The human digestive system is a complex of hollow organs through which food passes, covering a distance of 4-5 meters from the mouth to the rectum. The stomach is part of this route, the first stop of ingested food, where it mixes with gastric juices before moving on. The organ also performs immunological functions and is connected to a network of specialized nerves that are not found in any other part of the digestive tract.
What is a stomach?
The stomach is a hollow, sac-like organ of the initial section of the digestive tract. Partially crushed food from the esophagus enters it. The border between them is a special sphincter, which is normally closed and prevents the backflow (reflux) of stomach contents into the esophagus, no matter what position the human body is in. When swallowing, it relaxes.
5 facts about the stomach
- Stomach distension from overeating is an unscientific myth.
- Belching is a natural process by which the stomach gets rid of excess air that is swallowed when eating.
- The stomach produces hydrochloric acid in concentrations that can dissolve muscles, bones and some metals.
- When we blush, our stomach also turns red due to the influence of the sympathetic nervous system.
- Thoughts about the taste and smell of food stimulate the production of gastric juice.
How is the size of the stomach determined?
Fluoroscopy can be used to determine the size of the stomach.
To diagnose an enlarged stomach in modern medicine, the following diagnostic methods are used:
- X-ray
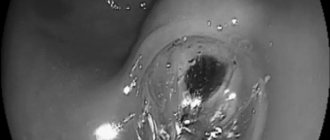
- Gastroscopy
- Computer diagnostics
To determine the size of the stomach using fluoroscopy, the patient is given a special liquid to drink. Then the specialist uses X-rays to obtain an image of the organ on a fluorescent screen. Today, X-ray television examination is used, during which the resulting image can be further processed in order to better diagnose the disease. The image remains in the device's memory and on the film.
Gastroscopy is performed to examine the inner surface of the stomach and its mucous membrane. A tube with a camera is inserted through the throat and esophagus into the patient's stomach. The image from the camera appears on the monitor. If necessary, the image is recorded. During the procedure, it is possible to conduct additional diagnostics: taking tissue for a biopsy. Computed tomography of the stomach has a number of advantages compared to other diagnostic methods:
- No special liquid is used during the study.
- Provides a more complete image in several projections compared to radiography.
- Does not cause pain during the procedure, compared to gastroscopy.
Functions and role of the stomach in the body
The stomach performs the following functions²:
- Deposition and mechanical processing. Food stays in the stomach for several hours, swelling and liquefying.
- Partial digestion (chemical processing) of food. It is carried out thanks to gastric juice, which is produced by special cells located in the mucous membrane. On average, a person secretes about 2-2.5 liters of juice per day. It has an acidic reaction (pH 1.5-1.8), consists of water, hydrochloric acid, mucus and enzymes.
- Portioned evacuation of the food bolus into the small intestine. Happens approximately every 20 seconds. Slow gradual passage is necessary to neutralize the acidic contents with the alkaline pancreatic juice - until the bolus of food reaches the delicate mucous membrane of the small intestine.
- Secretion of biologically active compounds: serotonin, histamine, motilin, gastrin, substance P, ghrelin (hunger hormone).
- Absorption of some substances: water (partially), amino acids, a small part of ethanol from alcoholic drinks, caffeine, medications (aspirin), a small proportion of water-soluble vitamins.
- Neutralization and/or destruction of pathogens (immunological protection).
- Isolation of Castle factor, necessary for the absorption of vitamin B12 from foods.
The stomach is one of the first lines of defense of the immune system. It not only digests food, but also sterilizes it. The chemical treatment process kills or weakens bacteria and toxins. Thanks to accumulations of lymphoid protective cells, information is transmitted to other immunocompetent organs during the passage of viruses, helminths, and bacteria³.
All food taken does not mix with gastric juice. As chemical and mechanical treatment proceeds, its layer adjacent to the mucous membrane moves to the central part of the organ. From there, the lump is slowly evacuated in small portions into the duodenum.
