Gastroesophageal reflux disease (GERD)
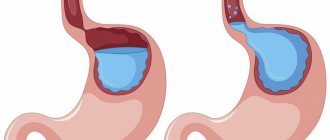
is a disease caused by repeated spontaneous reflux of stomach contents (and in some cases, duodenum) into the esophagus.
Our body is designed in such a way that movement must occur in only one direction: food from the esophagus must enter the stomach.
The reverse movement is prevented by a ring of muscle, the lower esophageal sphincter, which provides a barrier that prevents stomach contents from naturally flowing into the esophagus. The digestive process begins in the stomach. Gastric juice secreted to digest food contains aggressive hydrochloric acid. Once in the esophagus, where it is not intended to be located, the acid causes irritation of the mucous membrane, manifested as a burning sensation along the esophagus, which we call heartburn. Heartburn can occur even in a healthy person, but if reflux occurs quite often, irritation of the esophageal mucosa can cause inflammation.
Thus, isolated cases of heartburn are not a disease, but if irritation of the esophageal mucosa occurs often enough, GERD is diagnosed. In this case, endoscopic examination may not reveal mucosal erosion. This form of the disease is called endoscopically negative reflux disease.
.
It accounts for approximately 70% of cases. In 30% of cases, endoscopy reveals mucosal lesions. This form of the disease is called reflux esophagitis
.
Causes of GERD
Reflux (reflux of stomach contents into the esophagus) can occur for the following reasons:
decreased tone of the lower esophageal sphincter.
Sphincter weakness may result from:- consumption of caffeinated drinks, chocolate;
- smoking;
- alcohol abuse;
- hormonal changes during pregnancy;
taking certain medications;
- flatulence (which, in turn, can be a consequence of poor nutrition, gastrointestinal diseases, digestive disorders - dyspepsia);
pregnancy;
- hiatal hernia.
For the development of gastroesophageal reflux disease, not only the reflux itself is important, but also some other factors that contribute to the aggravation of the situation, for example:
- depressed state of the esophageal mucosa, in which it is unable to resist damage;
- impaired ability of the esophagus to cleanse itself. Normally, the esophagus should quickly be cleared of the stomach contents that have entered it - due to gravity and peristalsis, and the acidity of the environment should be eliminated by sodium bicarbonate, which is part of the saliva.
Factors that provoke reflux are:
- stress;
- eating too much food (overeating);
- eating foods that cause increased gas formation and other digestive disorders;
- physical activity after meals.
Prokinetics
These drugs restore the normal physiological state of the esophagus by increasing the tone of the lower sphincter, improving clearance and enhancing peristalsis. The main means of pathogenetic therapy for GERD is the prokinetic drug Motilium. It normalizes the motor activity of the upper digestive tract, restores active gastric motility and improves antroduodenal coordination. Motilium is well tolerated when long-term therapy is necessary and reduces the percentage of disease relapses.
Symptoms of GERD
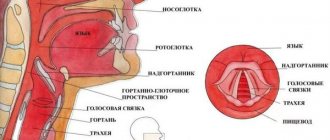
Acid from the stomach can enter the respiratory tract (this usually happens when lying down) and cause a sore throat, hoarseness, dry mouth, and cough. GERD can stimulate the development of bronchial asthma, chronic obstructive bronchitis, and aspiration pneumonia.
The constant presence of acidic contents in the esophagus leads to scarring of the mucous membrane of the lower part of the esophagus, as a result of which the lumen of the esophagus narrows (this complication of GERD is called peptic stricture of the esophagus). In this case, pain when swallowing and dysphagia (difficulty swallowing) may occur.
But first of all, GERD is characterized by symptoms that usually appear an hour and a half after eating. This:
Heartburn
Heartburn is the main symptom of GERD. The presence of heartburn that regularly occurs after eating is the basis for diagnosing the disease.
More about the symptom
Belching
With GERD, belching after eating is typical.
More about the symptom
Sour or bitter taste in the mouth
A sour taste in the mouth means that acid from the stomach has traveled up the esophagus and irritated the taste buds. The taste in the mouth may be bitter if bile enters the esophagus, which normally should not rise above the duodenum.
Chest pain
A burning sensation may be felt behind the sternum (along the esophagus). Often the complaint is formulated as chest pain, so it is important to make sure that the pain is caused by irritation of the esophageal mucosa, and not by heart problems. In the case of GERD, the pain is usually associated with food intake, begins in the epigastric region and only then rises higher. Pain can radiate to the neck, shoulders, interscapular area, and lower jaw.
Proton pump inhibitors
If GERD with esophagitis is diagnosed, treatment with prokinetics is carried out in combination with proton pump inhibitors. As a rule, the new generation drug “Pariet” is used. Due to its use, acid secretion is reduced, and there is a positive dynamics in the clinical manifestations of the disease. Patients report a decrease in the intensity or even complete disappearance of heartburn, and a decrease in pain. For GERD, the treatment regimen with prokinetics and proton pump inhibitors is as follows: 20 milligrams of the drug “Pariet” and 40 milligrams of the drug “Motilium” are prescribed per day.
