Calculous pancreatitis is a disease caused by the accumulation of calcium salts in the pancreas with subsequent formation of stones. The disease occurs in old age and women are more susceptible to it.
The disease is extremely dangerous, and the patient who has been diagnosed with this disease must strictly follow all the doctor’s recommendations, otherwise many complications may develop. The prognosis is usually unfavorable.
Factors such as poor nutrition, frequent antibiotic treatment, alcoholism, gallbladder disease, and viral hepatitis lead to this disease.
Causes
Doctors identify several main risk factors for the incidence of chronic calculous cholecystitis:
- middle and old age;
- pregnancy and childbirth;
- overweight and obesity;
- too sudden loss of body weight;
- starvation;
- total parenteral nutrition;
- family history, heredity;
- taking a number of medications (fibrate derivatives, contraceptive steroids, estrogens during the postmenopausal period, progesterone, octreotide and its analogues, ceftriaxone);
- Crohn's disease, diabetes mellitus, liver cirrhosis, biliary system infections, choledochal and duodenal diverticula.
Symptoms and complications
Pain syndrome. Chronic calculous cholecystitis is characterized by various types of abdominal pain. As a rule, it has a pulling, dull or aching character; in the vast majority of cases, its localization is in the area of the right hypochondrium. 20−30% of patients complain of epigastric pain; in some cases, the pain syndrome is not characterized by a clear localization. The pain radiates to the lumbar region on the right, under the shoulder blade, to the shoulder and the side of the neck.
Hepatic colic. This symptom is a distinctive feature of calculous cholecystitis. This is a sudden onset of acute cramping pain under the right rib. Such cholecystitis often occurs latently, and its first sign is hepatic colic.
Bile intoxication and jaundice. Calculous cholecystitis is characterized by signs of jaundice and intoxication of the patient’s body with bile acids. The sclera, skin, and mucous membranes acquire a yellowish tint. Patients often complain of itchy skin, and upon examination, marks of scratching can be seen on the skin. If the flow of bile is significantly impaired, the urine becomes dark and the feces become discolored. Manifestations of bile intoxication are: low blood pressure, irritability, decreased heart rate, headache, sleep disturbances.
Dyspeptic symptoms. Unstable stools, nausea, belching, metallic or bitter taste, and dry mouth are noted. When the gallbladder suddenly empties, heartburn and vomiting of bile are possible.
The most significant complications of calculous cholecystitis are:
- choledocholithiasis (blockage of the common bile duct with stones);
- stenosis of the papilla of Vater;
- chronic or acute pancreatitis;
- hepatitis, reactive cholangitis;
- subphrenic abscess;
- empyema and perforation of the gallbladder;
- peritonitis.
Chronic pancreatitis: modern approaches to diagnosis and treatment
Serebrova S.Yu.
Today, diseases that occur with a decrease in the enzymatic function of the pancreas and the mucous membrane of the small intestine occupy a significant place in the structure of diseases of the gastrointestinal tract.
Digestion begins in the oral cavity with the grinding of food and partial chemical processing of amylase contained in saliva. Proteins are denatured in the stomach with the participation of hydrochloric acid and undergo hydrolysis there, catalyzed by pepsin. In the duodenum, the food bolus mixes with bile and pancreatic secretions, which leads to the launch of numerous chemical reactions transforming polymers into low molecular weight compounds that can be absorbed. Cavity digestion is carried out mainly with the help of pancreatic enzymes that hydrolyze proteins, fats, and carbohydrates. Nutrients, acting on the chemoreceptors of the duodenum, stimulate the formation of those pancreatic enzymes for which they are substrates. On the other hand, enzymes are selective inhibitors of their own secretion, which underlies duodenopancreatic self-regulation of their formation according to the principle of negative feedback. A decrease in the secretory activity of the pancreas is observed with a decrease in the M-cholinergic and peptidergic (secretin and cholecystokinin) stimulating effect on it and with the activation of the adrenergic inhibitory mechanism. Endogenous factors that increase the amount of secreted pancreatic enzymes are cholecystokinin, gastrin, bombesin, substance P, secretin, vasoactive intestinal polypeptide, histamine, nitric oxide. The secretion of enzymes is inhibited by somatostatin, glucagon, pancreatic polypeptide, gastric inhibitory peptide, enkephalins, calcitonin, peptide Y, peptide YY, norepinephrine. Acidification of the contents of the duodenum (decompensation of alkalization in the antrum of the stomach during duodenal ulcer) leads to stimulation of the formation of secretin with an increase in the production of bicarbonates by the pancreas. Bicarbonates of pancreatic origin, in turn, neutralize hydrochloric acid residues and provide the pH level necessary for the activation of pancreatic enzymes [4,9,11].