The food bolus remains in the stomach for 1.5 to 6 hours, while the time of its evacuation depends on the chemical composition of the food consumed. Dishes rich in fat and protein are delayed for a longer period. While foods containing carbohydrates pass much faster⁵. Partially processed food has a special name - chyme. It looks like a thick viscous mass.
Figure 1. Functions of the stomach. Image: ChiaraLoveStar / freepik.com
Pathology of the stomach and esophagus on ultrasound
Types of pathological changes in the stomach on ultrasound
Despite the difficulties of visualizing the stomach on ultrasound, due to the presence of a cavity in the organ, the accumulation of gases and the constantly changing shape due to peristalsis, the sonography method allows one to obtain fairly extensive and high-quality information about the condition of the stomach, on the basis of which various pathologies are identified.
Ultrasound signs of gastric pathology are the following:
- change in organ shape;
- change in the diameter of the gastric lumen;
- change in wall thickness;
- the presence of irregularities on the inner or outer surface of the stomach wall;
- the presence of bulges on the wall of the stomach;
- lack of peristalsis;
- presence of antiperistalsis.
The main sign of stomach pathology is thickening of its walls and expansion/narrowing of the lumen of the organ. Thickening of the walls of the stomach with a characteristic uneven echogenicity, when the outer part of the wall is hypoechoic compared to the hyperechoic inner part, is called a symptom of damage to a hollow organ. Currently, in the world medical literature, the terms “target”, “lesion halo”, “pseudo-kidney”, “bull’s eye”, “pathological type of cockade” are also used as synonyms for the term “symptom of lesion of a hollow organ”. All of the above terms refer to the same pathological condition of the stomach, and therefore can be used as equivalent. However, in the countries of the former USSR, the most commonly used term is “symptom of an affected hollow organ,” which we will also use.
Thus, thickening of the stomach wall, as a symptom of an affected hollow organ, can be diffuse and limited. With diffuse thickening, ultrasound shows an increase in wall thickness along its entire length. And with limited thickening, the wall of the stomach turns out to be thicker than normal only in a certain limited area. Unfortunately, the two main pathological signs of stomach diseases detected by ultrasound, namely the symptom of the affected hollow organ and the expansion/narrowing of the organ lumen, are nonspecific. This means that these pathological signs are inherent in many diseases, as a result of which it is impossible to accurately diagnose using ultrasound data alone.
In order to correctly diagnose a person’s existing stomach disease and choose one of the many pathologies that are characterized by a symptom of an affected hollow organ or a change in the lumen of the organ, it is necessary, in addition to the ultrasound results, to also evaluate the clinical symptoms that worry the patient. Only a combination of pathological changes on ultrasound with clinical symptoms will help make the correct diagnosis. Below, for general orientation in the problem, we will provide a table in which we will indicate which diseases of the stomach are characterized by the presence of symptoms on ultrasound of the affected hollow organ and changes in the lumen of the organ.
| Diseases characterized by an ultrasound symptom of an affected hollow organ with diffuse wall thickening | Diseases characterized by an ultrasound symptom of an affected hollow organ with limited wall thickening | Diseases that are characterized by narrowing or widening of the lumen of the stomach cavity on ultrasound |
| Swelling of the stomach wall | Pyloric stenosis | Scar stricture |
| Chronic gastritis type B | Ulceration of carcinoma | Inflammatory stenosis |
| Ménétrier's disease | Stomach ulcer | Tumor-induced stenosis |
| Infiltrative carcinoma | Varicose veins | Impaired evacuation of gastric contents |
| Malignant lymphoma | Gastric carcinoma |
Swelling of the stomach wall can be observed in acute pancreatitis, nephrotic syndrome, congestive heart failure, as well as protein deficiency in the body. Pyloric stenosis can be congenital or acquired due to inflammation, ulcers or tumors.
