Structure and functions of the liver
Externally, the liver is covered with a capsule. In the recess of the lower surface of the liver there is a gallbladder in the form of a sac with a volume of 40-70 ml. Its duct merges with the common bile duct of the liver.
Liver tissue consists of lobules, which in turn consist of liver cells - hepatocytes, which have a polygonal shape. They continuously produce bile, which collects into microscopic ducts that merge into one common one. It opens into the duodenum, through which bile enters. 500-1200 ml are released per day.
This secretion is formed in the liver cells and flows directly into the intestine (hepatic bile) or into the gallbladder, where it accumulates (vesical bile). From there, bile enters the intestine as needed, depending on the availability and composition of the food taken. If digestion does not occur, bile collects in the gallbladder. Here it is concentrated due to the absorption of water from it, becoming more viscous and cloudy compared to the liver.
Bile has the property of activating the digestive enzymes of the intestines, as well as emulsifying fats and, thus, increasing the surface area of interaction of enzymes (lipases) with fats, facilitating their breakdown. Bile has a detrimental effect on microorganisms, preventing their reproduction.
The composition of bile includes: water, bile acids, bile pigments, cholesterol, fats, inorganic salts, and enzymes (mainly phosphatases).
In addition to the participation of the liver in digestion, metabolism of carbohydrates, proteins, fats, vitamins, it has such leading functions as protective and neutralizing. The following are neutralized in the liver:
- Gut toxins (phenols);
- nitrogenous products of protein breakdown;
- alcohol;
- urea is synthesized;
- monosaccharides are converted into glycogen;
- Monosaccharides are formed from glycogen.
In addition, the liver also performs a certain excretory function. Metabolic products such as uric acid, urea, cholesterol, and the thyroid hormone thyroxine are excreted with bile.
In the embryonic period of development, the liver plays the role of a hematopoietic organ. It is now known that almost all blood plasma proteins are synthesized in the liver - albumins, globulins, fibrinogens, prothrombin and many enzymes.
The exchange of cholesterol and vitamins takes place in this gland, which shows that the liver is the leading biochemical “factory” of the body and needs to be treated with care. In addition, its cells are very sensitive to alcohol.
The role of the pancreas and liver in digestion
Food enters the body through the mouth and begins to be digested there. The esophagus, stomach - everywhere the food bolus is crushed by the muscles, irrigated by secretions, and slowly broken down by enzymes. Well, what happens to a former apple or steak under the influence of enzymes operating in the pancreas and liver? What do they turn into in the intestines? Let's follow this path.
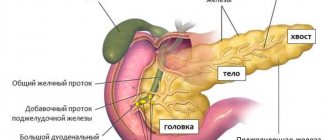
Pancreas
This gland, going around the duodenum, lies “in the rear” of the stomach, adhering to the posterior abdominal wall. It has the shape of a large cucumber, one edge of which is thickened, and a length of up to 20 centimeters, thus being the largest gland of mixed secretion.
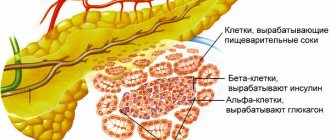
During external secretion
The pancreas secretes:
· Amylase, maltase - with their help, carbohydrates are broken down.
· Trypsin - it breaks down proteins.
· Lipase, which leads to the breakdown of fats with the participation of bile.
With internal secretion
it produces:
· Insulin - helps burn glucose in the cell, or converts glucose into animal starch glycogen.
· Glucagon - capable of breaking down starch (or glycogen) into glucose.
Features of pancreatic juice
1. The secretion of pancreatic juice is regulated in two ways: both unconditioned reflex and conditioned reflex. The center of the first regulation is the medulla oblongata, the second is the cerebral cortex.
2. Almost two liters of pancreatic juice are secreted in 24 hours. Moreover, there is more of it if hydrochloric acid and gastric juice enter the duodenum (this is how humoral regulation manifests itself).
3. Has a slightly alkaline reaction (pH 8-9), since an alkaline environment is needed to “turn on” pancreatic enzymes.
4. The acidic environment of the stomach contents when transporting food from the stomach to the duodenum becomes neutral or slightly alkaline, so food can easily be digested by pancreatic enzymes.
