The effect of the pancreas on the heart can be called indirect, since there is no direct effect, but when the functionality of the organ is disrupted, the entire body suffers, including the cardiovascular system. Pain in pancreatitis has a particular effect, since it often causes a reflex change in heart rhythm
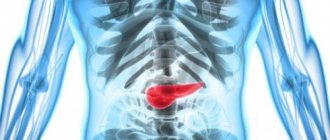
The pancreas (PG) is part of the digestive system and its role is to regulate mineral and lipid (carbohydrate) metabolism. The difficult location of the organ often does not allow diagnosing diseases in the early stages of development. When examining a patient, more attention is usually paid to the small intestine, liver, spleen, and stomach, which are located nearby.
The most common types of inflammation are pancreatic inflammation (acute and chronic), cancer and diabetes mellitus.
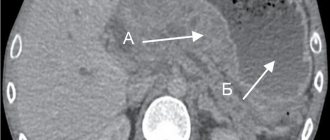
Laboratory and instrumental methods are used to diagnose pancreatic pathologies. In particular, a general blood test, biochemical diagnostics, electrocardiography, x-ray of the chest and abdominal cavity, etc. are performed.
Video: Pancreatitis and pain in the heart | Doctor Myasnikov “About the Most Important Thing”
Description of the pancreas
The pancreas is an oblong organ located in the abdominal cavity with digestive (exocrine) and hormonal (endocrine) functions. Located in the transpyloric plane. With the exception of the tail, the pancreas is mainly located in the retroperitoneal space, located deep in the upper abdomen in the epigastrium and its left regions.
In the abdominal cavity, the pancreas has direct anatomical connections with several structures: organs and choroid plexuses.
Organs:
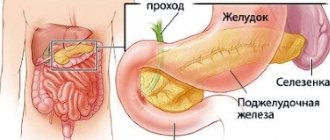
- Stomach - located separately from the pancreas, but at a close distance, since the stomach and pylorus lie in front of the pancreas.
- Duodenum - The duodenum curves in a “C” shape around the head of the pancreas. Part of the duodenum is located in front, while the second part of the organ is located on the side and to the right of the head of the pancreas.
- Transverse colon - attached to the anterior surface of the pancreas.
- Common bile duct - descends behind the head of the pancreas before opening into the second part of the duodenum next to the main pancreatic duct through the main duodenal papilla.
- The spleen is located behind and to the side of the pancreas. The linorenal ligament is formed from the peritoneum and connects the spleen to the tail of the pancreas.
The pancreas is located close to several large vessels, which are significant landmarks in vascular anatomy:
- The aorta and inferior vena cava pass posterior to the head of the pancreas.
- The superior mesenteric artery is located behind the pancreas.
- The posterior part of the pancreas, the splenic and superior mesenteric veins unite to form the hepatic portal vein.
- The splenic artery crosses the superior border of the pancreas.
Anatomical structure
The pancreas is anatomically divided into five parts;
- The head is the widest part of the organ. It lies in the C-shaped arch created by the duodenum and is connected to it by connective tissue.
- The uncinate process is a formation that arises from the lower part of the head and passes medially, therefore it lies as if under the body of the pancreas and behind the superior mesenteric vessels.
- Pancreatic notch (neck) - located between the head and body of the pancreas. It overlaps the superior mesenteric vessels, which form a groove in its posterior part.
- Body - located in the center, while crossing the midline, which allows this part of the organ to lie behind the stomach and to the left of the superior mesenteric vessels.
- The tail is the end of the pancreas, which is located on the left in close proximity to the spleen. It enters the splenorenal ligament with the vessels of the spleen. This is the only part of the pancreas that belongs to the intraperitoneal space.
Excretory function
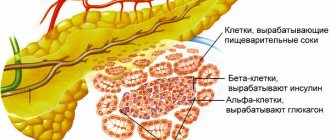
- The pancreas, which has an exocrine function, produces digestive enzyme precursors into the duodenum. The digestive fluid is produced by cells called acini, connected by short intercalated ducts.
- Intercalated ducts pass in the space that unites neighboring lobules and through them enzymes enter the network of intracavitary canals, which, in turn, are combined into the main canal of the pancreas.
- The pancreatic duct runs the entire length of the pancreas and unites with the common bile duct to form the hepatopancreatic ampulla of Water. This structure then opens into the duodenum through the large duodenal papilla.
- The process of secretion into the duodenum is controlled by a muscular valve - the sphincter of Oddi. It surrounds the ampulla of Vater, acting as a valve.