Ultrasound picture for various diseases of the stomach
Currently, there are six main pathological processes of the stomach that can be accurately diagnosed using ultrasound - these are erosive and ulcerative lesions, polyps, pyloric stenosis, duodenogastric reflux, malignant tumors and malformations. Below we present the characteristic features of the ultrasound picture for the six different above-mentioned pathologies of the stomach, as well as damage to the organ.
Ultrasound picture of the developmental defect “pyloric stenosis”. With congenital pyloric stenosis, a baby develops persistent vomiting of gastric contents at 2–4 weeks of life. Ultrasound shows a pronounced symptom of the affected hollow organ, namely: sharp thickening of the walls in the antrum, narrowing of the walls in the central part and the general appearance of the stomach as an “hourglass”, as well as the presence of contents in the stomach more than 24 hours after eating. Ultrasound picture with the developmental defect “duplication of the stomach” Using an ultrasound, it is possible to establish a doubling of the stomach only by performing a water-siphon test so that both cavities are filled with water and the doctor can clearly see them. A diverticulum is an area of protrusion in the wall of an organ.
Such diverticula can be single or multiple; on ultrasound they are visible only during a water-siphon test, when their lumen is filled with water and makes them visible. A diverticulum filled with water is an anechoic formation of any shape, bulging away from the wall of the stomach and connected to its cavity by a thin stalk. Damage to the stomach usually occurs due to mechanical impacts on the area where the organ is located, for example, from blows to the stomach, a fall from a height onto the stomach, etc. Such damage to the stomach can manifest itself as bruises, tears and ruptures of the walls of the organ. Less commonly, there are injuries caused by chemical substances, the picture of which on ultrasound is different from mechanical injuries.
Gastric contusion is characterized by limited, weakly echogenic thickening or bulging of the wall in the area of injury. The bruise is better visible when performing a water-siphon test than on an empty stomach. A rupture of the stomach wall is characterized by an uneven contour of the walls and their interruption in the area of \u200b\u200bthe rupture. When performing a water-siphon test, a rupture is easily diagnosed, since an ultrasound immediately shows the place where water leaks into the abdominal cavity. Chemical damage to the stomach wall is characterized by its thickening and doubling of the contour (an echo-negative stripe on the outside and an echo-positive stripe on the inside).
If, as a result of the damage, a cicatricial narrowing of the stomach cavity has developed, then an ultrasound will reveal fluid and food debris taken more than 14 hours ago. A gastric ulcer on an ultrasound looks like a hyperechoic thickening of the wall with its deformation and narrowing of the lumen. In addition, an excess amount of fluid on an empty stomach is recorded, a symptom of damage to a hollow organ. The following sizes of various parts of the stomach according to ultrasound are characteristic:
- outer diameter 16 – 22 mm;
- thickening of the wall of the gastric outlet from 6 to 10 mm;
- the distance between the walls in the thickening area is 7 – 12 mm;
- image factor 0.5 – 3.3 mm.
When performing a water-siphon test for a stomach ulcer, the following symptoms are characteristic:
- a clear, uneven contour of the wall in the area of the ulcer with hyperechoic inclusions;
- uneven thickening of the internal hyperechoic layer of the stomach up to 2 – 4 mm;
- the wall thickness in the area of ulcer or erosion is always more than 5 mm;
- indistinct layering of the wall in the area of the ulcer;
- inactive peristalsis.
Ultrasound picture for gastritis The walls of the stomach are evenly thickened, their echogenicity is uneven, with alternating hypoechoic and hyperechoic areas, more than 40 ml of fluid is detected in the cavity on an empty stomach, the diameter of the pylorus is more than 10 mm, signs of duodenogastric reflux. Stomach peristalsis is sluggish. Menetrier's disease is a giant hypertrophic gastritis, in which the gastric mucosa forms huge folds with polyp-like growths. Ultrasound shows a highly thickened wall with uneven echogenicity. Peristalsis is sluggish. A large amount of liquid and food taken more than 14 hours ago is found in the stomach.