Liver
This vital, largest exocrine gland is divided into lobes and segments. It performs many tasks and is capable of regeneration - thanks to this property, such a branch of transplantology as transplanting part of the gland from a living donor is now being developed.
Liver structure
1. Special liver cells - hepatocytes
- secrete bile into bile capillaries, small initial structures.
2. Capillaries merge to form bile ducts (similar to venules in the circulatory system).
3. The ducts carry bile into the hepatic ducts (similar to veins in the circulatory system).
4. From them, as if from streams, bile flows into the “river” - a single bile duct (similar to the vena cava), which exits into the duodenum, or gall bladder.
Liver functions
1. Barrier
. Blood purification - harmful substances are neutralized by the liver and, together with bile, are released back into the intestines.
2. The liver is a blood depot
(along with the lungs, skin, spleen). It always contains 20-30 percent blood and in case of blood loss it urgently releases blood into the body.
3. Animal starch warehouse
. The liver contains significant reserves of glycogen, which is a reserve of sugars.
4. Gluconeogenesis
. The gland converts amino acids and glycerol into glucose, and then glucose into glycogen. This ability allows us to figuratively call the liver an “exchange point” that converts other substances into glucose.
5. Protein synthesis
. Half of the blood proteins are formed in the liver, primarily albumin proteins and blood plasma globulins.
6. Red blood cell breakdown
.
7. "Graveyard" of leukocytes
.
Features of the liver
1. The liver has its own “blood pipeline” - it enters through the hepatic artery
arterial blood enters.
2. Along the portal vein
blood comes to the liver with food and slightly “dirty” blood from the intestines, spleen, stomach, and pancreas. It is filled with food eaten by a person, but also with toxins (dyes, preservatives, etc.). The purpose of the portal vein is to pass substances collected in the gastrointestinal tract through the liver. They undergo filtration in the liver, are broken down, neutralized and then absorbed into the general bloodstream. Up to 70-80 percent of the blood received by the liver as a whole is infused through the portal vein.
3. Thus, in the liver there are two capillary systems: ordinary
, provided by the hepatic artery, between the arteries and veins, and
the capillary network of the portal vein
, which are nicknamed
the “miraculous network”
(between two venules). The veins of the portal vein branch into venules and pass inside the liver into other venules that collect into the hepatic vein.
4. The liver produces bile
, but does not synthesize digestive enzymes.
Bile, which has a slightly alkaline environment, leaves the liver into the gallbladder
(this “pouch” is adjacent to the lower part of the liver). It concentrates bile by absorbing mineral salts and water.
5. Gallstones
in the gallbladder are formed from cholesterol over many years and can cause a lot of problems for a person, clogging the bladder itself and the ducts.
6. In chronic alcoholics, secretory liver cells turn into connective tissue. Also, liver cells are very sensitive to nicotine.
The meaning of bile
1. Its key role is that bile acids facilitate the processing of fats by emulsifying them - breaking them down into small droplets.
2. Stimulates the activity of pancreatic and gastric gland enzymes.
3. Promotes the movement (peristalsis) of the intestine and the secretion of pancreatic juice.
Do you want to pass the exam with flying colors? Click here - preparation for the OGE in biology
General information about the study
The liver and pancreas are vital organs of the digestive system located in the upper abdominal cavity. The liver produces and secretes bile, which is necessary for the breakdown and absorption of fats in the intestines. The pancreas secretes enzymes that help digest carbohydrates, proteins and fats. In addition to participating in digestion, both organs perform many other functions. The liver ensures detoxification of harmful substances, regulates carbohydrate, protein and fat metabolism, accumulates vitamins and microelements, maintains hormonal balance, and synthesizes blood clotting and immune defense factors. The pancreas synthesizes hormones that regulate blood glucose levels.
The causes of damage to the liver and pancreas are varied, and often the pathological process occurs in both organs simultaneously. For example, cholestasis and impaired outflow of bile and pancreatic juice in diseases of the biliary tract (cholelithiasis with choledocholithiasis), hepatitis lead to reactive pancreatitis. Inflammatory or neoplastic diseases of the pancreas are often also accompanied by cholestasis and affect the liver. A common cause of pathologies of the liver and pancreas is alcohol abuse, poor nutrition, and overeating.