Blood network
The pancreas is supplied with blood through the pancreatic branches of the splenic artery. The head is additionally supplied by the superior and inferior pancreatoduodenal arteries, which are branches of the gastroduodenal and superior mesenteric arteries, respectively.
The venous network of the head of the pancreas is part of the superior mesenteric branches of the hepatic portal vein. The pancreatic veins, which arise from the rest of the pancreas, drain blood away from the organ through the splenic vein.
Lymphatic system
The pancreas is equipped with lymphatic vessels, located similarly to the arterial connection. The lymph nodes of the pancreas and pyloric intestine are connected to the upper mesenteric and abdominal lymphatic system.
Angina and heart attack under the guise of pancreatitis
Often, symptoms of pancreatic inflammation may hide problems with other organs, such as the heart. The heart is in close proximity to the pancreas, and in pathological conditions such as heart attack or angina, it can be difficult to determine the source. With these diseases, pain appears, radiating to the back and left shoulder.
Myocardial infarction
This is a dangerous, life-threatening condition. The danger also lies in the fact that for a long time it can be asymptomatic, and manifest itself only as pain in the abdomen or left arm. These referred pains are taken, in particular, for pancreatitis, as well as other diseases.
Pain in the area of the stomach and pancreas is manifested by the so-called abdominal infarction, which is a rather rare form of heart pathology.
In such cases, taking stomach medications (antacids and antispasmodics) does not bring significant relief. This means that the reason must be sought in something else. During myocardial infarction, pain develops progressively and reaches a peak within an hour. Taking nitroglycerin brings some relief. The appearance of pain is usually associated with great physical and psycho-emotional stress. Sometimes they occur after a heavy meal and may be accompanied by vomiting.
Angina pectoris
A very common disease, which is based on insufficient blood supply to the heart muscle. With angina, painful sensations vary in nature and intensity. They are usually localized behind the sternum. In some cases, referred pain appears in the epigastric region. They can be mistaken for a manifestation of acute pancreatitis or peptic ulcer of the stomach and duodenum. In this case, nausea often appears, turning into vomiting.
Various pathologies of the gastrointestinal tract may be accompanied by increased secretion. Excessive production of hydrochloric acid causes:
- nausea;
- heartburn;
- belching sour;
- epigastric pain.
These unpleasant symptoms are explained by insufficient production of digestive enzymes, which is typical for many gastrointestinal diseases, in particular pancreatitis. Such symptoms will allow the specialist to most likely exclude heart pathology.
With biliary dyskinesia and cholelithiasis, sharp, cramping or dull, aching pain appears in the right side. Problems with the gallbladder are a very common cause of chronic pancreatitis.
With angina pectoris and heart attack, pain occurs in the heart, radiating to the left side of the body. However, these symptoms are not always associated specifically with heart disease. Chest pain causes diseases of the musculoskeletal system, disorders of the digestive and respiratory systems. In any case, only a specialist can make an accurate diagnosis after conducting the necessary research.
Effect of the pancreas on the heart
The main organ in the cardiovascular system is the heart. This cone-shaped muscular organ can work automatically and at the same time performs an important function - it pumps blood throughout the body. The close location of the heart to the pancreas and stomach contributes to the fact that various inflammatory processes of these organs contribute to changes in cardiac activity.
The main cardiac disorders in pancreatic pain:
- Tachycardia - rapid heartbeat
- Extrasystole is an extraordinary contraction of the myocardium.
The features of the structure and equipment of the pancreas were indicated above. All this confirms the complexity of the organization of the organ and the importance of the influence it has on the entire body as a whole and on the heart in particular. Since with pancreatitis the first thing that worries the patient is pain, it is its presence and severity that significantly affects the functioning of the heart.
Pain causes an increase in blood pressure and heart rate by two main mechanisms that can act simultaneously.
- The sympathetic (autonomic) nervous system is stimulated through electrical pain signals that reach the central nervous system. This often occurs with acute pain, exacerbation, but can also occur with chronic pain. Aberrant neuroanatomical changes in the brain that can occur with severe persistent pain are capable of producing continuous sympathicotonia. As a result, excitation of the sympathetic department leads to changes in heart rate and pressure.
- When pain occurs, signals are sent to the hypothalamus and pituitary gland, which promotes the release of the hormone adrenocorticotropin (ACTH) , which stimulates the adrenal glands, which release adrenaline with a subsequent increase in heart rate and blood pressure.