A typical symptom is a lesion of a hollow organ with a thickening of the wall in the area where the polyp is located up to 20–28 mm, and a gap between the walls in the area of the thickening of 3–12 mm. There is also an uneven structure of the stomach wall in the area of thickening, the image coefficient in the area of the polyp is 0.9 - 9. The amount of fluid in the stomach on an empty stomach is normal. When performing a water-siphon test on ultrasound, a polypoid bulging of the wall into the lumen of the stomach is clearly visible. The structure of the polyps is heterogeneous, there is no layering.
Ultrasound picture for malignant tumors of the stomach
There is always a symptom of damage to a hollow organ above the area where the tumor is localized. The wall is thickened unevenly (from 10 to 30 mm), the thickening area is hypoechoic, heterogeneous, with impaired layering. The outer contour of the stomach wall in the area where the tumor is located is uneven, but clear. The lumen of the stomach in the tumor area is 2 – 16 mm. The lower border of the greater curvature of the stomach is lower than normal. The amount of fluid in the stomach on an empty stomach is either within normal limits or slightly increased. When performing a water-siphon test, uneven filling of the cavity with water and its insufficient expansion are noted. Rigidity of the thickened wall and sluggish peristalsis are also characteristic. The internal contour of the stomach is hyperechoic, fragmented and thickened more than 3 mm. In the area of the tumor, the outer and inner contours of the stomach are uneven, but clear. Pyloric stenosis is a narrowing of the outlet of the stomach, due to which the evacuation of food masses into the duodenum is impaired.
The causes of pyloric stenosis are usually tumors or a long course of a peptic ulcer, as a result of which scars are formed that tighten the walls of the stomach and reduce the lumen of its pyloric part. Pyloric stenosis is characterized by a shapeless hyperechoic formation with a sharp narrowing of the lumen of the affected area. At the initial stage, the walls of the stomach are thickened, but then they become thinner and the cavity expands. An ultrasound shows that the stomach is dilated and filled with contents of different ages. The amount of fluid on an empty stomach is more than normal, and there is sediment in it. The lower limit of the greater curvature of the stomach is significantly lower than normal. Peristalsis is either absent or weak. In the area of stenosis there is a symptom of damage to a hollow organ, and the wall is thickened to 7 - 22 mm, it has no layering, and the image coefficient is 0.6 - 8.5. When performing a water-siphon test for pyloric stenosis, the patient can only drink a small amount of liquid – no more than 300 ml, due to a feeling of fullness in the abdomen, nausea and sometimes vomiting. When liquid enters the stomach, its contents are mixed and sediment floats to the surface.
The lower border of the greater curvature drops even lower than when examined on an empty stomach. Peristalsis is sluggish or absent. It is impossible to visualize the normal layering of the stomach wall in the area of stenosis. Duodenogastric reflux is a pathological condition in which the contents of the duodenum are refluxed into the stomach. Reflux is detected during a water-siphon test, and on an empty stomach it can be seen on an ultrasound only if there is an accumulation of fluid in the patient’s stomach in an amount greater than normal. On ultrasound, reflux is visible by the retrograde movement of hyperechoic particles from the duodenum up the stomach after filling it with water. The presence of fluid in the stomach on an empty stomach in an amount of more than 40 ml may indicate a peptic ulcer, gastritis, pyloric stenosis or a malignant tumor. In order to understand exactly what disease the fluid in the stomach indicates in a particular case, you need to take into account other signs on ultrasound, as well as the clinical symptoms that the person has.
Pathological changes in the esophagus and ultrasound images in various diseases
Pathological changes in the esophagus on ultrasound are changes in the diameter, wall thickness, length of the abdominal organ, as well as the angle of His. Let's consider what ultrasound signs are characteristic of various pathologies of the esophagus. GER is a pathological reflux of stomach contents into the esophagus. And GERD is damage to the lining of the esophagus due to reflux. GER and GERD are characterized by expansion of the lumen of the esophagus on ultrasound and thickening of its wall. Chalazia is weak peristalsis, as a result of which food stagnates in the esophagus, moving only under the influence of gravity.