Pancreatic enzymes are secreted into the lumen of the duodenum in an active state or in the form of proenzymes. α-amylase (breaks down the polysaccharides starch and glycogen to maltose and maltotriose) and lipase (breaks down triglycerides to mono-, diglycerides and fatty acids) are secreted in active form. In this case, lipid metabolism depends on the size of fat droplets that undergo emulsification with the participation of bile acids. Proteolytic enzymes are secreted in the form of proenzymes, and their activation occurs in the lumen of the small intestine at a certain pH level with the participation of enteric enzymes (enterokinase) or due to mutual catalytic effects. If there is insufficient production of bicarbonate by the pancreas, when the pH does not rise to the level necessary to activate proteolytic enzymes, protein breakdown will be less efficient. At a pH of approximately 6, with the participation of enterokinase, trypsinogen is converted into active trypsin, which, in turn, activates the proenzymes chemotrypsin, elastase and carboxypeptidase A and B. Trypsin breaks down protein molecules mainly in the zone of arginine and lysine, chemotrypsin - in the zones of aromatic amino acids , leucine, glutamine, methionine. Elastin (a connective tissue protein) is destroyed only by elastase. Carboxypeptidase A and B cleave the outer bonds of proteins. Hydrolysis of proteins by pancreatic enzymes leads to the formation of low molecular weight peptides and glucose. The final stage of oligopeptide cleavage and amino acid transport occurs on the villi of the apical surface of enterocytes with the participation of intestinal and adsorbed pancreatic peptidases. When pancreatic enzymes move to the terminal parts of the small intestine, their activity decreases, but proteases and amylase are more stable than lipase, which is inactivated when the pH of the chyme decreases and under the influence of the same proteases. In conditions of exocrine pancreatic insufficiency, lipase deficiency is even more noticeable. This explains the fact that impaired digestion of fats develops earlier than starch and proteins [4,10,12].
The causes of abdominal digestion disorders can be different. Hydrolysis of fats can decrease with a deficiency of bile acids (congenital pathology, obstructive jaundice, primary biliary cirrhosis, severe parenchymal liver pathology, disturbances in the enterohepatic circulation of bile acids). But the most common and significant cause of disorders of luminal hydrolysis are diseases of the pancreas, leading to a deficiency of its functioning tissue and exocrine insufficiency: chronic pancreatitis, subtotal or total pancreatectomy, pancreatic cancer, cystic fibrosis, decreased enterokinase activity (Zollinger-Ellison syndrome, pancreozymin deficiency and secretin).
The term chronic pancreatitis denotes a group of chronic diseases of the pancreas of various etiologies, predominantly inflammatory in nature, with phase-progressive focal, segmental or diffuse degenerative or destructive changes in its exocrine tissue, atrophy of glandular elements (pancreocytes) and their replacement with connective (fibrous) tissue, changes in ductal system of the pancreas with the formation of cysts and calculi, with varying degrees of disruption of exocrine and endocrine functions [4,6].