The stronger the pain, the more pronounced the changes in the cardiovascular system may be. People who have previously been diagnosed with heart or vascular disease are especially susceptible to such disorders.
In such cases, the risk of myocardial infarction especially increases, since with severe pain the blood supply to the heart muscle is disrupted, which can lead to ischemia and necrosis.
If the pain does not go away for a long time, it is necessary to use suitable medications that may have been previously prescribed by a doctor. If this has not been done, then you should immediately contact a gastroenterologist, who will prescribe medications to eliminate pain due to pancreatitis, which will make it possible to normalize cardiac activity.
Symptoms of pancreatic diseases
People complain of severe pain in the pancreas with pancreatitis
The main symptom of the development of the disease in the organ is a feeling of acute pain, localized in the left hypochondrium and in some situations taking on a girdling character. Obvious signs may be nausea and vomiting, which intensify along with increased pain. Symptoms that may indicate the development of an inflammatory process in the pancreas:
- temperature rise
- persistent diarrhea (undigested food particles may be present in the stool)
- weight loss
- insomnia
- constant feeling of hunger, especially worse in the morning
- bloating that occurs after eating
- pain in the left hypochondrium
- frequent urination after eating
Diseases in the early stages are often not characterized by pain, but vomiting may nevertheless be present. Most often it manifests itself in the morning, or during meals: the stomach cramps, followed by a sharp attack of vomiting. After this, the patient's condition becomes somewhat easier.
Vomit may have a bitter or sour taste, depending on the degree of development of the pathology. The most likely cause of vomiting is pancreatitis. There are times when a person experiences an exacerbation on his own, without seeking help from a specialist. As a result, the disease can enter a chronic stage, worsening from time to time.
The human body is able to get used to pain and respond only to really strong outbreaks. Sometimes the pancreas increases in size and the patient feels it pressing on the ribs and preventing normal breathing.
It should be remembered that these symptoms are demonstrated by the pancreas not only against the background of excessive consumption of salty foods or alcohol. The human body has a certain “margin of safety” that allows it to independently regulate many negative processes that arise in it from time to time. This supply will be used up over time if the patient constantly neglects his health. As a result, the pancreas begins to report the disease too late, when the process of death of its tissues has begun.
Diseases of the pancreas have quite characteristic symptoms. The main one is pain in the left hypochondrium, which sometimes affects other areas of the body. Painful sensations are often accompanied by bouts of vomiting, an increase in the patient’s temperature, and other deviations in his functioning are observed.
Symptoms of disorders
First of all, with pancreatic diseases, patients are bothered by abdominal pain. The presence of this sign allows you to make a diagnosis almost immediately. Additionally, disorders of the heart and blood vessels of the following nature can be determined:
1. Tachycardia - the patient feels a rapid heartbeat, that is, a heart rate above 90 beats/min (in adults). Tachycardia may be accompanied by a feeling of weakness, lack of air, dizziness, loss of appetite, a feeling of anxiety or fear.
The cause of palpitations in pancreatic diseases may be increased body temperature, indicating intoxication of the body. Additionally, the patient may experience excessive excitability, which also affects the state of the cardiovascular system. If pain shock is extremely pronounced, then blood pressure decreases, which also contributes to the appearance of tachycardia.
2. Extrasystole - the patient has a feeling of interruptions in the heart, and a discomfort may also occur in the cardiac region. If during an attack it is possible to do electrocardiography, then, as a rule, extraordinary contractions are recorded that disrupt the normal rhythm of the heart. The more often such extrasystoles appear, the more pronounced the clinical manifestations are and the worse the patient feels.
The occurrence of extrasystoles in diseases of the pancreas, especially those accompanied by pain, is of a reflex nature. The situation worsens if the patient has increased nervousness or other negative emotions. Also, sometimes pancreatitis is accompanied by increased diarrhea and vomiting, which contributes to the removal of potassium from the body. This, in turn, can also contribute to heart rhythm disturbances and the occurrence of extrasystole.
PANCREATITIS – REVOLT OF THE PANCREAS
24.Dec.2019
With regular abuse of fatty and spicy foods, strong alcoholic drinks, one “fine” day you will definitely experience pain and heaviness in the abdomen, nausea, and indigestion. This will mean that the pancreas is “tired”, indicating its dissatisfaction with the manifestations of the first signs of pancreatitis
Despite its relatively small weight (80-90 grams), the pancreas plays a huge role in the functioning of the body. One of the most important functions is the production of special digestive enzymes and ensuring the digestion of proteins, fats and carbohydrates in the intestines. At the same time, the pancreas produces hormones (including insulin) that regulate blood glucose levels and the functioning of other body systems.
