In the modern world, it is difficult for a person to lead a healthy lifestyle. Due to poor nutrition and alcohol intake, internal organs are negatively affected. This leads to various diseases and pathologies of the digestive organs.
The pancreas is a multifunctional organ of the human digestive system. It participates in metabolic processes and carries a double load. But people remember about it only with diagnoses such as pancreatitis and diabetes.
Pancreas: role
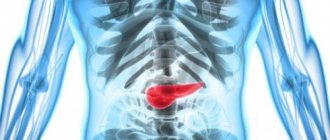
The pancreas regulates the digestion process.
The role of the pancreas is very significant in human life. It is involved in the secretion of enzymes that synthesize nutrients and the hormone insulin, and also regulates the entire process of food digestion.
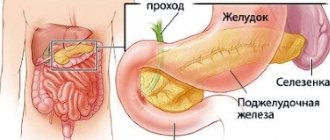
Pancreatic juice of the gland helps enhance the process of digestion of food. This organ is located behind the stomach at the level of the thoracic and lumbar vertebrae in the abdominal cavity. Improper functioning of the organ contributes to the development of diabetes, pancreatitis and pancreatic necrosis.
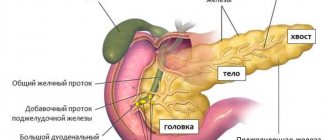
The digestive gland is divided into a head, body and tail. A change in the size of these sections leads to improper functioning of the gland and the development of various diseases. Any disorders of this organ can adversely affect the stomach, liver, heart and spleen.
Because the gland is very close to them and leads to other diseases of these organs. For this reason, it is important to know the size of this organ and what its deviation from the norm can lead to.
Other methods
Other diagnostic methods include:
- Ultrasound examination of the abdominal area (i.e. sonography).
- Performing computed tomography.
- Taking general laboratory tests of blood, urine, and feces to assess the functional status of the digestive system and the entire body as a whole.
They also conduct a preliminary conversation with the patient as part of the initial appointment with a gastroenterologist, during which they take a detailed anamnesis, finding out the details of the symptoms.
Pancreas size in a healthy person
The pancreas is the same size in both men and women.
Not everyone knows the size of the pancreas of a healthy person. And its parameters directly affect the condition of the organ itself and indicate the development of diseases.
A healthy digestive gland has an elongated shape and a tail curved upward. In men and women it is the same size: length on average from 16 to 23 cm, width - up to 9 cm, and thickness - up to 3 cm. The length of the head of the gland is up to 32 mm, the body is up to 21-25 mm, and the tail is up to 30 -35mm.
Treatment
Therapeutic assistance for dilation of the Wirsung duct may coincide with the treatment of the primary pathology, that is, pancreatitis. When the pancreas returns to normal, all its ducts are stabilized.
Acute pancreatitis is treated with a fasting diet, medication, and analgesics. In addition, droppers are prescribed to administer saline and colloidal solutions and medications that inhibit enzyme activity. In some cases, surgical intervention may be required in the form of removal of calculi (that is, stones) and resection of the inflamed area of the gland.
Chronic pancreatitis, which causes constant dilation of the Wirsung duct, is treated by following a diet, and, in addition, through vitamin therapy, consumption of painkillers prescribed by the doctor and replacement therapy with enzyme preparations. A diet against the background of duct enlargement involves introducing strict restrictions on the menu of fatty foods and fast carbohydrates. It is preferable to eat dietary meat and slow carbohydrates.
Causes of pancreatic diseases
Inflammation of the pancreas can cause pancreatitis.
The development of acute inflammation is rapid and can develop into a chronic form.
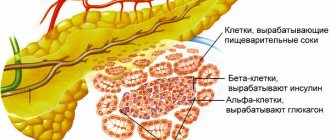
In diseases of the gland, the enzymes that it produces do not pass into the intestines, as during normal activity, but are activated inside the organ, thereby destroying it.
