The pancreas is an important part of the human digestive system. The production of enzymes that affect digestion and the functioning of the entire body as a whole depends on how this organ functions. Where does the pancreas hurt? When diseases affect the pancreas, a person experiences characteristic pain of severe intensity that occurs in the hypochondrium area. They often acquire an encircling character and are therefore felt everywhere. Everyone needs to know what problems with the pancreas are characterized by.
The role of the pancreas in the body
It is difficult to overestimate the role of this organ, because after its complete removal a person usually does not live longer than one year³.
But why does this happen? On the shelves of pharmacies you can find enzyme preparations that compensate for the digestive function of the gland, and the lack of hormones can be compensated for by introducing their synthetic analogues into the blood. Unfortunately, not everything is so simple, since the endocrine function of the organ is very difficult to compensate. The pancreas produces many hormones and enzymes. The regulation of their secretion is associated with a huge number of factors that currently cannot be taken into account in hormone replacement therapy. Today, medicine can only correct the deficiency of any component, but not the functioning of the entire organ. The structure of the pancreas and the principles of its operation, discussed below, will help to understand this point more fully.
5 facts about the pancreas
- The most common organ disease is pancreatitis.
- Pancreatic enzyme preparations are made from the pancreas of slaughtered cattle.
- The pancreas begins to produce digestive juice within 2-3 minutes after eating.
- The organ has a similar structure to the salivary glands, which is why it was previously called the abdominal salivary gland.
- The gland is capable of digesting itself.
What can be revealed during examination by a gastroenterologist?
Most often, when examined by a gastroenterologist, chronic diseases of the stomach, pancreas, and gall bladder are discovered. These include gastritis, pancreatitis, cholecystitis. Sometimes the inflammatory process is localized in the small or large intestine, in which case the patient is diagnosed with colitis. Also, examinations can reveal benign and malignant tumors of the gastrointestinal tract, various surgical pathologies (gallstones, bleeding from ulcers) requiring surgical treatment.
The structure of the pancreas
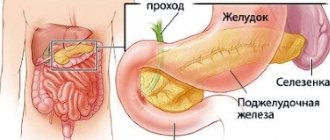
The pancreas is a fairly large organ (14-22 cm in length), which in a living person is located, contrary to its name, not under the stomach, but rather behind it. The “pancreas” was named because of its displacement under the stomach after a person’s death. It is also interesting that it is located separately from most digestive organs in the so-called retroperitoneal space, “settled” in it next to the kidneys and large vessels.
The structure of the pancreas consists of a head, body and tail. Its head adjoins the duodenum, and its tail approaches the spleen. Externally, the organ has a lobular appearance. Each such lobule is a functional unit of the gland (acinus), which consists of secretory cells and has its own small duct. The small ducts of each lobule unite into larger ones, and then flow into the main excretory duct, which runs in the center of the organ along the entire length.
Figure 1. Structure and topography of the pancreas. The red dotted line indicates the boundaries of the head, body and tail; black dotted line - ductal system of the gland. The bile ducts are marked in green. Illustration by Danila Melnikov
In the area of contact between the head of the pancreas and the duodenum, the above-mentioned excretory duct opens into the cavity of the latter. Thus, pancreatic juice formed in the lobules enters the intestine through the excretory duct.
How are the pancreas and biliary system related?
Figure 1 shows that another large duct, called the common bile duct, flows into the excretory duct of the pancreas. Since both ducts have one outlet into the intestine, with cholelithiasis it is possible to block not only the bile ducts, but also the pancreatic duct system. The rule also works in the opposite direction: with neoplasms of the pancreas, the common bile duct may be blocked. It is for this reason that jaundice can be a symptom of both diseases.
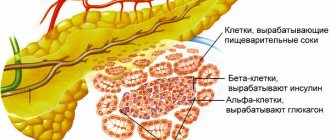
Endocrine part of the pancreas
In addition to the lobules with exocrine cells involved in the production of pancreatic juice, the gland has so-called pancreatic islets. They are also called the islets of Langerhans in honor of the scientist who discovered them. These are small clusters of cells that are “scattered” inside the organ, mainly in its tail part. These cells do not have ducts, since their secretions are absorbed by adjacent microvessels and enter directly into the blood. The main products of pancreatic islets are hormones: insulin and glucagon.
Thus, the pancreas essentially combines two completely different organs: digestive and endocrine. Glands of this type, which remove secretions through ducts and at the same time secrete hormones into the blood, are called mixed secretion glands.