On ultrasound, chalazia of the esophagus is characterized by expansion of the lumen of the organ and thickening of its wall. Chalazia cardia is characterized by a gaping of the distal esophagus up to 6–14 mm, as well as visible flow of stomach contents into the esophagus. Cardiospasm is a pathological increase in the tone of the esophagus, as a result of which food does not move well to the stomach. Cardiospasm on ultrasound is characterized by expansion of the thoracic esophagus and at the same time a sharp narrowing of the esophageal-gastric junction to 3 - 5 mm. Stagnant contents are visible in the lumen of the esophagus, the wall of the organ is slightly thickened.
Structure of the stomach
The shape of the stomach resembles a pear, but it constantly changes depending on the nature and volume of foods eaten, body position, and individual characteristics of the person. The organ consists of the following parts¹:
- the cardiac opening with the cardiac part adjacent to it is the entrance to the stomach;
- the bottom (fundus or fornix) is a dome-shaped extension that is located slightly above the cardial opening;
- body - the largest part of the organ, located between the fornix and the pylorus;
- greater curvature - the convex side directed to the left and down;
- pylorus (pylorus or pyloric part) - exit section;
- lesser curvature - concave side directed upward and to the right;
- the opening of the pyloric canal with the circular muscle - sphincter.
Figure 2. Structure of the stomach.
Image: sciencepics / Depositphotos Anatomically, the stomach has two walls - anterior and posterior. They consist of four layers²:
- The mucous membrane is in the form of various folds and gastric fields. Equipped with many glandular cells that produce biologically active substances (pepsinogen, hydrochloric acid, mucus, etc.). Also in the mucosa there are single accumulations of lymphatic tissue.
- Submucosa. Contains blood vessels and nerves.
- Three layers of muscles - oblique, circular, longitudinal.
- The serous membrane (peritoneum), separated from the muscular layer by the subserosal base. Absent from a small area of the posterior wall, where the stomach is in contact with the diaphragm, less commonly the adrenal gland or the upper pole of the left kidney.
The stomach is the widest part of the digestive tract. The average volume of an empty organ is 500 ml. In the process of eating, it stretches to 1-2 liters, rarely - up to 4 liters.
Neighboring organs
The anatomy of the human stomach is inextricably linked with the condition of neighboring organs. Therefore, it is important for a doctor to know the topography; we can call it a “3D vision” of connections with neighboring organs. The anterior surface of the stomach is partially adjacent to the diaphragm, the abdominal wall and the lower edge of the liver.
The posterior surface is in contact with the pancreas, aorta, spleen, the upper part of the left kidney with the adrenal gland, and partially with the transverse colon. The dense “neighborhood” is reinforced by nutrition from the same arterial branches, joint venous and lymphatic drainage. Therefore, the structure of the human stomach is subject to changes in pathological conditions of other internal organs.
Where is the stomach?
The stomach is located in the upper half of the abdominal cavity. Approximately ¾ of the organ is located in the left hypochondrium, ¼ in the epigastric region (under the xiphoid process of the sternum)¹.
Inside the human body, the stomach is in close contact with the following organs²:
- diaphragm;
- adrenal;
- spleen;
- colon;
- liver;
- left kidney;
- pancreas.
After eating, the shape of the stomach changes; it is in closer contact with other internal organs, reaching the level of the navel. When emptied, the organ seems to move backwards, without touching the anterior abdominal wall. Relative stability in the abdominal cavity is ensured by a complex of ligaments and low mobility of the inlet/outlet openings².
Why doesn't digestive juice digest the stomach?
Gastric juice, which contains hydrochloric acid, has aggressive chemical properties.
