The pancreas is an integral part of other gastrointestinal organs. If pain occurs, it can lead to health problems throughout the body.
The pancreas is the most important organ of the digestive system. It takes part in the processing and consumption of fatty acids (proteins, fats and carbohydrates) through the production of insulin. Also, the pancreas is directly involved in the digestive process. If a pathology forms in this organ, it will negatively affect the entire digestive system as a whole. Pain in the pancreas is a kind of signal indicating that the organ cannot cope with the load and needs help. There are a large number of diseases and pathologies that can negatively affect the functioning of the gland. It is very important to promptly determine the cause of the disease and begin effective treatment, which will avoid serious consequences and complications.
Pancreatitis: symptoms, treatment, nutritional features.
What is pancreatitis, what are the symptoms of the disease, what stages of pancreatitis are distinguished in medicine and what are the methods of treatment for each of them, what is included in the diet of patients with pancreatitis?
Pancreatitis is a collection of syndromes and diseases that manifest themselves as inflammation of the pancreas. This gland plays a very significant role in the body: it is responsible for normalizing digestive processes, regulating metabolism, and ensuring the digestion of proteins, fats and carbohydrates.
With the development of the inflammatory process, the enzymes secreted by the gland are not transferred to the duodenum, but continue to be activated directly in the gland, thereby destroying it from the inside. The main danger is that the released enzymes and toxins can enter the bloodstream and have a detrimental effect on the internal organs of a person - lungs, heart, liver, kidneys, brain. Today, pancreatitis is considered a fairly common disease - over the past 30-40 years, the number of cases of diagnosing inflammation of the pancreas has doubled. People with bad habits, prone to excessive intake of spicy, smoked and fatty foods are especially susceptible to the disease.
Pancreas - structure and main functions
Pain in the pancreas brings severe torment
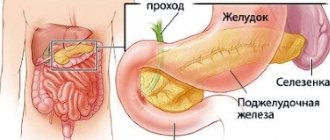
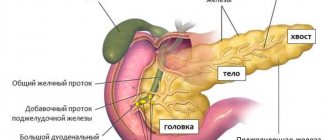
The pancreas is an organ of the digestive system located behind the stomach on the back wall of the abdomen. It is characterized by a peculiar shape, has a head, body and tail. The length is 16-22 cm, and it weighs about 80g.
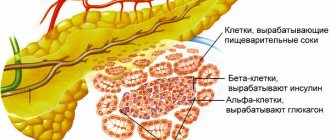
The gland has an alveolar-tubular structure. It is divided into grayish-pink lobules, each of which consists of glandular tissue and has its own system of excretory ducts. These small excretory ducts are connected to larger ones, which, in turn, are combined into a common excretory duct. The common excretory duct runs along the entire length of the organ and opens into the duodenum.
The lobules of the gland are formed from cells that produce pancreatic juice, rich in digestive enzymes. From the lobules, the secretion enters the duodenum through a common duct running along the entire gland. Between the lobules of the gland are groups of glandular cells, the so-called islets of Langerhans. These clusters of cells do not have excretory ducts; they produce insulin and glucagon directly into the blood. The gland has a mixed type of secretion, that is, it performs both endocrine and exocrine actions:
- The exocrine function is to participate in digestion. The gland produces pancreatic juice and carries it through the ducts into the duodenum. Every day, about 500-700 ml of juice is produced, which contains the enzymes necessary for digesting food - amylase, which helps convert starch into sugar; trypsin and chymotrypsin are enzymes responsible for protein breakdown; lipase, responsible for the breakdown of fat, etc. Thus, pancreatic juice is an important digestive juice necessary for the digestion of organic components of food.
- The endocrine function of the gland is to secrete glucagon and insulin, hormones involved in the regulation of carbohydrate metabolism.
The pancreas is in close relationship with other organs of the digestive tract. Any pathological process affecting it negatively affects digestion. Without the enzymes it produces, normal breakdown of food is impossible, and without the hormones glucagon and insulin, regulation of metabolic processes in the body is impossible.
Types of pancreatitis of the pancreas
In medicine, there are three main types of pancreatitis, the symptoms and treatment of which may differ:
- acute pancreatitis - characterized by segmental or complete inflammation of the gland, accompanied by suppuration, destruction of tissue structures, and in especially severe cases, hemorrhage;
- reactive pancreatitis - is the result of an exacerbation of acute pancreatitis and an attack of diseases of the internal organs;
- Chronic pancreatitis is characterized by a slow progression and can progress if not treated in a timely manner. A diet for pancreatitis can reduce pain; if the doctor’s instructions are not followed, the pain will return again.
