Crohn's disease | 5 730 — 9 590 |
| Prices for treatment of viral hepatitis C and B | 5 380 — 7 580 |
| Prices for treatment of gastrointestinal cancer | 4 700 — 6 200 |