The organ protects itself by continuously producing a thick layer of mucus and other protective factors. Without it, the digestive juices could digest the stomach itself. The strength of the protective factors of the stomach is inhibited by the action of acids, alkalis, alcohol, bacteria (Helicobacter pylori) and medications. The most dangerous in this regard are non-narcotic analgesics (non-steroidal anti-inflammatory drugs - NSAIDs), aspirin and glucocorticosteroids. If you take such medications in high doses for a long time, NSAID gastropathy develops with erosions or ulcers, and the risk of bleeding increases³.
Lower left quadrant
The organs in this quarter are the left kidney, part of the large and small intestine, and in women, the left ovary and fallopian tube.
Abdominal pain in this quarter can be a symptom of colitis, colonic diverticulosis or kidney stones, and in women can also be a sign of ovarian or pelvic inflammation.
Why does your stomach hurt?
Patients cannot always correctly determine which organ hurts them. When contacting a doctor, it is better to talk about the appearance of pain in the upper abdomen (epigastric region). What matters is the time of occurrence of unpleasant sensations, their intensity, connection with food intake and body position.
How does my stomach hurt?
Pain in the stomach can be constant or paroxysmal.
Localized in the upper half of the abdomen under the xiphoid process. Depending on the cause, the sensation may become worse after eating or on an empty stomach. Patients often describe dyspeptic pain as burning or burning. The stomach may hurt for the following reasons³:
- hunger spasm - contraction of the stomach on an empty stomach;
- bad habits (smoking, alcohol abuse, drugs);
- taking medications: nonsteroidal anti-inflammatory drugs (NSAIDs), glucocorticoids, antibiotics, cardiac glycosides, iron supplements, antidepressants.
- injuries, burns, foreign bodies;
- pylorospasm and isolated spasm of the pyloric part, located in the zone of transition of the stomach to the duodenum.
- acute atony - a sharp decrease in the tone of the gastric muscles in a short period of time, which leads to rapid expansion of the organ.
- peptic ulcer and its complications (bleeding, perforation of the stomach wall, pyloroduodenal stenosis, penetration);
- neoplasms - benign tumors or cancer;
- complications of diverticular disease of the stomach - diverticulitis, ulceration of the bottom of the diverticulum, its perforation or torsion of the leg;
- volvulus, prolapse of the stomach
- Ménétrier's disease (tumor-like gastritis) is a rare disease in which giant, rough folds of the mucosa appear with multiple adenomas and cysts.
Stomach ulcers are a common cause of pain.
Image: Crevis / Depositphotos Patients often visit doctors with pain in the upper abdomen, suspecting an exacerbation of chronic gastritis. However, this is a morphological diagnosis, which is made after examining pieces of the stomach (biopsy specimens) under a microscope. If the patient did not undergo gastroscopy with biopsy, then the diagnosis of gastritis is incorrect. Most often, gastritis is generally asymptomatic. What people mistake for its exacerbation is now included in the concept of “functional dyspepsia” (FD). Usually these two diagnoses complement each other.
Stress is no friend to the stomach
Severe stress disrupts gastric motility, leads to changes in the composition of normal microbiota, and worsens the digestion process.
Negative emotions can increase pain, nausea and abdominal discomfort. Therefore, treatment regimens for functional dyspepsia often include antidepressants, and some patients need the help of a psychologist or psychotherapist. Pain in the projection of the stomach does not always indicate its damage. Unpleasant sensations in this place may be caused by diseases of other organs⁴:
- acute pancreatitis and exacerbation of chronic pancreatitis;
- cholelithiasis and biliary tract dysfunction;
- pancreas cancer;
- enterocolitis (inflammation of the intestines), diverticular disease of the colon;
- acute appendicitis: pain initially appears in the epigastrium under the xiphoid process, and after a few hours migrates to the right iliac region (Kocher-Volkovich symptom);
- chronic ischemic disease of the digestive system;
- diseases of the cardiovascular system: angina pectoris, myocardial infarction, pericarditis;
- chest pathology: exudative pleurisy, fractures of the lower ribs;
- viral or bacterial infection;
- depression and other psychiatric spectrum disorders (anorexia, bulimia, anxiety disorder) - can provoke the development of psychogenic pain;
- premenstrual syndrome;
- autoimmune diseases: systemic scleroderma, lupus erythematosus.