Possible consequences
Pancreatic cancer
If you ignore the body's signals for a long time, this can lead to the most unfavorable consequences. Operation. Advanced forms of pancreatitis and pancreatic cancer require surgical intervention. Complete removal of the gland also has its negative consequences in addition to pain. This includes diabetes, which we will talk about separately, diarrhea, and increased gas production. In case of cancer, not only the pancreas, but also part of the stomach can be removed.
- Diabetes. With pancreatitis, the production of insulin in the blood is disrupted, which can result in such a dangerous disease as diabetes.
- Pancreatic abscess. An abscess usually occurs with severe pancreatitis associated with alcohol consumption. This disease is a suppuration of dead pancreatic tissue. In this case, severe abdominal pain occurs, fever, loss of appetite, and palpation reveals a tumor formation in the abdomen.
- Pancreatic necrosis. This is a very serious disease that occurs as a result of acute pancreatitis, as a result of which the cells of the pancreatic tissue begin to die. This is accompanied by severe abdominal pain, and intra-abdominal bleeding may occur. Patients suffering from pancreatic necrosis have to go through many unpleasant procedures: dialysis, surgeries, spinal catheters, drainage tubes. The treatment is quite long and painful.
- Death. The most terrible consequence of all possible. Death may occur as a result of cancer or pancreatic necrosis. Pancreatic cancer is quite rare and usually affects men. Since it is often detected in the last stage, the mortality rate is quite high.
- Vein thrombosis. Pancreatitis can lead to chronic thrombosis of the splenic vein. As a result, the spleen becomes enlarged, vomiting of blood, and pain are observed. The body's immunity also suffers, and the patient becomes a target for viral infections.
- Cholestasis. One of the complications of chronic pancreatitis is cholestasis - a disease associated with impaired flow of bile into the duodenum, in other words, it is stagnation of bile in the liver. The patient's skin turns yellow, itchy skin appears, and stool becomes discolored.
Very often, negative consequences result from self-medication when the time for real help is delayed. To prevent this from happening, it is important to contact a specialist as soon as possible when pain occurs.
Pancreatitis: symptoms
Pancreatitis of the pancreas can have different symptoms depending on the form of the disease. However, all types of the disease also have common symptoms - acute abdominal pain, which is localized in the part where the inflammatory process directly takes place. If the inflammation is located in the body of the gland, pain will occur in the epigastric zone; the inflammatory process in the tail is characterized by pain localized in the left hypochondrium; if the entire gland is affected, the pain will be girdling in nature and radiate to the back, sternum or shoulder blade.
The most severe pain is observed in acute pancreatitis, the symptoms in this case are as follows:
- pain in the upper abdomen that radiates to the back;
- nausea, in some cases with vomiting;
- temperature increase;
- disturbance during bowel movements;
- sometimes - jaundice.
The chronic stage is characterized by loss of appetite and loss of body weight, and the following signs are also observed:
- abnormal stool accompanied by a disgusting odor;
- nausea and vomiting when eating liquid food;
- flatulence, bloating and rumbling in the stomach;
- avitaminosis.
Pancreatic diseases - causes, symptoms, diagnosis
The list of diseases that can affect the organ is quite extensive. The most common disease is acute pancreatitis, which, if not adequately treated, can develop into chronic pancreatitis. Cancer is much less common.
Acute pancreatitis
Acute pancreatitis is based on the process of self-digestion of the gland’s own tissue. Normally, the enzymes secreted by the gland are in an inactive state. To activate inactive enzymes, it is necessary to have a sufficient amount of bile, which is present in the lumen of the duodenum. In acute pancreatitis, due to one reason or another, premature activation of enzymes occurs in the gland itself, and not in the intestines, which leads to damage to its tissues.
Pathological processes such as increased production of pancreatic juice, disruption of its outflow, and changes in its chemical composition lead to pancreatitis. Most often, the development of this disease is facilitated by the abuse of alcohol-containing drinks, the abuse of fatty and fried foods, traumatic injuries to the gland, diseases of the digestive organs (liver, biliary tract, duodenum), and diseases of the vascular system.
