March 28, 2011
The pancreas is one of the smallest organs of the human body, but its malfunctions are immediately noticeable.
The pancreas is one of the smallest organs of the human body, the existence of which people usually remember only when visiting a gastroenterologist. Why the work of this gland is so important for the body, says Oleg Shifrin, head of the clinic department at the First Moscow State Medical University. I. M. Sechenov.
Why is the pancreas needed?
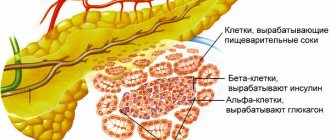
First of all, it produces digestive enzymes
necessary for digesting food. These are proteases that are involved in the digestion of proteins, lipases that break down fats and amylases - enzymes that help digest carbohydrates.
The ABCs of healthy eating
20 simple facts about how to eat right will help you build a balanced diet for health and well-being.
In addition, the pancreas is an internal secretion organ.
It produces the hormones glucagon and insulin
, which are necessary to maintain normal blood sugar levels.
Pancreas: the one and only. How to keep her healthy?
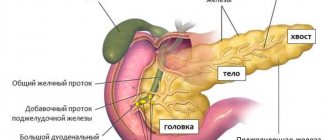
This is, in general, a small organ - from 16 to 23 centimeters in a healthy person - and so important. We talk about how to take care of the pancreas with Vasilisa Vladimirovna Ishchenko, a gastroenterologist at the Expert Clinic Kursk.
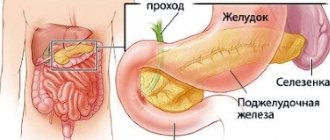
– Where is the pancreas located, and what functions does it perform?
– This gland performs the role of internal and external secretion. It is located behind the stomach at the level of the upper lumbar vertebrae. It plays a very important role in the process of digestion and maintaining internal homeostasis - maintaining the constancy of the internal environment of the body. In addition, it secretes hormones that are involved in the regulation of carbohydrate, fat and protein metabolism.
– What are the most common diseases that affect the pancreas?
– The most common are inflammatory diseases, less often – cystic fibrosis (a systemic hereditary disease), oncology. The hormonal part of the pancreas is affected by diseases such as diabetes. There are also complicated forms after inflammatory processes, destructive forms of pancreatitis. Chronic pancreatitis itself is a long-term inflammatory disease of the pancreas; it is characterized by irreversible morphological changes in the structure of this organ and leads to decreased function. This process is accompanied by pain.
– What manifestations may indicate the appearance of pancreatic pathology?
– Symptoms of pancreatic disease primarily include pain. Pain can occur in the upper abdomen, in the epigastric region (popularly called “in the pit of the stomach”), in the left hypochondrium, but can also radiate to the right, in the interscapular space, back. The pain syndrome intensifies after eating - this is a reaction to errors in the diet. When bending forward, the pain may decrease.
Pain may occur in the upper abdomen, in the epigastric region
Nonspecific signs that are not criteria for chronic pancreatitis include pain during belching, heartburn, and bloating. Exocrine pancreatic insufficiency occurs with a significant decrease in its functional activity. This can be characterized, first of all, by the release of neutral fat along with feces, flatulence, bloating, loss of body weight - this is already in an advanced stage. Also, accompanying factors include an increase in blood glucose levels when taking tests on an empty stomach - this is not yet diabetes mellitus, but a condition preceding it.
What indicators are included in a general blood test? Read here
The first stage of chronic pancreatitis is usually detected by test results. On the second, pain begins, the pain can be paroxysmal in nature. At the third stage, the pain is constant, it is no longer associated with food intake, signs of endocrine and exocrine insufficiency appear - the functions of the pancreas secreting digestive enzymes and the functions of the hormonal part are disrupted.
– How well developed is the diagnosis of pancreatic diseases?
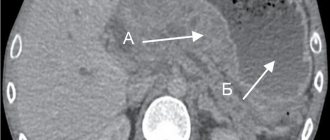
– Diagnosis of pancreatic diseases is based on anamnesis, collection of complaints from the patient, then laboratory tests follow. Radiation diagnostic methods are used - ultrasound, computed tomography, MRI of the pancreas. According to indications, endoscopic ultrasound and other more in-depth studies are used.
How to prepare for an abdominal ultrasound? Read here
– Do gastroenterologists identify any risk groups for pancreatic diseases?
– In the first place are people who abuse alcohol, smoke, and make big mistakes in their diet. It is this category that is most at risk of being diagnosed with toxic or metabolic chronic pancreatitis. Hereditary factors, concomitant autoimmune lesions of other organs, and diseases of the gastrointestinal tract play a role. High levels of cholesterol, calcium in the blood, chronic renal failure - these can also be attributed to predisposing factors.