Over the past thirty years, there has been a more than twofold increase in the number of chronic and acute pancreatitis. It is difficult to name the true incidence figures, and the frequency of chronic pancreatitis among the population of different countries varies from 0.2 to 0.68%. The disease is diagnosed in 6-8% of gastroenterological patients. In developed countries, chronic pancreatitis has become noticeably “younger”: the average age of patients diagnosed with this disease has decreased from 50 to 39 years, and the proportion of women among patients has increased by 30%. There are 8.2 new cases per 100,000 population per year. The prevalence of chronic pancreatitis according to autopsy data ranges from 0.01 to 5.4%, on average - 0.3-0.4%. The incidence of pathology is constantly increasing due to alcohol consumption and improved diagnostic methods; the proportion of alcoholic pancreatitis increased from 40 to 75%. There is also an increase in the incidence of pancreatic carcinoma, which develops against the background of chronic pancreatitis. In Russia, an even more dramatic increase in incidence is observed: for example, the prevalence of chronic pancreatitis among children is 9-25 cases, and among adults - 27-50 cases per 100,000 population [5,8,11].
Chronic pancreatitis is a polyetiological disease. The main causes of primary pathology are alcohol, heredity, errors in diet (protein deficiency in the diet, abundant intake of fatty and protein foods against the background of chronic alcohol intake), the use of certain drugs (azathioprine, 6-mercaptopurine, hydrochlorothiazide, methyldopa, sulfonamides (sulfasalazine), tetracyclines, glucocorticoids, estrogens, etc.), chronic pancreatic ischemia, autoimmune diseases [3,6]. The causes of secondary chronic pancreatitis (obstructive, biliary-dependent, cholepancreatitis) are cholelithiasis, anomalies in the development of the common bile duct, postcholecystectomy syndrome, adhesive disease, helminthic infestations (parasitic chronic pancreatitis), chronic hepatitis and cirrhosis of the liver (hepatopancreatic syndrome), primary and secondary sclerosing cholangitis ( sclerosis of the terminal part of the common bile duct), hemochromatosis (“bronze diabetes”: cirrhosis, chronic pancreatitis, diabetes mellitus), mumps, hyperparathyroidism (impaired calcium and phosphorus metabolism, calcifications in the pancreas), papillitis (odditis), papillostenosis, papillary diverticulum duodenum, Crohn's disease, etc. Diseases in which there is an increase in pressure in the duodenum (peptic ulcer, arteriomesenteric compression) can lead to reflux of luminal contents into the pancreatic duct and the development of chronic pancreatitis [2,3,9,14]. Risk factors include hyperlipidemia, hypercalcemia, diabetes mellitus, smoking, drinking coffee, nitrates and nitrites used in agriculture, some industrial agents and chemicals, salts of heavy metals (strontium, zinc, lead) [3].
Speaking about the pathogenesis of chronic pancreatitis, it is noted that in a significant proportion of patients the leading factor is an increase in pressure in the ductal system with activation of enzymes in the pancreas and autolysis. The entry of activated enzymes into the blood leads to destructive changes in other organs and tissues: kidneys, lungs, central nervous system, fatty tissue, etc. A common cause of progression of chronic pancreatitis is the deposition of protein precipitates in small ducts. With the viral etiology of pancreatitis, the most significant pathophysiological phenomenon is not autolysis, but the progression of fibrosis due to cell degeneration and acceleration of apoptosis. In all forms and variants of the pathogenesis of chronic pancreatitis, changes in the microcirculation system play a significant role, leading to hypoxia of gland cells and an increase in the level of cAMP in them, which, in turn, promotes the activation of Ca2+ transport into the cells. As a result, cells are oversaturated with calcium, excessively accumulated in mitochondria, and this leads to the decoupling of oxidation and phosphorylation. Next comes deenergization of cells and an increase in the processes of dystrophy [6,15].
Chronic pancreatitis is morphologically characterized by irregular sclerosis, destruction and irreparable loss of pancreatic parenchyma, which can be focal, segmented or diffuse (most patients have calcification). Obstructive chronic pancreatitis is a separate nosological form, characterized by a general expansion of the ductal system proximal to the site of occlusion.
More than 40 classification options for chronic pancreatitis are known. In 1983, at the II International Symposium in Marseille, it was decided to distinguish two forms of the disease:
I. Chronic pancreatitis with focal necrosis, segmental or diffuse fibrosis with (or without):
- calcifications;
- expansion and deformation of the ductal system of the gland;
- inflammatory infiltration, cyst formation.