Treatment of pancreatitis of the pancreas
When you notice the first symptoms of pancreatic pancreatitis, you must definitely call an ambulance. Before doctors arrive, you must limit yourself to eating and drinking, as this can cause complications. It is recommended to take a horizontal position. To reduce pain, you can apply a heating pad with cold water or ice to the sore spot. You cannot take any medications on your own. If pancreatitis is chronic, treatment will consist of following a special diet, controlling emotions and avoiding alcohol. The acute form involves treatment with hunger, cold and complete rest. For 2-3 days, the patient must completely refuse food; he is allowed to drink still water, weak tea without sugar, and can eat only 4-6 days after an exacerbation of pancreatitis. To reduce the risk of relapse of pancreatitis, medications are prescribed in the form of enzymes, antispasmodics, pain relievers, and drugs to reduce acidity levels. Exacerbation of pancreatitis leads to the need for surgical intervention, the essence of which is to wash the abdominal cavity and remove the affected gland tissue.
Characteristic signs of inflammation
When the pancreas becomes inflamed, certain processes occur in the body, which cause the appearance of certain symptoms. When it becomes inflamed, the ducts of the gland through which digestive enzymes are released become narrowed, as a result of which they begin to accumulate inside it and digest their own cells, which leads to the following:
- bowel dysfunction – a person develops severe diarrhea;
- the appearance of severe pain, which can occur in both the left and right hypochondrium;
- disruption of digestive processes, which is manifested by a feeling of heaviness in the abdomen, flatulence, increased gas formation, etc.;
- paleness of the skin;
- a feeling of bitterness in the mouth;
- increased heart rate;
- lowering blood pressure.
Acute inflammation of the pancreas always manifests itself as severe pain
When the pancreas hurts, the patient cannot fully straighten up or lie on his back, as the acute pain simply paralyzes him. It begins to “twist”, as this allows you to at least slightly reduce the pain. In this case, the general clinical picture may be supplemented by aversion to food and the appearance of nausea, which develops into vomiting, after which the patient does not feel relief. And in some cases, when inflammation is complemented by a bacterial infection, a sharp increase in temperature to 38 degrees or more may be observed.
Important! It is necessary to understand that pain in the pancreas can also occur as a result of inflammation of other organs. Therefore, before starting treatment if pain occurs in the right or left hypochondrium, it is necessary to accurately establish the diagnosis. And only a doctor can do this after a thorough examination of the patient.
What can you do for pancreatitis?
The menu for pancreatitis must contain foods rich in vitamins and proteins with a minimum amount of fats and carbohydrates. This number includes:
- soups based on cereals, lean meat and vegetables;
- omelette with chicken eggs, lean fish and meats;
- cereals, pasta, crackers, stale bread, vegetable oil in limited quantities;
- slightly sour and dairy products, low-fat cheese and milk, butter;
- vegetables and fruits;
- juices from fruits and vegetables, rosehip decoction, tea with milk, a small amount of brine;
- honey, jam, limited amount of chocolate, berry jelly, sugar.
All ingredients must be ground, the method of preparation is boiling, baking, steaming. It is better to divide the food into 5-6 meals; it can be consumed warm.
Pain Management Clinic Specialists
Shapoval Nikolay Sergeevich Neurologist, Pain Treatment Specialist
Experience: more than 8 years
Details Make an appointment Call a doctor Online consultation
Sinelnikov Konstantin Andreevich Neurologist, Specialist in pain treatment
Experience: more than 10 years
Details Make an appointmentOnline consultation
Chernenko Valery Yurievich Neurologist, Specialist in pain treatment
Experience: more than 7 years
Details Make an appointment Call a doctor Online consultation
Tyulikov Konstantin Vladimirovich Neurosurgeon, Specialist in pain treatment, Doctor of the highest category, Candidate of Medical Sciences
Experience: more than 14 years
Details Make an appointment
Galperin Mark Yakovlevich Pain treatment specialist at the E. Malysheva clinic, anesthesiologist, algologist
Experience: more than 25 years
Details Make an appointment
Shubin Dmitry Nikolaevich Neurologist, chiropractor, Pain Treatment Specialist at the E. Malysheva Clinic
Experience: more than 30 years
Details Make an appointment
Trushin Pavel Vadimovich Neurosurgeon, Candidate of Medical Sciences
Experience: more than 10 years
Details Make an appointment
Ivanyuk Andrey Genrikhovich Neurologist, reflexologist, doctor of the highest category
Experience: more than 26 years
Details Make an appointment
What should you not eat while on a diet for pancreatitis?