Obesity and pancreatic diseases
In addition to the fact that acute pancreatitis develops more often in obese individuals, the latter also contributes to the development of type 2 diabetes mellitus. With this form of diabetes, there is no direct damage to the pancreas. However, tissue resistance to insulin develops, which ultimately leads to hyperglycemia and the corresponding symptoms described above. Therefore, it is important to eat in moderation, watch your caloric intake and be physically active.
Symptoms of pancreatitis in men and women
Pancreatitis presents with similar symptoms in men and women. The main one is a sharp pain that surrounds the abdomen and can radiate to the back and shoulder blades. At the same time, the sensations do not intensify during coughing, sneezing or taking a deep breath, which is typical for cholecystitis and appendicitis. Sometimes pain is accompanied by vomiting and nausea, which, however, do not lead to a weakening of symptoms. The disease is also characterized by other manifestations:
- pale or blue skin;
- a sharp decrease or increase in temperature;
- colic in the intestines;
- cardiopalmus.
Attention!
Acute pancreatitis can cause internal bleeding, which is often fatal. Therefore, at the first occurrence of painful sensations of a chronic nature, it is necessary to undergo diagnostics.
Functions in the body
The pancreas has two fundamentally different functions: exocrine and endocrine. In this regard, there is a complete correlation with the structure of the organ, as we have seen above. Let's look at each of the functions separately.
Exocrine function
The prefix “exo-” translated from Greek means outside, outside. In anatomy, exocrine glands are called glands that have ducts and the secretion of which is released through them into various cavities. In this case, pancreatic juice flows through the pancreatic duct and enters the intestine. Pancreatic juice is a liquid consisting of water, sodium bicarbonates and enzymes. Each of the components has a meaning:
- Sodium bicarbonate is a substance necessary to neutralize the aggressive acidic contents that flow from the stomach into the intestines. The thing is that acid is a damaging factor for the intestinal mucosa. Therefore, when hydrochloric acid as part of a bolus of food enters the intestine, it immediately reacts with the aforementioned bicarbonate and becomes harmless.
- Enzymes refer to special protein structures that break down food components: proteins, fats and carbohydrates. For each of these nutrients, pancreatic juice contains its own enzymes that break them down into simpler compounds. For carbohydrates - amylase, for proteins - trypsin and chymotrypsin, for fats - lipase and phospholipase. This is necessary for the reason that the intestinal mucosa is not able to absorb nutrients in their original form.
- Water is a universal solvent and an ideal medium for the remaining components.
In the absence of bicarbonates, gastric contents would form ulcers in the intestines. A lack of enzymes would lead to the inability to obtain the necessary nutrients and, as a consequence, to various metabolic disorders. It is these processes that occur in the body when the gland duct is blocked by a tumor, a stone, or when most of the organ is destroyed (with chronic pancreatitis).
Why doesn't the pancreas digest itself?
This question is quite reasonable, because pancreatic tissue, like all other organs and like the food we eat, consists of proteins, fats and carbohydrates. However, pancreatic juice enzymes normally do not cause any damage to the gland. The thing is that enzymes are initially secreted in an inactive form. Only after the enzymes in pancreatic juice enter the intestines do they become activated. The enzyme enteropeptidase, produced by the intestinal mucosa, is responsible for this process.
Endocrine function
The prefix “endo-” has the opposite meaning - in, inside. The endocrine part of the pancreas (pancreatic islets) secretes several hormones directly into the blood, the main ones being insulin and glucagon.
The importance of insulin for the body
Insulin is one of the most significant hormones in the human body. The main function of this substance is the distribution of glucose from the blood to organs and tissues. The hormone is produced especially actively in the first few hours after eating.
Figure 2. Functions of insulin in the body. Image: Ismail Jarmouni / Wikipedia (CC BY-SA 4.0)
During the digestion of food, complex carbohydrates are broken down into simple molecules, and glucose is the main product of this process. Glucose is the main energy substrate for almost all cells in the body. Without it entering the cells, their work will stop, just as a steam locomotive will stop without coal. In this comparison, insulin acts as a fireman throwing coal into the firebox of a steam locomotive. In addition to carbohydrates, insulin takes part in fat and protein metabolism. Without this hormone, the synthesis of the body's own proteins and fats is disrupted.
We can talk about the functions of insulin for a long time. However, it is very clear what happens to a person when this hormone is not produced or does not work for other reasons, which happens in patients with diabetes. All organ systems suffer: cardiovascular, immune, nervous - almost all organs are affected by the lack of glucose supply. The exception is the brain, which can take up glucose from the blood even without insulin. But as diabetes progresses, the brain also suffers damage due to vascular damage.