GERD Treatment Methods
Treatment of GERD is carried out by a gastroenterologist. Treatment is aimed at relieving inflammation of the esophageal mucosa, reducing the frequency of reflux of stomach contents into the esophagus, reducing the damaging properties of refluxate (the substance that enters the esophagus from the stomach), and increasing the protective properties of the esophageal mucosa.
Of great importance is:
Drug treatment
Treatment with medications is prescribed by a doctor and must take into account the individual characteristics of the patient.
Lifestyle change
Normalization of lifestyle is of great importance. It is necessary to quit smoking, limit, or better yet eliminate, alcohol consumption. You should not eat fatty, spicy, sour foods, as well as coffee, tea, chocolate, legumes, cabbage, peas, and brown bread. It is better to take food more often (4-6 times a day), but in small portions. You should not eat before bed (the last meal should be 2-2.5 hours before bedtime). You should sleep with your upper body elevated to reduce the likelihood of reflux during sleep.
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Recommendations for diet and regimen
Regardless of the stage and severity of GERD, treatment involves constant adherence to certain rules:
- Do not lie down or lean forward after eating.
- Do not wear tight clothes, corsets, tight belts, bandages - this leads to an increase in intra-abdominal pressure.
- Sleep on a bed in which the part where the head is located is raised.
- Do not eat at night, avoid large meals, do not eat too hot food.
- Quit alcohol and smoking.
- Limit consumption of fats, chocolate, coffee and citrus fruits, as they are irritating and reduce LES pressure.
- Lose weight if you are obese.
- Stop taking medications that cause reflux. These include antispasmodics, β-blockers, prostaglandins, anticholinergic drugs, tranquilizers, nitrates, sedatives, calcium channel inhibitors.
Surgical intervention
Sometimes, to restore normal function of the cardia, it is necessary to resort to surgery aimed at eliminating reflux. Indications for surgical treatment are as follows:
- complications of GERD (repeated bleeding, strictures);
- ineffectiveness of conservative therapy;
- frequent aspiration pneumonia;
- diagnosing Barrett's syndrome with high-grade dysplasia;
- the need of young patients with GERD for long-term antireflux therapy.
Reflux is often treated by fundoplication. However, this method is not without drawbacks. Thus, the result of the operation entirely depends on the experience of the surgeon; sometimes after surgery there remains a need for drug treatment, there is a risk of death. Currently, various endoscopic techniques have been used to influence foci of metaplasia: electrocoagulation, laser destruction, photodynamic destruction, argon plasma coagulation, endoscopic local resection of the esophageal mucosa.
Advantages of laparoscopic surgery
- Less traumatic and no pain in the postoperative period;
- Short period of hospitalization - no more than three days;
- Rapid recovery - after two weeks, patients return to their normal lifestyle.
Since patients often have other diseases that require surgical treatment, so-called simultaneous operations can be performed using laparoscopic access. I have been performing similar interventions for more than two decades. When performing a simultaneous operation during one anesthesia, you can immediately get rid of 2-5 surgical pathologies (for example, calculous cholecystitis, cholelithiasis, tumors, cysts, etc.).
Many, even experiencing painful attacks of heartburn, are in no hurry to see a doctor, trying to alleviate the condition in various ways, including with the help of medications. Is it necessary to treat reflux esophagitis if the symptoms are eliminated with the help of drugs that can be bought at any pharmacy? Of course, since there is a risk of developing severe complications. In addition, in the absence of adequate treatment, you will have to take medications throughout your life and adhere to strict dietary restrictions. At the same time, the effect of the drugs is very short-lived, and any physical activity immediately causes unpleasant and even painful sensations. To determine the extent of the disease and choose the most appropriate treatment tactics, just contact me by email or by scheduling a consultation.
Carrying out surgical interventions for diseases of the esophagus and stomach requires excellent command of surgical techniques, including endoscopic suture, which is impossible without appropriate experience. Over more than 25 years of experience, I have performed more than 2000 surgical interventions for reflux esophagitis, GERD and hiatal hernia. I am the author of monographs and more than 50 scientific papers devoted to these problems. I also regularly conduct seminars and master classes on these diseases, which are attended by specialists from various clinics and centers.
Therapy for young children
In babies, reflux causes frequent burping. Treatment consists of several stages:
- Postural therapy. You need to feed the baby in a sitting position, holding him at an angle of 45-60 degrees. At the end of feeding, this position must be maintained for another twenty to thirty minutes, after which the baby can be placed on his back, with his head elevated at an angle of 30 degrees.