Toxins released into the bloodstream cause serious harm to other internal organs. The causes of inflammation can be excessive alcohol consumption, spicy and fatty foods, as well as cholelithiasis. Doctors include other risk factors:
- Duodenal disease;
- Surgical intervention for stomach diseases;
- Abdominal injury;
- Taking medications;
- Infectious diseases and hepatitis;
- Metabolic disease;
- Hormonal disorders;
- Heredity;
- Poor nutrition.
All these factors in their own way disrupt the normal functioning of the digestive gland. Violation of the outflow of pancreatic juice into the intestines leads to premature activation of enzymes in the organ itself. The gland tissue can be replaced by scar tissue and functions (endocrine and exocrine) are disrupted, which again leads to major inflammation.
Prevention and diagnosis of such diseases is mandatory for everyone. If you do not go to the doctor in time, the disease will lead to various complications. Very often, patients with pancreatitis also suffer from inflammation of the gallbladder.
Symptoms of pathology
The main symptom of the development of pathology is a violation of the digestive processes. Pancreatitis can cause dilation as well as narrowing of areas of the Wirsung duct. Experts call this pattern the chain of lakes syndrome. The contours of the canal become uneven, and solid inclusions, which are calcifications or stones, are found in their lumen. Additional symptoms of the disease are:
- The appearance of severe pain in the hypochondrium area (the fact is that pain, as a rule, is not relieved by antispasmodics and analgesics).
- The occurrence of diarrhea and pasty stools.
- The appearance of nausea, vomiting and weight loss.
- Decreased appetite along with specific signs indicating persistent dilation of the gland canal.
Preparing for an ultrasound
An ultrasound of the pancreas will help make the correct diagnosis.
It is difficult to make a diagnosis of inflammation due to the location of this organ. It is located near the stomach and intestines, where gas is produced.
To obtain a normal picture, it is necessary to eliminate gases before performing an ultrasound, otherwise the ultrasound may not penetrate.
Two days before the examination, you should not eat foods that lead to the accumulation of gases (legumes, vegetables, carbonated water, flour and sweets). In the morning hours a person has few gases in his organs and therefore it is recommended to go at this time.
You should start the ultrasound on an empty stomach (last meal within 12 hours). On the day of the examination, do not take medications or alcohol. Sometimes medications are prescribed to cleanse the intestines. Failure to follow these simple recommendations increases the likelihood of misdiagnosis by up to 40%.
It is important to know that in this way the doctor can only give information about the appearance and size of the gland. And for an accurate diagnosis, you need to undergo additional research: computed tomography and blood tests. On an ultrasound scan of a person with a healthy pancreas, the doctor reveals the following:
- Absence of formations and anatomical anomalies;
- Standard gland sizes;
- The main duct is 1.5 to 2 mm wide;
- Clear outline of the organ;
- Homogeneous structure;
- Echogenicity, as in the liver and spleen.
All these factors together indicate the healthy state of the organ. If one of the indicators does not correspond, this indicates the development of inflammation.
Why is puncture needed and how is it performed?
Why is pancreatic puncture needed? If the patient first discovers any unclear tissue formation in the gland, then to make an accurate diagnosis it is necessary to puncture it with a thin needle under ultrasound control. In addition, puncture may be performed for therapeutic purposes to evacuate pseudocysts, abscesses, or fluid around the gland.
Contraindications to puncture are some blood diseases accompanied by a reduced number of platelets and slow blood clotting time. The puncture is also done with caution in patients in serious condition.
Before the puncture, the patient’s skin is treated with alcohol and iodine at the site of the future puncture. As a rule, local anesthesia is given for puncture. Then the skin is pierced with a special guide needle, through which another thin needle is then inserted, observing its direction using an ultrasound scanner. When the tip of the needle reaches the lesion, the doctor uses a syringe to suck out a small amount of tissue, pull out the needle and apply the material onto a special glass or into a test tube. The puncture results prepared in this way are sent to the laboratory for further study.
Often, only puncture and tissue analysis can provide an accurate diagnosis.