If you know that a large feast is coming up, you can take two tablets of an enzyme preparation for prevention. Quote from the material “Picnics, barbecues and... stomach health”
– Vasilisa Vladimirovna, share your tips: what is harmful to our pancreas, what it likes, what it doesn’t like, how to keep it healthy?
– For those who want to stay healthy, and especially for those who already suffer from chronic pancreatitis, you need to know the rules for preventing pancreatic disease: abstain from alcohol and tobacco, follow dietary recommendations; You should eat often, in small portions, without overeating. Try to avoid eating fried, smoked, very fatty foods, and limit marinades. Steamed, boiled, baked dishes are preferable.
– In general, people who are fond of the folk “vitamin Tse” - wine, lard, butter...
– ... yes, they are first in line for pancreatic disease and, in particular, chronic pancreatitis.
Interviewed by Igor Chichinov
The editors recommend:
Acute pancreatitis: prevent and neutralize
An insidious pain-mask. Does abdominal pain always indicate problems with the gastrointestinal tract?
Is it possible to cleanse the liver?
For reference:
Ishchenko Vasilisa Vladimirovna. In 2015, she graduated from Kursk State Medical University, Faculty of General Medicine. 2016 – internship in the specialty “therapy”, Department of Internal Medicine. In 2016-2017, she underwent professional retraining in the specialty “gastroenterology”. Currently, he is a gastroenterologist at the consultative and diagnostic department of the Expert Clinic, Kursk. Receives at the address: Kursk, st. Karl Liebknecht, 7.
How does alcohol affect the pancreas?
In recent years, alcohol consumption in the world has been constantly increasing. In our country alone, it is about 15 liters of pure alcohol per person – including infants and pensioners. And alcohol is a strong toxin that negatively affects the pancreas. Consumption of any amount of alcohol leads to damage and death of pancreatic cells
- the cells of the pancreas.
Unlike the liver, there is no lower limit for a dangerous dose of alcohol set for the pancreas, and scientists believe that it is extremely low - at the level of just a couple of sips of alcohol. Moreover, the pancreas of the female body begins to suffer at an even lower dose than for men. In addition, alcohol provokes a narrowing of small vessels that feed the pancreas, which disrupts its blood supply
and causes cell death.
Causes of pancreatitis
One of the functions of the pancreas is the production of trypsin
. This is a special enzyme involved in the digestion of proteins. During normal operation of the pancreas, trypsin becomes active only in the intestines, but if for some reason trypsin is activated while still in the pancreas, it begins to break down the tissue of the gland itself, which leads to irritation and inflammation.
Alcohol can activate trypsin, which is why chronic pancreatitis or attacks of acute pancreatitis often occur in people who drink frequently. Globally, the number of people with chronic pancreatitis is growing, and researchers attribute this to increased alcohol consumption.
But pancreatitis can be caused not only by alcohol. In every third patient, it is not possible to establish the cause of the disease at all; in this case, pancreatitis is called “idiopathic.” This form of the disease is typical for adolescents or older people. There are other reasons for the development of pancreatitis
, which are much less common:
- autoimmune disorders
, as a result of which the human immune system itself begins to fight the pancreas; - genetic abnormalities
that stimulate the development of pancreatitis in a child from birth; - cystic fibrosis
, which destroys internal organs, including the pancreas.
If a person has attacks of acute pancreatitis periodically, then there is a high probability that pancreatitis will become chronic and lead to irreversible consequences. If the cause of acute pancreatitis is alcohol, then the chronic form of the disease is called “alcoholic pancreatitis.”
Nutrition and pancreas
“During the process of evolution, this organ was tuned to work in a certain mode,” says Shifrin. If there are long gaps in food intake, the rhythm of
the pancreas is disrupted - the secretion of its enzymes and insulin.
If the diet remains irregular for a long time, food digestion is disrupted and the risk of developing diabetes increases. Meals should be fractional, preferably 4-5 times a day, with approximately equal breaks between meals. Both the pancreas and other digestive organs work most efficiently in this rhythm. Food needs to be varied
, and two or three times a day - also hot. And also do not contain too much animal fat.
Treatment of acute and chronic pancreatitis
Patients with acute pancreatitis should be admitted to a surgical or intensive care unit. Treatment is prescribed depending on the form of the disease; mild forms of pancreatitis can be cured easier and faster. The patient must be put on a diet
. The first few days are prescribed complete fasting with plenty of drinking of alkaline water without gas. Then the patient is transferred to liquid porridge, gradually expanding the diet. It is important that the patient receives small portions of healthy food.