Damage to these organs often occurs unnoticed and proceeds for a long time without clinical manifestations. A disease of the liver and/or pancreas can be suspected if there is girdling pain and burning in the upper abdomen, heaviness and/or pain in the right hypochondrium, nausea, vomiting, bitterness in the mouth, bloating, change in color, quantity and consistency of stool, yellowness of the skin. .
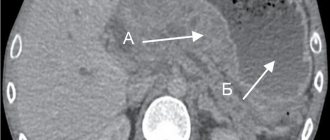
With the destruction of liver cells (cytolytic syndrome), the level of alanine aminotransferase (ALT) in the blood increases; with cholestasis syndrome, the concentration of bilirubin increases. Excessive activity of the lipase enzyme in the blood is a sign of damage to the pancreas. A simultaneous increase in all these laboratory parameters indicates the involvement of both the liver and pancreas in the pathological process, which most often occurs with a stone in the common bile duct.
An increase in individual test indicators requires additional laboratory and instrumental research methods in order to clarify the diagnosis and select adequate therapy.
What is the research used for?
- To assess the functional state of the liver and pancreas.
- For differential diagnosis of liver and pancreas diseases.
- To monitor a patient with chronic diseases of the hepatopancreatobiliary zone (cholelithiasis, cholelithiasis, chronic pancreatitis).
- To monitor the effects of certain medications to avoid side effects.
- In order to monitor the effectiveness of treatment of the liver and pancreas.
When is the study scheduled?
- With symptoms of possible damage to the liver and/or pancreas (girdling pain and/or burning in the upper abdomen, heaviness and/or pain in the right hypochondrium, nausea, vomiting, bitterness in the mouth, bloating, change in color, quantity and consistency of stool, yellowness, itching of the skin).
- When the structure and size of the liver and pancreas changes according to instrumental research methods.
- When examining persons who abuse alcohol.
- When taking drugs that affect the functions of the liver and pancreas.
- If one of your family members has already had liver and pancreas diseases.
- When monitoring patients with chronic diseases of the liver, pancreas, biliary tract, stomach and intestines.
- During a preventive examination.
Anatomy of the gastrointestinal tract
print version- home
- >
- For patients
- >
- Anatomy of the gastrointestinal tract
The digestive system includes organs that perform mechanical and chemical processing of food, absorption of nutrients and water into the blood or lymph, formation and removal of undigested food residues.
Food first enters the oral cavity, where during the chewing process it is not only crushed, but also mixed with saliva and transformed into a food bolus. This mixing in the oral cavity is carried out using the tongue and cheek muscles.
The mucous membrane of the oral cavity contains sensitive nerve endings - receptors, with the help of which it perceives taste, temperature, texture and other qualities of food. Excitation from the receptors is transmitted to the centers of the medulla oblongata. As a result, the salivary, gastric and pancreatic glands begin to work sequentially, then the bolus of food is swallowed through the esophagus into the stomach.
|
| The pharynx is a funnel-shaped canal lined with mucous membrane. The upper wall of the pharynx is fused with the base of the skull, at the border between the VI and VII cervical vertebrae of the pharynx, narrowing, and passes into the esophagus. Food enters the esophagus from the mouth through the pharynx. In addition, air passes through it, coming from the nasal cavity and from the mouth to the larynx. The crossroads of the digestive and respiratory tracts occurs in the pharynx. | Pharynx |
| The esophagus is a cylindrical muscular tube located between the pharynx and the stomach, 22-30 cm long. In the upper part of the esophagus there is an upper esophageal sphincter, in the lower part there is a lower esophageal sphincter, which play the role of valves that ensure the passage of food through the digestive tract in only one direction and prevent entry of stomach contents into the esophagus, pharynx, or oral cavity. The esophagus is lined with mucous membrane; in its submucosa there are numerous own glands, the secretion of which moistens food as it passes through the esophagus into the stomach. The movement of the food bolus through the esophagus occurs due to wave-like contractions of its wall - contraction of individual sections alternates with their relaxation. | Esophagus |
| The stomach is a pouch-shaped extension of the digestive tract, a distensible organ that is located between the esophagus and the duodenum. It connects to the esophagus through the cardiac opening, and to the duodenum through the pyloric opening. The inside of the stomach is covered with a mucous membrane, which contains glands that produce mucus, enzymes and hydrochloric acid. The stomach is a reservoir for absorbed food, which is mixed in it and partially digested under the influence of gastric juice. |
|
Gastric juice is produced by gastric glands located in the lining of the stomach. It contains hydrochloric acid and the enzyme pepsin .