II. Chronic obstructive pancreatitis, which is characterized by expansion and (or) deformation of the ductal system, parenchymal atrophy, diffuse fibrosis proximal to the site of duct occlusion.
Depending on the clinical symptoms, it is proposed to distinguish the following forms of chronic pancreatitis:
- latent (subclinical), when morphological changes are detected in the pancreas; organ dysfunction is observed, but there are no clear clinical symptoms of the disease;
- painful chronic pancreatitis, characterized by the presence of periodic or constant abdominal pain;
- painless chronic pancreatitis occurring with exo- and (or) endocrine pancreatic insufficiency with or without complications.
With all its undoubted advantages, the Marseille classification of 1983 is not always applicable in wide clinical practice: it is possible to classify the form of the disease only on the basis of histological examination of pancreatic biopsies obtained during laparotomy or endoscopic retrograde pancreatic cholangiography.
The Marseille-Roman classification (1988) is a modification of the Marseille (1983) classification and includes three main types of chronic pancreatitis:
I. Chronic calcific pancreatitis (presence of pancreatic calcifications or the possibility of their development in the future). The most common cause of this form of the disease is alcohol. As a result of inflammation and changes in the structure of the smallest pancreatic ducts, the secretion thickens with the formation of plugs rich in protein and calcium. In this process, an important role is played by reducing the concentration of lithostatin (a protein that prevents stone formation).
II. Chronic obstructive pancreatitis (observed with severe narrowing of the main pancreatic duct or its large branches, or the nipple of Vater). Causes of development: alcohol, cholelithiasis, trauma, tumor, birth defects. Rarely seen.
III. Chronic parenchymal fibrous (inflammatory) pancreatitis is also a relatively rare form.
In 1990, Ivashkin V.T. et al. proposed a classification of chronic pancreatitis
- According to morphological characteristics:
interstitial-edematous;
- parenchymal;
- fibrous-sclerotic (indurative);
- hyperplastic (pseudotumorous);
- cystic.
- painful;
- rarely recurrent;
- biliary dependent;
- disturbances in the outflow of bile;
When describing the clinical manifestations of chronic pancreatitis, several syndromes are distinguished.
Exocrine insufficiency syndrome is manifested by weight loss and dyspeptic disorders. The consequence of lipase deficiency is an increase in stool frequency up to 2-4 or more times a day, bloating, excessive gas formation, polyfecal matter, and steatorrhea. With severe lipase deficiency, patients note a kind of “pancreatic stool” - large in volume, foul-smelling, grayish in color. The surface of the stool may be covered with a thin film of fat, which gives it a peculiar “shiny” character. The absorption of fat-soluble vitamins is impaired. Trophic disorders (dry skin, dullness and brittleness of nails and hair, cracks in the corners of the lips, tongue, etc.) with the syndrome of impaired cavity digestion are rare.
Inflammatory-destructive syndrome. Inflammation, sclerosis and cyst formation can be accompanied by compression of the common bile duct, the development of jaundice with acholia, and skin itching. Jaundice appears or increases more often after a painful attack and is recurrent in nature. Hyperbilirubinemia is observed in 1/3 of patients. In chronic pancreatitis, the phenomenon of enzyme “evasion” may be observed, i.e. their increased entry into the blood, which is caused either by a violation of the integrity of the gland parenchyma, or by ductal hypertension.
The pain syndrome is usually explained by a violation of the outflow of pancreatic juice and ductal hypertension, as well as with the involvement of the parietal peritoneum in the chronic inflammatory process, cicatricial changes in the parapancreatic tissue and adjacent organs. The pain is usually constant, often painful, aggravated by eating fatty, spicy foods, localized in the epigastric region, and sometimes girdling. Irradiation depends on the localization of the inflammatory-degenerative process in the pancreas: when the head of the pancreas is affected, the pain radiates to the right hypochondrium, the body to the epigastric region, and the tail to the left hypochondrium. In approximately 10% of patients, pain irradiates to the heart area. There is a dependence of the pain syndrome on the nature of the food: in alcoholic chronic pancreatitis, which often occurs against the background of pronounced stimulation of external secretion, pain often occurs after eating spicy and sour foods; with cholangiogenic pancreatitis, pain appears after eating fatty foods.