Glucagon and its functions
Glucagon is a complete insulin antagonist. If insulin stimulates the entry of glucose into cells and the synthesis of proteins and fats, then glucagon reverses these processes. The need for this arises during the period of fasting in order to release nutrient reserves into the blood from the depot and thereby constantly maintain a certain concentration in the blood. This is especially true during physical activity to ensure that fatty acids and glucose enter the bloodstream to fuel muscles. Insulin and glucagon are not produced separately; these hormones always work in pairs, clearly regulating metabolic processes in the body.
What does a gastroenterologist treat?
A gastroenterologist deals with congenital and acquired diseases of the digestive system.
The digestive tract consists of the mouth, pharynx, esophagus, stomach, small and large intestines. The pancreas, liver, and gall bladder also take part in the digestion process. A gastroenterologist examines and treats diseases of all of the above organs.
The most common pathologies of the digestive system:
- Chronic gastritis;
- Peptic ulcer of the stomach and duodenum;
- Gastroesophageal reflux disease;
- Chronic pancreatitis;
- Chronic cholecystitis;
- Biliary dyskinesia;
- Non-alcoholic fatty liver disease;
- Chronic colitis of various etiologies;
- Malignant tumors of the gastrointestinal tract;
- Irritable bowel syndrome and others.
Sometimes a disease requires the collaboration of several specialists. In such cases, the gastroenterologist may refer the patient for consultation to a surgeon, endocrinologist, proctologist or other specialized doctors.
Symptoms of pancreas problems
Symptoms of pancreatic diseases vary greatly depending on the severity of the pathological process. The most common acute condition is acute pancreatitis. As for chronic diseases, these are mainly chronic pancreatitis, cysts and tumors. Type 1 diabetes mellitus stands apart, in which autoimmune damage to the endocrine apparatus of the gland occurs.
Figure 3. Proper nutrition to prevent pancreatitis. Source: BelSU
Symptoms of acute pancreatitis
Acute pancreatitis is a dangerous condition that is accompanied by destruction of the pancreas due to its self-digestion. This occurs due to a violation of the outflow of pancreatic juice and an increase in pressure within the ductal system, which ultimately gradually leads to the activation of enzymes before secretion into the intestine. The initial symptoms of acute pancreatitis are as follows:
- Sharp, sudden pain in the upper abdomen. The pain syndrome is distinguished by: high intensity, constancy, often encircling in nature. Less commonly, the pain spreads to the entire abdomen and very rarely is absent altogether.
- Specific taste in the mouth.
- Nausea.
- Repeated vomiting.
- Bloating.
- Yellow-bluish spots on the abdomen (rare).
Of these symptoms, the most persistent and constant is pain. The girdling nature of the pain is relatively specific for pancreatitis. The presence of other manifestations is variable. For this reason, acute pancreatitis in the initial stages is difficult to distinguish from other acute diseases of the abdominal cavity. However, the appearance of these symptoms 12-48 hours after drinking a significant amount of alcohol or some time after eating a large meal makes the diagnosis highly likely.
Important!
The described symptoms, especially pain, are a reason to seek help from an ambulance. Acute abdominal pain, combined with or without other symptoms, requires examination by a surgeon and urgent instrumental diagnosis.
Symptoms of chronic pancreatic diseases
Chronic pancreatitis
Chronic pancreatitis is a slowly progressive disease in which functional pancreatic tissue is replaced by nonfunctional connective tissue. Possible symptoms:
- Dull, aching pain in the upper abdomen, may be of a girdling nature.
- Nausea.
- Vomit.
- Alternating constipation and diarrhea.
- Loss of body weight.
- Yellowness of the skin.
- Symptoms of diabetes.
With an exacerbation of the process, the symptoms become the same as in acute pancreatitis.
Figure 4. Healthy pancreas and changes in it characteristic of acute and chronic pancreatitis. Image: Pikovit/Depositphotos
Pancreatic cysts and tumors
Pancreatic cysts are cavities with fluid that can be located both in the gland itself and in the tissues surrounding it. These formations can be congenital or appear as a result of various pathological processes. Small cysts do not manifest themselves in any way. Symptoms appear when the cyst becomes infected, becomes large, or causes pressure on nearby organs. Among the manifestations:
- Dull aching pain in the upper abdomen, constant or paroxysmal, can be girdling.
- Nausea.
- Vomit.
- Weakness and weight loss.
- Periodic increase in body temperature.
- Palpable tumor formation in the abdomen.