Hunger pains
Rarely occurring night pain in the upper abdomen may appear due to a banal spasm due to hunger.
To prevent it, it is enough to adjust your diet and diet without taking long gaps between meals. If hungry night pain in the epigastric region intensifies on an empty stomach, this most likely indicates a peptic ulcer of the stomach and duodenum. It is necessary to consult a gastroenterologist in a timely manner to find the cause of the discomfort and prevent the development of complications.
Colon diverticulosis
Diverticula are projections on the outside of the wall of the colon, commonly called “pockets.” The causes of colonic diverticulosis are not fully known. It is believed that the pathology may be associated with a congenital predisposition and constipation. Diverticulosis itself does not usually cause pain, but it can interfere with bowel movements, make bowel movements difficult, cause air to accumulate in the area, and cause bowel spasms, which can be painful.
Another cause associated with severe pain is inflammation of diverticulitis (diverticulosis). With inflammation, the pain is acute, severe discomfort, bloating, cramps, blood, mucus or pus in the stool may occur, and the temperature may rise. Antibiotics are usually prescribed and surgery is rarely required.
Can a person live without a stomach?
Complete removal of the stomach (gastrectomy) is performed for malignant tumors, severe injuries, and extensive wounds³. After the operation, the person lives on and can even eat naturally.
This becomes possible by creating a special path for the continuous passage of food between the esophagus and intestines. Subsequently, the person is given special treatment and diet to prevent possible complications.
Severely obese patients often undergo surgery to reduce the volume of the stomach (gastrobypass). Surgery has risks (complications and death). The doctor determines the indications during a personal consultation and examination.
After surgery, patients still need to follow a diet and physical activity regimen. Gastric bypass is not a safe alternative to lifestyle changes, but only partially facilitates the process of losing weight.
Gastrointestinal system
This organ is part of the gastrointestinal tract. The general goal of this system is to process food at its entire stage, digestion and absorption of elements necessary for the body. The entire gastrointestinal tract consists of the following sections:
- oral cavity – food is crushed here;
- esophagus - crushed food passes through it to other sections;
- stomach – primary digestion of food occurs here;
- duodenum - here food continues to be digested and transported to the intestines;
- small intestine - a number of chemical elements are absorbed here, which may or may not be needed by the body.
- large intestine - here the necessary components of food are finally absorbed and feces are formed;
- rectum - transports feces directly to the anus.
The system is also equipped with a number of necessary glands: salivary, sublingual, pancreas, etc. Often the liver and gallbladder are part of this same system, although they also have other functions. A diagram of the gastrointestinal tract is shown below (Figure 2).
rice. 2
Prevention of stomach diseases
The following points play a major role in preventing many stomach diseases³:
- Balanced, regular nutrition without strict restrictions and excesses. Food is taken in sufficient portions (individually) without overeating or undereating. It is important to avoid long breaks between meals. The optimal period is 4-5 hours.
- Using an individual set of utensils and keeping the kitchen clean. Control of quality, expiration dates and composition of products.
- Quitting smoking and alcohol.
- Timely detection and adequate treatment of any diseases, including gastrointestinal ones. Compliance with all rules for taking medications, especially those with a negative effect on the gastric mucosa.
- Compliance with safety regulations in industries where occupational hazards are present (coal dust, alkali vapors, acids, lead, paints and varnishes, pharmaceuticals).
- Regular physical activity at moderate intensity. Normalization of body weight.
- Organization of a rational work and rest schedule. Get enough sleep.
- Avoiding stressful situations, if necessary, visiting a psychologist or psychotherapist.
Some diseases are genetic or of unknown origin. Their occurrence is difficult to prevent, but if detected early, they can be controlled with adequate treatment.