Endocrine deficiency syndrome: frequent development of hypoglycemic conditions due to low levels of glucagon in the blood serum or hyperglycemia, especially at the height of the inflammatory-destructive syndrome. It manifests itself as attacks of “ravenous hunger” and signs of diabetes mellitus with less need for insulin. A “pseudopancreatic triad” develops: hyperglycemia, dry mouth and thirst without ketoacidosis.
Astheno-vegetative syndrome - weakness, irritability, especially on an empty stomach, sleep disturbance, decreased performance.
Dyspeptic syndrome is manifested by changes in appetite (to the point of anorexia), nausea, vomiting that does not bring relief, aversion to fatty foods, salivation, flatulence, bloating, diarrhea (sometimes alternating with constipation).
Dyskinetic syndrome - diarrhea, sometimes constipation (due to low intake of fats and fiber, intestinal atony) [3,4,13].
Chronic pancreatitis can be complicated by diabetes mellitus, intestinal dysbiosis, nonspecific reactive hepatitis, pseudocysts, pancreatic cancer, hypovolemic shock (associated with the entry into the blood of vasoactive kallikrein and kinin with increased vascular permeability and leakage of plasma into the intercellular space, a decrease in circulating blood volume), development gastrointestinal bleeding (due to thrombosis of the splenic vein), stenosis of the distal common bile duct (due to edema of the head of the pancreas, less often the cause of its development are pseudocysts), stenosis of the duodenal bulb, abscesses of the pancreas and adjacent tissues, pancreatic ascites (due to rupture of pancreatic ducts with increased pressure in them), peritonitis, fistulas and stenosis of the colon, reactive pleurisy, pneumonia, fistula formation, arteriopathy of the lower extremities, anemia, encephalopathy, splenomegaly (rarely), hepatomegaly (due to the development of fatty degeneration), etc. . [3,5,6].
Laboratory diagnostics. In most patients with chronic pancreatitis, a general blood test, both during the period of remission and at the time of exacerbation of the disease, turns out to be unchanged. Determination of α-amylase remains important in recognizing exacerbations of chronic pancreatitis. The main methods used to diagnose exocrine pancreatic insufficiency are coprological examination, direct tests of exocrine function (secretin-pancreozymin or secretin-cerulein, LUNDT test and its modifications), indirect tests of exocrine function that do not require duodenal intubation (PABK test or bentyramine test, serum immunoreactive trypsin test, fecal elastase-1 test).
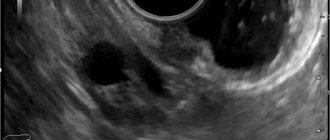
Modern methods of instrumental diagnostics make it possible to determine changes in the size of the pancreas, uneven contour, decrease and increase in its echogenicity, pseudocysts (ultrasound, CTG), signs of enlargement of the head (hypotonic duodenography), calcifications, duodenal dyskinesia or duodenostasis (radiography), various changes in the ductal system (cholecystocholangiography, ECPGR, Wirsungography) and in the vascular system of the pancreas (selective angiography) [3,5].
The main way to compensate for exocrine pancreatic insufficiency is enzyme replacement therapy. Chronic pancreatitis is one of the indications for prescribing Mezim® forte 10000, a drug with amylase enzymatic activity of 7500 Ph units. Eur, lipase 10000 units Ph. Eur and proteases 375 units Ph. Eur. The first pancreatin-containing drugs were characterized by low clinical effectiveness, which was associated with their rapid inactivation by gastric hydrochloric acid. Mezim® forte 10000 is available in the form of enteric-coated tablets. Since pancreatic lipase is most susceptible to acid-dependent destruction, the absorption of fats and fat-soluble compounds will depend entirely on the quality of the enteric coating. Therefore, the greatest clinical effectiveness should be expected from a well-proven drug produced by a well-known manufacturer [17]. For earlier activation of proteolytic enzymes and their contact with the epithelium of the proximal small intestine, the combined use of enzyme preparations with inhibitors of gastric acid production is recommended [4]. The patient should be warned that Mezim® forte 10000 tablets should be swallowed without chewing, so as not to damage the enteric coating. Also, the drug should not be used simultaneously with liquid products whose pH is greater than 5.5 (for example, milk), as this leads to premature destruction of its shell.