- Yellowness of the skin.
Tumors, both benign and malignant, are clinically identical to cysts. The difference is that malignant tumors more often cause jaundice, which is usually the reason for visiting a doctor. The appearance of pronounced symptoms in the case of malignant tumors, unfortunately, indicates an advanced process.
There are also special hormone-producing tumors of the pancreas. The most common of them is insulinoma. As the name suggests, this neoplasm is capable of uncontrollably secreting insulin into the blood, which causes low blood glucose concentrations. The following symptoms develop:
- Tremor.
- Weakness.
- Sweating.
- Constant feeling of hunger.
- Confusion, memory impairment.
- Epileptic seizures.
- Coma.
If you eat something sweet, these symptoms are smoothed out or disappear.
Symptoms of diabetes
Type 1 diabetes mellitus develops as a result of autoimmune damage to the insular apparatus of the pancreas. Because of this process, insulin is not secreted into the blood after eating, which leads to excessive concentrations of glucose in the blood (hyperglycemia). This manifests itself symptomatically:
- Increased urination.
- Thirsty.
- General weakness and fatigue.
- Increasing incidence of infectious diseases.
- Slow healing of wounds.
Typically, patients seek help at this stage of the disease. However, as the disease progresses, the number of symptoms may increase significantly due to the systemic nature of the disorders.
Popular questions and answers
We discussed important issues related to the pancreas with general practitioner Tatyana Pomerantseva .
Which doctor treats a person's pancreas?
Initially, you need to contact a therapist to undergo general tests and examinations that will show which organ functions are affected. If there is a violation of the exocrine system (responsible for digestive enzymes), a referral to a gastroenterologist is necessary. In case of endocrine pathology, contact an endocrinologist.
What are the first signs of problems with the human pancreas?
Since the pancreas is a complex organ, the symptoms for each pathology are quite specific. Let us list the main signs by which one can suspect a disease of this organ: • pain in the upper abdomen (often encircling in nature); • nausea and vomiting that does not bring relief; • heaviness in the stomach after eating fatty foods; • suspected diabetes mellitus).
What is the pancreas afraid of?
The two main “enemies” for the pancreas are alcohol and gallstone disease. Both cause acute pancreatitis in 90% of cases³.
The effect of alcohol on the pancreas
Alcoholic pancreatitis is common, but how does alcohol contribute to inflammation in the pancreas? The thing is that it affects the gland through three effects:
- Spasm of the sphincter of Oddi, a muscle that closes the outlet for pancreatic juice in the duodenum.
- Increased secretion of pancreatic juice by exocrine cells of the gland. This effect is especially pronounced when combining alcohol intake with fatty foods.
- Increasing the permeability of the ductal system for protein substances, which are pancreatic juice enzymes.
Thus, all conditions are created for the premature activation of digestive enzymes, which leads to the development of pancreatitis.
Alcohol is the main enemy of the pancreas. Photo: alexlmx/Depositphotos
Gallstones and pancreatitis
The connection between the common bile duct and the exit pancreatic duct has already been mentioned above. Because of this anatomical feature, stones in the biliary system can interfere with the release of pancreatic juice, which becomes the cause of biliary pancreatitis. Thus, the “enemies” of the gallbladder are also those of the pancreas. Common causes of gallstone disease are:
- Long breaks between meals.
- A diet high in fat and cholesterol, fried foods.
- Taking combined oral contraceptives in women.
- Obesity.
Treatment of acute pancreatitis
If acute pancreatitis is detected, the patient should be hospitalized immediately. Treatment should take place in a hospital setting, as this condition is very dangerous.
To relieve pain, antispasmodics are taken; in difficult cases, the contents of the stomach are pumped out to relieve the load on the gland.
In case of exacerbation of pancreatitis, patients require hospitalization with daily monitoring of blood parameters, water balance, leukocyte count, and enzyme levels in the blood serum during the first week. In the first 1–3 days, fasting and taking alkaline solutions every 2 hours are recommended.
During an exacerbation of chronic pancreatitis, the patient is shown therapy similar to the acute process. The patient must follow a diet throughout his life and take drugs from the group of antispasmodics and drugs that normalize the secretory function of the organ.
The most important thing in the chronic form of the disease is to maintain a diet that involves excluding fatty and fried foods from the diet. At the slightest violation of the regimen, the patient may experience discomfort and nausea. For intense pain, the doctor prescribes antispasmodics. Antisecretory therapy can be used for a short course.