In case of pancreatitis, it is necessary to completely exclude from the diet fatty, spicy, fried, salty, smoked foods, fast food, and foods that increase the formation of gases and the secretion of gastric juice. The consumption of alcoholic and even low-alcohol drinks is strictly prohibited. You should not eat such dishes as mushrooms, fatty creams, fatty meats and fish, kebabs, whole eggs, sour cream, marinades and pickles, seasonings and vinegar, spinach, radishes, onions and garlic, bananas, ice cream, cocoa and coffee, grapes and juice from it, figs and dates, sorrel. It is advisable not to consume milk in its pure form; it is better to add it to porridge or tea.
Causes of pancreatitis
In most cases, pancreatitis develops as a result of cholelithiasis (stones can obstruct the outflow of pancreatic secretions), or as a result of alcohol abuse.
Women at risk are during pregnancy and in the early postpartum period. Monotonous food, overeating and consumption of low-quality foods (including fast food) can also cause an attack of acute pancreatitis.
Other factors contributing to the development of pancreatitis include:
- diseases of the stomach and duodenum;
- tumors;
- injuries;
- parasites (worms);
- taking certain medications, such as furosemide, estrogens, antibiotics, sulfonamides;
- metabolic disease;
- hormonal changes;
- vascular diseases.
Most often the disease is registered between the ages of 40 and 60 years.
Treatment of pancreatitis in medical
Medical in St. Petersburg is a multidisciplinary medical institution operating according to European standards. The Institute of Gastroenterology has been founded at our clinic, where you can undergo a full diagnostic examination if pancreatitis is suspected. Qualified specialists with many years of experience will quickly make an accurate diagnosis and prescribe effective treatment, and also develop a special menu for you for pancreatitis. With strict adherence to the diet, a person can live peacefully for many years and feel great, forgetting about attacks of pain. Our center successfully practices an electronic system for registering patients and maintaining cards, and confidential communication between patients and doctors contributes to a speedy recovery. Clinic "Energo" is your main assistant in the fight against pancreatitis of the pancreas!
general information
To understand what symptoms inflammation causes, you first need to know exactly where the pancreas is located in a person. And the pancreas is located behind the stomach, tightly adjacent to it with its body. Its tail and head seem to envelop it, adjacent to other nearby organs.
For example, the tail of the gland is located on the left side near the spleen, and its head is located on the right side, closely adjacent to the duodenum and connected to it by tubules through which pancreatic juice and bile are released. Given this location of the gland, when it becomes inflamed, various symptoms arise, from which it is difficult to understand that the pancreas is hurting, since there is a feeling that the painful sensations are localized in completely different organs, for example, in the spleen or stomach.
However, there are characteristic signs that allow you to know that the occurrence of pain is associated specifically with inflammation of the pancreas. We will talk about them now.
How to determine the cause of pain?
The health of the pancreas can be checked using the results of a comprehensive diagnosis, which includes instrumental and laboratory tests. The first measures were taken as a basis - using special devices:
- Ultrasound analysis, which helps to identify changes in the structure (heterogeneous areas of tissue, etc.) and size of the organ. This method can detect polyps, cysts, as well as determine the size of the pancreatic ducts and identify diffuse echographic signs of diseases.
- Elastography, which allows you to determine the level of tissue elasticity, even in the form of minor changes. This is a type of ultrasound diagnosis, the results of which can be used for histological analysis.
- Computed tomography, which can be used to identify moderate and pronounced diffuse changes in the organ. This method determines the size and shape of the organ, detects various neoplasms (cysts, tumors, etc.), and changes in the ducts.
- Computed tomography using contrast helps to find out how narrowed the pancreatic ducts are.
An alternative to the last diagnostic measure is endoscopic cholangiopancreatography.
Lab tests
Instrumental diagnostics are carried out to identify structural and histological changes, changes in the size of organs such as hepatosplenomegaly (enlarged spleen and liver). Laboratory tests are required to determine the functional characteristics of the gland.
You can understand how fully the endocrine function of the pancreas is performed by the pancreas (the level of insulin secreted into the blood, which is involved in the body’s absorption of glucose) by analyzing the volume of glucose and amylase.