Sometimes, under the influence of various factors, the movement of digestive juices is disrupted. Liquids stop entering the small intestine and begin to corrode the tissue of the gland itself, causing severe inflammation of the latter - acute pancreatitis. Normal pancreatic tissue is gradually replaced by scar tissue. In the case when the endocrine parts of the gland are involved in the process, and subsequently are affected and die, then the person develops diabetes mellitus and the metabolism in the body is disrupted.
The first sign of acute pancreatitis is attacks of cutting pain in the pit of the stomach, intensifying after eating, the duration of which can take quite a long time. Often the pain radiates to the back, to the left and right hypochondrium, and can be girdling or simulating heart pain. The pain worsens if you lie on your back and gets better if you sit and lean forward. In addition, dry mouth, nausea, hiccups, belching, frequent vomiting, and diarrhea appear. In severe cases, the general condition quickly deteriorates: the temperature rises, the pulse quickens, shortness of breath appears, and blood pressure drops. In such a condition, you cannot do without medical help.
Risk factors
Doctors believe that the main causes of pancreatitis are alcohol consumption and gallbladder diseases, primarily cholelithiasis, in which the ducts of the gland become “clogged.” But there are other factors, including: diseases of the duodenum (gastroduodenitis, peptic ulcer), excessive food load (fatty and spicy foods), taking certain medications (antibiotics, paracetamol, sulfonamides, etc.), injuries, infections (hepatitis , mumps), obesity. In older people, the disease can appear when the blood circulation of the pancreas is impaired as a result of atherosclerosis. In addition, hereditary predisposition cannot be ruled out.
Diagnose and treat
Diagnosing pancreatitis in the early stages is not always easy. This requires laboratory and instrumental studies. In some cases, abdominal x-rays, computed tomography and laparoscopy will also be required.
It is very important to start treatment as quickly as possible to stop the progression of the disease. As a rule, in the first days, patients are prescribed medications that reduce inflammation and pain, suppress the activity of the pancreas, are prescribed a strict diet (sometimes even several days of fasting) and bed rest. In severe cases, surgical treatment is necessary.
When the disease cannot be curbed, the disease becomes chronic. And periodically, especially after culinary and alcoholic excesses, it makes itself felt with attacks of pain and unpleasant sensations in the abdomen. To get rid of them, various digestive enzymes are used (Mezim, Festal, Creon, etc.). These drugs should be taken with meals, Moreover, the required dose directly depends on what the person will eat. In addition, all patients need to promptly treat cholelithiasis and cholecystitis, and keep blood sugar levels under control.
The best prevention is the right food
A person who has experienced attacks of pancreatitis naturally does not want a repetition of the latter. Therefore, in order to enjoy life in the future, you have to follow some rules. First, train yourself to eat small portions 5-6 times a day (fractional meals). The menu should be dominated by protein products - lean boiled meat and fish, dairy products, egg whites. Secondly, you can’t overeat at night. Thirdly, it is important, despite the temptations, to give up fatty, spicy, fried, smoked foods and alcohol.
If you adhere to these principles, attacks of chronic pancreatitis will occur much less frequently.
Yulia Gudkova, general practitioner, Nyagan City Clinic
Medical treatment of pain due to pancreatitis
In 1986, WHO proposed an analgesic regimen for the treatment of severe pain. This treatment strategy was originally developed to relieve severe cancer pain. Later, the proposed method of pain relief was intended to eliminate pain due to causes other than cancer.
According to the WHO regimen, pain treatment begins with low-potency nonsteroidal anti-inflammatory drugs, which may be sufficient for mild to moderate pain due to pancreatitis. More and more potent NSAIDs are then gradually used, which may eventually be combined with opioids.
Previously, the WHO analgesic regimen was only partially useful for the treatment of patients with acute pancreatitis (AP) because opioid analgesics, especially morphine, have long been implicated in sphincter of Oddi dysfunction. However, several studies have shown that morphine does not have a significant adverse effect on acute pancreatitis. In a comparative study between metamizole and morphine, it was found that the former drug provided more frequent and faster pain relief than the same drug.
Additional studies have suggested pethidine as an analgesic when considering treatment for pancreatitis pain. However, buprenorphine, as a longer-acting analgesic, has similar analgesic potency to pethidine but a lower potential to cause physical opioid dependence.