Maintaining proper pancreas function
Unfortunately, not all pancreatic diseases have developed preventive measures, and some of these diseases are genetic in nature (for example, type 1 diabetes). But you can successfully prevent the most common pathology - acute pancreatitis.
To do this, first of all, you need to give up excessive alcohol consumption and adjust your diet. You should not abuse products such as:
- Rich bread.
- Fatty meats.
- Pork lard, beef and lamb fat.
- Sour vegetables and fruits.
- Ice cream, confectionery with cream.
- Fatty and spicy sauces.
- Deep fried food.
- Highly carbonated drinks.
- Strong coffee and cocoa.
- Products with artificial colors and preservatives.
For patients with chronic pancreatitis, it is better to try to exclude these foods from the diet completely. It is also recommended to avoid long breaks (more than 4-5 hours) between meals.
Diagnosis of the disease at the private medical clinic “Medunion”
Diagnosing this disease is not difficult, since the first signs speak for themselves. However, in order to prescribe adequate treatment, it is necessary to determine the form of the disease. To do this, the doctor performs laparoscopy - a method that allows you to examine the abdominal cavity from the inside using a special instrument.
If acute pancreatitis is suspected, laboratory tests are performed:
- General blood analysis
- Blood chemistry
- Analysis of urine
- Stool analysis
- Ultrasound, MRI or radiography of the abdominal organs
- Computed tomography according to indications
In the chronic form, the same studies are carried out, but it is better to take tests during the period of exacerbation of the disease.
Sources
- Guyton, A.K. Medical physiology / A.K. Guyton, J.E. Hall / Per. from English; Ed. IN AND. Kobrina. - M.: Logosphere, 2008. - 1296 p.: ill.
- Prives M. G., Lysenkov N. K., Bushkovich V. I. / Human Anatomy. — 12th ed., revised. and additional - St. Petersburg: Publishing house SPbMAPO, 2006. - 720 p., ill.
- Surgical diseases: Textbook / M. I. Kuzin, O. S. Shkrob, N. M. Kuzin, etc.; Ed. M.I. Kuzina. — 3rd ed., revised. and additional - M.: Medicine, 2002. - 784 p.: ill.
- Erika F. Brutsaert, MD. Diabetes mellitus // MSD Handbook - 2019.
- Imaeva A.K., Mustafin T.I., Polovinkina S.R. MORTALITY AND MORTALITY INDICATORS IN ACUTE PANCREATITIS AS AN INDICATOR OF THE STATE OF MEDICAL CARE AT THE REGIONAL LEVEL // Problems of social hygiene, health care and history of medicine. 2022. No. 6.
Diet for pancreatitis
For any form of the disease, the patient is prescribed a strict diet “Table No. 5p”, according to which it is forbidden to eat spicy and fried foods. All dishes are steamed, boiled or baked. Alcohol and smoking are also prohibited.
It is also necessary to limit salt intake and eat small portions 6 times a day. Dishes should always be served warm. It is necessary to exclude all products with a high content of extractives or essential oils (fish, meat broths, cocoa, coffee, etc.), fresh berries, vegetables, herbs, fruits, sour juices, carbonated drinks, marinades.
Toxic (drug-induced) pancreatitis
Drug-induced pancreatitis occurs in less than 5% of cases. The prognosis for this pancreatitis is generally good and the mortality rate is low. The pathogenetic mechanism of drug-induced pancreatitis includes:
- immunological reactions (6-mercaptopurine, aminosalicylates, sulfonamides);
- direct toxic effects (diuretics, sulfonamides);
- accumulation of toxic metabolites (valproic acid, didanosine, pentamidine, tetracycline), ischemia (diuretics, estrogens);
- increased viscosity of pancreatic juice (diuretics and steroids).
Demonstrating interactions between pancreatitis and drugs is usually difficult. Pancreatitis may develop within a few weeks of starting treatment. Rash and eosinophilia may occur. Meanwhile, patients taking valproic acid, pentamidine or didanosine do not develop pancreatitis until many months later due to chronic accumulation of the drug's metabolite.
When restarting treatment, patients should be closely monitored. If symptoms recur, the drug should be discontinued.
How does the reception work?
At the beginning of an outpatient appointment, the doctor asks in detail about the patient’s complaints, the presence of concomitant diseases, and heredity. After this, they proceed to a physical examination, including palpation, percussion, and auscultation of the abdomen. The gastroenterologist studies the results of previously performed tests and, if necessary, prescribes additional examinations to clarify the diagnosis. The appointment ends with drawing up a treatment plan, the doctor also gives recommendations on lifestyle changes and sets a date for the next visit.