A healthy, balanced diet helps prevent stomach diseases. Photo: timolina / Depositphotos
What disease is an enlarged stomach a symptom of?
An enlarged stomach is not only a harbinger of obesity, this indicator can be a symptom of other diseases. Such diseases include:
- Stenosis of the pylorus of the stomach. In which the size of the stomach increases, a sour taste is felt in the mouth, a constant feeling of a full stomach appears, and frequent vomiting.
- Malignant neoplasms in the stomach (cancer). Increased stomach volume, heaviness, blood in the stool, weakness, loss of appetite.
- Hernia in the area of the stomach and esophagus. Pain while eating and while moving.
- Gastric obstruction. Obstruction of food, retention in the stomach, formation of polyps or tumors.
- Hyperplastic gastropathy. During the disease, there is an increase in the folds of the gastric mucosa in size, due to which the stomach becomes larger. Patients experience delayed digestion, a feeling of bloating, pain and heaviness.
- Menetrier's disease. Multiple polyps in the stomach. The stomach is enlarged, frequent pain, weight loss, nausea, diarrhea, bleeding.
If any of these symptoms occur, you should undergo a full examination.
Sources
- Sapin M.R., Bilich G.L. Normal human anatomy: Textbook. In 2 books. Book 1. M.: Medical Information Agency LLC, 2010. - 480 pp.: ill. ISBN 978-5-8948-1814-6
- Agadzhanyan N.A., Smirnov V.M. Normal physiology: A textbook for medical students. M.: LLC Publishing House “Medical Information Agency”, 2009. - 520 pp.: ill. ISBN 978-5-9986-0001-2
- Gastroenterology: Diseases of the stomach - Vakhtangashvili R.Sh., Krzhechkovskaya V.V. 2007. 664 p.
- Trukhan D.I., Tarasova L.V. Pain in the stomach: issues of differential diagnosis // Handbook of outpatient physicians. 2013. No. 2. P. 7–10.
- Kong F, Singh RP. Disintegration of solid foods in human stomach. J Food Sci. 2008 Jun;73(5):R67-80. doi: 10.1111/j.1750-3841.2008.00766.x. PMID: 18577009.
What cells provide the function of digesting food?
The structure of the mucous membrane is studied by histologists when diagnosing a pathological process. Normally it includes:
- cells of single-layer columnar epithelium;
- a layer called “intrinsic”, made of loose connective tissue;
- muscle plate.
The second layer contains its own glands, which have a tubular structure. They are divided into 3 subspecies:
- the main ones - produce pepsinogen and chymosin (digestive enzymes, in an acidic environment they turn into proteolytic enzymes);
- parietal (lining) - synthesize hydrochloric acid and gastromucoprotein;
- additional - form mucus.
Among the glands of the pyloric zone are G-cells that secrete the gastric hormonal substance gastrin. Accessory cells, in addition to mucus, synthesize a substance necessary for the absorption of vitamin B12 and hematopoiesis in the bone marrow (Castle factor). The entire surface of the mucosa in the deep layers contains cells that synthesize the precursor of serotonin.
The gastric glands are located in groups, so under a microscope, from the inside, the mucous membrane has a granular appearance with small pits and flat, irregularly shaped fields. The good adaptability of the healthy mucous membrane is noteworthy. It is capable of rapid recovery: the epithelium on the surface is replaced less than every 2 days, and the glandular one - in 2-3 days. A balance is maintained between old cells being rejected and newly formed ones.
In diseases of the stomach, hypertrophy of the glands, inflammation and cell death occur, dystrophic and atrophic disorders are accompanied by a failure in the production of necessary substances, scarring replaces the functioning tissue with non-functioning fibrocytes. Malignant cells transform into atypical ones. They begin to grow and release toxic substances that poison the body.
The secretory activity of the stomach is controlled by nervous and humoral mechanisms. The main influence on the functioning of the organ is exerted by the branches of the sympathetic and vagus nerves. Sensitivity is provided by the receptor apparatus of the wall and spinal nerves.