The dose of pancreatic enzymes is selected taking into account the severity of the disease, depending on the age of the patient and a number of other individual factors, the quantitative and qualitative composition of the drug used. It should be especially noted that the dosage of proteolytic enzymes should be extremely careful, since when using high doses of these enzymes, the development of iatrogenic fibrosing colitis is possible. When treated with drugs containing pancreatic enzymes, allergic reactions, skin irritation in the perianal area and oral mucosa are also possible, and the use of high doses of enzymes can lead to the appearance of hyperuricuria, which promotes the precipitation of uric acid in the tubular apparatus of the kidney, creating conditions for the development of urolithiasis [16,18,20]. Indicators of the effectiveness of replacement therapy are improvement in the patient’s subjective sensations and the absence of neutral fat in the feces.
The studies demonstrated that in patients with a moderate decrease in the exocrine pancreatic secretion in chronic pancreatitis, MezimO forte 10000 effectively corrected the clinical and laboratory manifestations of insufficiency of the exocrine function of the organ. It was concluded that, taking into account the positive effect of the drug on reducing the severity of pain, it can be used for monotherapy in people suffering from a painful form of chronic pancreatitis with moderate impairment of the exocrine function of the pancreas [13].
The reasons for the ineffectiveness of replacement therapy may be an incorrect diagnosis, steatorrhea of extrapancreatic origin (giardiasis, celiac disease, excessive microbial contamination of the small intestine), violation of the drug regimen (reduced frequency, taking asynchronously with food), insufficient amount of enzyme taken, loss of drug activity due to its long-term or improper storage, inactivation of the enzyme in the acidic contents of the stomach.
Thus, MezimO forte 10000, with an adequate choice of dosage regimen, taking into account the individual characteristics of the patient, and maintaining the integrity of the enteric membrane, is an effective, safe and affordable means of correcting exocrine insufficiency in chronic pancreatitis.
Literature 1. Belousova E.A., Nikitina N.V., Mishurovskaya T.S., Tsodikov G.V. Abdominal pain syndrome in chronic pancreatitis // Farmateka. - 2007. - pp. 29-34. 2. Vasiliev Yu.V. Dysfunction of the sphincter of Oddi as one of the factors in the development of chronic pancreatitis: treatment of patients // Journal “Difficult Patient”. - 2007. No. 5. 3. Diseases of the pancreas. https://www.therapy-handbook.medexplorer.ru/panc.php 4. Kalinin A.V. Disorders of cavity digestion and its drug correction // Clinical perspectives in gastroenterology and hepatology. - 2001. - N 3. — P. 21-25. 5. Kalinin A.V., Khazanov A.I., Sesivtsev V.N. Chronic pancreatitis: etiology, treatment and prevention. Guidelines. State Institute for Advanced Training of Doctors of the Ministry of Defense of the Russian Federation, Department of Gastroenterology, Moscow, 1999 6. Minushkin O.N. Chronic pancreatitis: some aspects of pathogenesis, diagnosis and treatment // CONSILIUM MEDICUM. - 2002. - Volume 4. - No. 1. 7. Minushkin O.N. Chronic pancreatitis: epidemiology, etiology, classification // Farmateka. - 2007. - No. 2. — P. 53-56. 8. Okhlobystin A.V., Buklis E.R. Modern possibilities for the treatment of chronic pancreatitis // Attending physician: Journal for a practicing physician. - 2003. - No. 5. - P. 32-36. 9. Paltsev A.I. Pain syndrome in the clinic of chronic pancreatitis // Medical interdisciplinary scientific and practical journal “PAIN and its treatment” -. - 2000. - No. 12. - https://www.painstudy.ru/matls/pabdo/xronich_pankreatit.htm 10. Parfenov A.I. Contribution of A.M. Ugolev in the development of enterology // Russian Journal of Gastroenterol., Hepatol., Coloproctol. - 1993. - No. 3. — P.6-12. 