- Dietary correction. It is recommended to reduce the child’s daily feeding volume, while increasing the total number of feedings. If breastfeeding is carried out, the mother should take breast milk thickeners. Formulas containing gum, such as Nutrilon AR, Nutrilak AR, Humana AR, or rice starch, such as Enfamil AR, are recommended for bottle-fed infants.
- Treatment of GERD in young children is also not complete without taking prokinetic drugs (Motilium, Motilak, Cerucal), antacids (Phosphalugel) and antisecretory drugs (Losec). The dosage should be selected only by a specialist.
Classification of reflux esophagitis
The two most widespread classifications of esophagitis in the world are the Savary-Miller classification, adopted in 1977 and modified in 1997 at the 6th European Gastroenterological Conference, and the Los Angeles classification, also adopted in 1997. It is considered more complete and therefore more often used.
Savary-Miller classification
1st degree - one or more erosions occupying less than 10% of the circumference of the esophagus 2nd degree - merging erosions occupying more than 10, but less than 50% of the circumference of the esophagus 3rd degree - multiple erosions occupying the entire circumference of the lower third of the esophagus 4th degree - complications of reflux esophagitis: esophageal ulcer, stricture, Barrett's esophagus
Los Angeles classification of esophagitis
Grade A - damage to the wall no more than 5 cm long, within one fold of the mucosa Grade B - damage more than 5 cm long, but within one fold Grade C - damage more than 5 cm long, occupying up to 75% of the circumference of the esophagus Grade D - damage to the mucosa occupying 75% or more of the circumference of the esophagus
Let's summarize:
Diagnosis of laryngopharyngeal reflux is not easy; it cannot be solved 100% by the methods familiar to a gastroenterologist; the efforts of other specialists are required to exclude other conditions with similar complaints.
Each case is discussed individually with patients or their families.
Often the solution may be to evaluate the effect of a trial treatment (more on therapy later...)
Treatment of laryngopharyngeal reflux
27, total, today
Diagnostics
First of all, the doctor analyzes the patient’s complaints. Then he sends him for a general blood and urine test.
To clarify the diagnosis, the following diagnostic methods are used:
- Ultrasound of the abdominal organs;
- Radiography;
- Stomach acidity test;
- Esophagogastroduodenoscopy;
- Impedance measurement of the esophagus;
- CT scan;
- Manometry;
- Scintigraphy;
- Billimetry;
- Breath test for Helicobacter pylori.
In some cases, a histological examination of a biopsy of the esophageal mucosa is required. It is obtained using a targeted biopsy.
If a patient has esophagitis, diagnosis and treatment of the pathology in Moscow can cost him an average of 10,500-50,000, depending on diagnostic methods and type of treatment.
Therapy with folk remedies
In the initial stages of GERD, alternative treatment can be very helpful. In general, at these stages you can cope with the disease simply by following an antireflux regimen and changing your lifestyle. If the disease is mild, instead of antacids to relieve heartburn, you can use various traditional medicines that strengthen and protect the esophageal mucosa, improve sphincter tone and reduce the acidity of gastric juice. In severe cases of the pathological process, it will not be possible to do without drug therapy, and in the presence of complications, surgical intervention is generally required. Therefore, treatment of GERD with folk remedies is rather an auxiliary and preventive method. It can be used as a complement to highly effective drug therapy regimens. Herbal medicine is very popular among people. Here are several traditional medicine recipes for the treatment of reflux disease.
- combine crushed dry herb yarrow (20 grams), St. John's wort (20 grams), celandine (10 grams) and chamomile (20 grams). Pour a tablespoon of the mixture into a glass of boiling water and leave for fifteen minutes. Take the strained solution one to two glasses per day;
- mix calendula flowers (20 grams), chamomile flowers (5 grams), coltsfoot leaves (20 grams). Pour two tablespoons of the mixture into a glass of boiling water and leave for thirty minutes. Take the strained infusion before meals (twenty minutes before) one tablespoon three or four times a day;
- combine St. John's wort herb (20 grams), chamomile flowers (5 grams), plantain leaves (20 grams). Pour two tablespoons of the mixture into a glass of boiling water and leave for thirty minutes. Take the strained decoction before meals (twenty minutes before) one tablespoon three or four times a day;
- pour two tablespoons of flax seeds with two glasses of boiling water and leave for eight hours. Take the strained infusion before meals, half a glass three to four times a day for five to six weeks;
- squeeze the juice out of potatoes and take it before meals (twenty minutes before) a quarter glass four times a day for three weeks;
- Fry the buckwheat until it turns dark brown. Crush the resulting mass into powder and use a pinch three or four times a day;
- You can quickly stop heartburn by chewing a piece of horse sorrel or calamus root. These plants have the ability to reduce the acidity of gastric juice and thus reduce its damaging effect on the esophageal mucosa. Also, horse sorrel and calamus protect the mucous membrane from the harmful effects of hydrochloric acid.