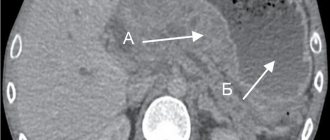
Ultrasound-guided pancreatic puncture
Prevention of organ dysfunction
To protect yourself from various diseases that are associated with disruption of the duct of Wirsung, you must:
- Completely get rid of all bad habits.
- Preference should be given to foods low in sugar, fat, salt and cholesterol.
- It is necessary to eat a varied diet that contains plenty of fresh vegetables, grains and fruits.
- You need to drink about two liters of water daily.
- From time to time you need to arrange fasting days for yourself.
- It is very important to play any sport.
- You should always get proper rest (namely, sleep at least eight hours a day) and avoid stressful situations.
- It is necessary to promptly treat infectious and viral diseases.
- During the autumn and winter periods, be sure to take complex vitamins.
The normal state of the duct is of great importance for many processes occurring in the human body. When the channel parameters deviate from the norm, a huge number of chronic or acute pathologies can occur. Therefore, it is necessary to monitor your health, maintaining in every possible way the normal functioning of absolutely all internal organs.
What is the drug treatment for this pathology?
As part of the treatment of pancreatitis, the doctor may prescribe the following medications:
- Use of calcium supplements.
- Treatment with choleretic drugs.
- Therapy with hormonal drugs.
- Use of drugs with sedative effects.
- Application of metabolite complexes.
- The use of drugs that have an enveloping effect.
Treatment of chronic forms of pancreatitis includes the use of vitamin complexes, as well as choleretic and enzyme medications in the form of “Creon”, “Festal”, “Digestal” and “Pansitrate”. If there is a disturbance in the functioning of the intestines, drugs in the form of Cisapride and Domperidone may be prescribed.
Tumors
Primitive neoplasms of the pancreas in childhood are quite rare. These tumors can be divided into three main groups: exocrine, endocrine and cystic lesions
.
Secondary lesions of non-Hodgkin's lymphoma, neuroectodermic tumors and retroperitoneal neoplasms (neuroblastoma) are more common.
Pancreatoblastoma is the most common pancreatic tumor in young children. It is an infantile-type pancreatic carcinoma with histological similarities to normal fetal pancreas at 8 weeks' gestation and demonstrates elevated alpha-fetoprotein levels in one third of cases.
On ultrasound, most pancreatoblastomas appear as well-defined heterogeneous lesions with solid and cystic components. Cystic formations are hypoechoic with hyperechoic internal septa. Sometimes a hypoechoic solid mass is found. Congenital cases of pancreatoblastoma in combination with Beckwith-Wiedemann syndrome have been described, and they are predominantly cystic.
Although pancreatoblastoma is considered the most common malignancy in children, recent studies have shown that solid pseudopapillary epithelial neoplasm (SPEN) is the most common pancreatic tumor in children.
SPEN is a lesion with low malignant potential that most commonly affects women of reproductive age. On ultrasound, the tumor usually appears as a well-defined large mass with varying characteristics depending on the presence of cystic and solid components, intratumoral hemorrhage, and calcifications. The fibrous capsule may be identified as an echogenic or, less commonly, hypoechoic rim.
Neuroendocrine tumors arise from pancreatic islet cells. On ultrasound, insulinomas are usually round or ovoid, hypoechoic with a hyperechoic rim. Tumors with larger islet cells, usually malignant insulinomas, gastrinomas (or other neuroendocrine tumors), may have a heterogeneous ultrasound appearance depending on the presence of cystic areas, hemorrhage, necrosis, and calcifications.
Nesidioblastoma is a similar neoplastic disease of the pancreas, characterized by new differentiation of the islets of Langerhans from the pancreatic ductal epithelium with subsequent hyperproduction of insulin. Ultrasound shows increased echogenicity and volume of the pancreas. Nesidioblastosis is often associated with hypoglycemia and Beckwith–Wiedermann syndrome.
Moreover, the pancreas may be involved in non-Hodgkin lymphoma, especially large cell lymphoma and sporadic Burkitt lymphoma. On ultrasound, these tumors are very hypoechoic and can variably appear as single or multiple lesions or diffuse infiltration of the pancreas.