11. Samsonov A.A. Modern pharmacotherapy of chronic pancreatitis // Russian pharmacies. - 2007. - No. 3 - P.30-32. 12. Ugolev A.M. Physiology and pathology of parietal (contact) digestion. - L., 1967. - 216 p. 13. Shifrin O.S. Enzyme preparations in the treatment of exocrine pancreatic insufficiency // CONSILIUM MEDICUM. - 2007. - Volume 9. - No. 1. 14. Shishkin I.M. Diagnosis and surgical treatment of chronic calculous cholecystitis and chronic pancreatitis with arteriomesenteric compression of the duodenum // Abstract of thesis. diss. ...cand. honey. Sci. - Perm, 2001. - 46 p. 15. Yakovenko A.V., Yakovenko E.P. Chronic pancreatitis. Practical approaches to therapy // Digestive diseases (for specialists and general practitioners): BC library. - 2007. - Volume 9. - No. 2. — P. 48-51. 16. Drug Facts and Comparisons. Digestive enzymes product list. Available at: https://online.factsandcomparisons.com/printsection.aspx?id-7696§ion=prodlist. Accessed March 29, 2006. 17. Hendeles L., Dorf A., Stecenko A., Weinberger M. Treatment failures after substitution of generic pancrelipase capsules: correlation with in vitro lipase activity // JAMA. - 1990. - Vol.26. — P.29-61. 18. Lee J., Ip W., Durie P. Is fibrosing colonopathy an immune mediated disease? //Arch. Dis. Child. - 1997. - Vol.77. - No. 1. — P.66-70. 19. Nair RJ, Lawler L., Miller MR Chronic Pancreatitis // Am Fam Physician. - 2007. - Vol. 76. - No. 11. - R.1679-1688. 20. Schibli S., Durie PR Tullis ED Proper usage of pancreatic enzymes // Curr. Opin. Pulm. Med. - 2002. - Vol.8. — No. 6. — P. 542-546.
Diagnostics
Diagnosis of cholelithiasis is based on the clinical picture, as well as data obtained during an instrumental examination. To make a diagnosis with sufficient accuracy, it is enough to perform an ultrasound of the upper abdominal cavity. With its help, you can identify stones in the ducts, gall bladder, determine the size of the bladder, its walls, the condition of the pancreas and liver. Gastroduodenoscopy is also performed to determine the condition of the mucous membrane of the stomach, esophagus and duodenum. If there are complications, retrograde cholangiography or transgastric ultrasound of the bile ducts is prescribed to detect choledocholithiasis.
Peculiarities
Pancreatitis with stones of various etiologies has its own characteristics.
Most often, inflammation of the gland is diagnosed in combination with cholelithiasis.
Calculous pancreatitis and cholecystitis
Women are more likely to suffer from calculous cholecystitis and pancreatitis. Stones are cholesterol (detected in 80% of cases) and pigment.
Women are more likely to suffer from calculous cholecystitis and pancreatitis.
When pancreatitis is combined with cholecystitis, biliary colic often occurs. This is an acute pain syndrome. The attack most often occurs at night. The pain intensifies when inhaling and lying on the left side. Worried about repeated vomiting and general malaise. This condition requires emergency care.
Treatment
Non-surgical treatment. It is based on diet and medication. Patients with calculous cholecystitis refuse foods that lead to excessive secretion of bile and cause an exacerbation of the disease. Alcohol and carbonated water are completely excluded. The doctor prescribes hepatoprotectors, antispasmodics, enzymes, herbal medicines, antibiotics (if there is an infection). Treatment of chronic calculous cholecystitis is possible with small stones (up to 15 mm), consisting of cholesterol, and normal motor activity of the gallbladder.
Surgical treatment. Treatment is often carried out surgically. As a rule, the entire gallbladder is removed along with the stones. Depending on the indications, access can be carried out either laparoscopically or laparotomically. The operations are performed under general anesthesia.
To make an appointment at the ABC-Medicine clinic to clarify symptoms and treat chronic cholecystitis, call +7.