A more informative analysis in this case is the secretin-pancreozymine test. Despite the fact that it gives almost 100% results, there is one drawback - poor tolerance by the human body. Other laboratory tests that are prescribed to identify signs of pancreatic disease accompanied by pain:
- analysis of pancreatic enzymes in stool;
- analysis for hydrolysis products in feces;
- analysis for hydrolysis products of substrates in exhaled air.
Based on the results of a comprehensive diagnosis, the doctor makes a final diagnosis and prescribes treatment that helps not only to cope with pain, but also to suppress the activity of the inflammatory or other etiology of the pathological process in the organ.
How to get rid of pain due to glandular diseases?
Pain syndrome is one of the clinical manifestations of a primary organ disease. Although there are many methods for relieving discomfort, you need to focus your efforts on treating the underlying pathology, since with symptomatic measures it will progress.
In case of acute pancreatitis, it is forbidden to carry out therapy at home, but you should consult a doctor. Otherwise, death is possible.
It is recommended to fast for the first day. Only drinking mineral alkaline water is allowed. To relieve pain, you can apply a cold compress to the area of discomfort. If this method does not help, medications with antispasmodic effects will be effective. These include medications No-shpa and Papaverine.
Other drugs that help relieve pain in pancreatic disease include Atropine and Novocaine. Experts do not recommend treating pain syndrome with drugs with the following names: Nise, Aspirin. The tablets help irritate the membranes of the digestive system and thin the blood. Etiotropic treatment of thyroid disorders:
- tablets Omeprazole, Allochol, Contrical to reduce the level of fluid produced;
- herbal preparations Digestal, Befungin, Creon for organ cleansing;
- anti-infective agents Ampicillin, Gentamicin, etc.
At home, you need to maintain proper nutrition.
Useful and prohibited foods
Prohibited foods that should not be eaten if organ function is impaired include:
- alcoholic drinks;
- fatty, fried;
- sweets;
- food with simple carbohydrates and coarse fiber;
- fast food and semi-finished products.
List of useful products for the period of treatment of acute inflammatory process:
- meat and fish;
- dairy and fermented milk products;
- vegetable and cereal soup;
- fresh vegetables and fruits;
- dried wheat bread;
- boiled eggs or as an omelet;
- jelly, juice, compote;
- vegetable and butter.
Approximate meals for a week can be placed in the table:
| Day of the week | Breakfast | Dinner | Afternoon snack | Dinner |
| Monday | Oatmeal porridge, tea without added sugar | Puree vegetable soup, boiled fish or chicken | Baked apples | Steamed vegetables, chicken meatballs |
| Tuesday | Eggs in the form of an omelet, compote | Milk soup | Cheese casserole | Mashed potatoes, boiled meat, juice |
| Wednesday | Buckwheat porridge, tea without added sugar | Boiled vegetables, boiled fish, jelly | Compote and oatmeal cookies | Vegetable puree |
| Thursday | Boiled risk, tea | Pumpkin soup in the form of puree, steamed meat | Eggs in the form of an omelet, fruit drink | Chicken and vegetables stew |
| Friday | Semolina, compote | Lean fish soup | Baked fruits | Rice porridge and veal stew |
| Saturday | Cottage cheese casserole, tea without added sugar | Steamed chicken cutlets, pasta | Crackers and yogurt | Buckwheat porridge, meatballs, jelly |
| Sunday | Milk soup, juice | Buckwheat soup, boiled chicken | Crackers and jelly | Fish casserole, fruit drink |
Alternative therapy
Clinical manifestations of pancreatic disease can also be eliminated with folk remedies that act symptomatically. These could be dill seeds. An infusion is prepared from them: 1 tsp. seeds are poured with hot water in a volume of 250 ml, left to infuse for 1 hour, filtered. The finished infusion is taken orally throughout the day instead of tea in small sips.
Products such as lemon, garlic and parsley enjoy good reviews, from which the following potion is prepared:
- take 3 lemons, 3 heads of garlic and 100 g of parsley;
- Grind the ingredients with a meat grinder until a homogeneous mixture is obtained;
- place the composition in a glass jar and leave to infuse for a day;
- take 1 tsp. mixture before meals.
No less effective are medicinal herbs, for example, chamomile and immortelle: take 1 tbsp. herbs, pour 1 glass of hot water, leave, strain, take 100 ml twice a day before meals.