These substances take part in the chemical processing of food entering the stomach during digestion. Here, under the influence of gastric juice, proteins are broken down. Thanks to these processes, food turns into a partially digested semi-liquid mass (chyme), which then enters the duodenum. The mixing of chyme with gastric juice and its subsequent expulsion into the small intestine is carried out by contracting the muscles of the stomach walls.
| The small intestine occupies most of the abdominal cavity and is located there in the form of loops. Its length reaches 4.5 m. The area of the inner surface of the small intestine increases due to the presence on it of a large number of finger-like outgrowths called villi. The small intestine contains many glands that secrete intestinal juice. This is where the main digestion of food and absorption of nutrients into the lymph and blood occurs. The movement of chyme in the small intestine occurs due to longitudinal and transverse contractions of the muscles of its wall. The small intestine, in turn, is divided into the duodenum, jejunum and ileum. |
|
The duodenum is the first of three sections of the small intestine.
It starts from the pylorus of the stomach and reaches the jejunum. The duodenum receives bile from the gallbladder (via the common bile duct) and pancreatic juice from the pancreas. In the walls of the duodenum there are a large number of glands that secrete an alkaline secretion rich in mucus, which protects the duodenum from the effects of acidic chyme entering it from the stomach. The jejunum is the middle section of the small intestine. The name “skinny” comes from the fact that when dissecting a corpse, anatomists found it empty. The jejunum makes up approximately two-fifths of the entire length of the small intestine. Loops of jejunum are located in the left upper part of the abdominal cavity. The length of the jejunum in an adult reaches 0.9 - 1.8 m. In women it is shorter than in men. In a living person, the intestine is in a tonically tense state. After death, it stretches and its length can reach 2.4 m.
The ileum is the lower portion of the small intestine, separated from the cecum by the ileocecal valve. The ileum is located in the lower right part of the abdominal cavity in the region of the right iliac fossa. The ileum is covered on all sides by peritoneum. There is no clearly defined anatomical structure separating the ileum and jejunum. However, there are differences between these two sections of the small intestine: the ileum has a larger diameter, its wall is thicker, and it is richer in blood vessels. The jejunal loops lie primarily to the left of the midline, and the ileal loops lie primarily to the right of the midline.
The large intestine is the lower part of the digestive tract, namely the lower part of the intestine, in which water is mainly absorbed and formed feces are formed from food gruel (chyme). The large intestine is 1.5 m long and is in turn divided into the cecum, colon and rectum. The colon primarily absorbs water, electrolytes, and fiber.
The cecum is the initial section of the large intestine and is a blind, sac-like area from 3 to 8 cm long. As a rule, it is completely covered by the peritoneum. It received its name due to its peculiar structure, reminiscent of a blind sac, into which the small intestine flows from the left side. Behind the junction of the small intestine with the cecum, a narrow, hollow, blindly ending vermiform appendix extends - the appendix, which is an appendage of the cecum. It is directed mostly towards the pelvis and is somewhat curved. However, the location of the process can be very diverse.
The colon is the main part of the large intestine, which consists of four sections:
- ascending colon,
- transverse colon,
- descending colon,
- sigmoid colon.
The rectum is the final section of the digestive tract. It gets its name because it runs straight and has no bends. Serves for accumulation and removal of feces. The length of the rectum is 15-16 cm. Feces accumulate in the area of the ampulla of the rectum, the diameter of which is 8-16 cm, but can increase with overflow or atony up to 30-40 cm. The final part of the rectum is directed back and down, called the anus the canal, passing through the pelvic floor, ends with an opening (anus).
Patient Materials
The GastroScan.ru website contains materials for patients on various aspects of gastroenterology:
- “Advice from doctors” in the “Patients” section of the site
- “Popular gastroenterology” in the “Literature” section
- “Popular gastroenterology” in the “Video” section
Video for students
Still from a video lecture by Dr. O.S. Tarasova “Physiology of Digestion” for students at the Faculty of Bioengineering and Bioinformatics of Moscow State University. M.V. Lomonosov.