In addition to diet, the patient may be prescribed medication to normalize the functioning of the pancreas. After completing treatment in a hospital, the patient goes under the supervision of a gastroenterologist, who must prevent relapse.
If an exacerbation of chronic pancreatitis occurs, the patient is also prescribed fasting with a gradual transition to fractional low-fat meals. Cold can be used as a temporary surgical measure to combat the symptoms of pancreatitis. If you apply cold to the areas of the pancreas, you can reduce the production of its enzymes. This can also be done with the help of medications.
, diet is an important therapeutic measure in the fight against pancreatitis.
. It is necessary to switch to fractional meals, give up alcohol, carbonated drinks, coffee, tea, spices, spicy, fried and salty foods. The emphasis should be on low-fat, high-protein foods.
Pancreas and excess animal fats
“Modern people, as a rule, eat incorrectly and are detrimental to themselves,” notes Shifrin, “many everyday foods contain excess animal fats.” Excess of this difficult-to-digest fat causes the pancreas to work in a forced mode - to secrete excessive amounts of digestive enzymes. As a result, digestive juice becomes thicker, and its outflow is disrupted. “In this way, the process of self-digestion of the pancreas begins,” says Shifrin, “or its inflammation - pancreatitis.” According to Shifrin, there has been a real epidemic of pancreatitis
.
The incidence of pancreatitis in all developing countries has increased two to three times. At the same time, it is impossible to single out foods that are absolutely beneficial or harmful for the pancreas. The most important thing for maintaining the health of this organ is moderation
. Any excess intake of food ultimately turns out to be harmful because it disrupts the normal secretion of digestive enzymes from the pancreas.
Causes
Causes of inflammation of the pancreas:
- Infectious diseases;
- As a result of injuries;
- Changes in the blood vessels of the pancreas;
- Inflammatory processes of other abdominal organs;
- Stagnant processes, formation of stones in the ducts of the gland;
- Cholecystitis;
- Allergic reactions to medications;
- Alcohol intoxication;
- Gallbladder diseases;
- Nutritional disorders (predominance of fatty, spicy foods in the diet, excess nutrition).
An attack begins when the secretion stagnates and the gland tissue is destroyed under its influence.
The chronic course of the disease is associated with the onset of morphological changes in tissues and the impact of any risk factor on the damaged organ. At this moment, exacerbation and new profound changes in tissues begin.
Symptoms of pancreatitis
Both forms of pancreatitis are accompanied by pain, disorders of the stomach and intestines, nausea and vomiting (these are the most characteristic symptoms of pancreatitis). However, it is worth taking a closer look at the symptoms of the acute and chronic forms of this disease.
Acute pancreatitis
Characterized by very severe pain. It is impossible to endure such pain, so an ambulance is immediately called for the patient and the patient is taken to the surgical department. The patient experiences pain in acute pancreatitis both in the upper abdomen and throughout the entire girth of the abdomen (girdling pain). Nausea, vomiting, and bloating appear. The patient complains of pain when palpating the abdomen. The heart rate increases and blood pressure may drop.
Chronic pancreatitis
Symptoms of chronic pancreatitis appear permanently and periodically worsen after exposure to various irritants. A person feels a constant dull pain in the epigastrium and both hypochondriums; due to a lack of enzymes for digesting food, diarrhea, bloating in the abdomen, and unstable stool may occur. During periods of exacerbation of pancreatitis, the patient should follow the instructions of his doctor or contact an ambulance service.
Constipation with pancreatitis
With reactive inflammation, constipation may occur. But its cause is not the disease itself, but a violation of the outflow of bile. Constipation needs to be treated, but the underlying cause must first be ruled out.
What foods are recommended to consume for pancreatic diseases?
For diseases of the digestive system, it is recommended to consume low-fat foods, boiled or baked. An example menu in this case looks like this:
- porridge, and especially buckwheat and oatmeal;
- pasta;
- lean meats and fish;
- soups, broths;
- fermented milk products;
- vegetables - boiled, baked or raw.
To treat chronic pancreatitis, you should follow a diet high in protein. It is advisable to exclude fats, fresh fruits and vegetables. All food is prepared boiled and baked.
It is prohibited to consume baked goods, fried foods, fatty meats, chocolate, alcohol, smoked, spicy and salty foods, tea and coffee.
To restore the functioning of the pancreas, these restrictions are not enough. Enzyme therapy is also necessary: therapeutic or preventive. Only a doctor can choose the right medication after studying the patient’s medical history. Make an appointment with a gastroenterologist in Krasnogorsk - don’t put off taking care of your health!