When do we suspect an infant has GERD?
There is regurgitation (release of stomach contents into the oral cavity, regurgitation)
+ possible signs of esophagitis - inflammation of the esophageal mucosa:
- irritability, crying, fussing, and arching during feeding
- baby sucks on a pacifier but is fussy when eating
- refusing to eat or eating only during sleep
- lag in weight gain as a consequence
- sometimes coughing and signs of lung damage, which can be associated with the reflux of gastric juice
I would like to immediately note that for each such complaint one can find another medical explanation, not related to esophagitis.
Doctor's opinion
Gastroesophageal reflux disease can cause a lot of trouble for the child and his parents. Frequent regurgitation in infancy can cause milk or stomach acid to enter the respiratory tract. At older ages, there is a significant risk of developing bronchial asthma and other associated pathologies. A timely visit to an experienced gastroenterologist and following all his recommendations will help you avoid problems and keep the disease under control.
It is important to pay attention to all aspects of treatment, including dietary adjustments and correct sleeping position. In this case, the child will quickly forget about the unpleasant symptoms and will be able to live a full life. The habit of controlling your diet and not overeating will be very useful in adulthood. If the doctor recommends surgery, you should not be afraid of intervention. Modern laparoscopic technologies can significantly reduce the recovery period. The operation allows you to completely get rid of GERD and forget about the need to take medications.
GERD in an infant and anti-acid drugs.
When reflux disease is suspected, it seems logical to prescribe treatment to the baby in order to relieve him of bothersome symptoms
The most popular and effective group for older children and adults are drugs that suppress acidity, most often proton pump inhibitors (PPIs) .
These drugs have become extremely popular abroad and for the treatment of infants (in Russia it has been official since the year)
How popular are anti-acid drugs?
From 1999 to 2004, the frequency of PPI use in children under one year of age increased 7 times
Proton pump inhibitor utilization patterns in infants
In another study, 874,447 American children under one year old received anti-acid drugs from 2001 to 2013.
- 7.7% of infants received H2-histamine blockers
- 0.8% - proton pump inhibitors
- 1.2% managed to receive both types of drugs!
Question answer
Is it possible to treat heartburn with folk remedies?
Traditional methods are not suitable for treating GERD, especially when it comes to a child. You shouldn’t waste time looking for the right product; at best, you’ll just waste time. At worst, you will encounter an unpredictable reaction from the body.
What sports are contraindicated for GERD?
The ban is imposed only on activities related to lifting weights, bending the body forward, or significant tension in the abdominal muscles. Other sports are not contraindicated and will even be beneficial.
Or maybe check for GERD first?
In my practice, several times I came across children who had already received such treatment before me while their family lived in the USA or Europe.
Usually, infants received anti-acid drugs precisely in connection with those complaints that I wrote about just above, and not because of objective confirmation of inflammation of the esophagus according to the results of fibrogastroduodenoscopy (FGDS).
Endoscopy is not an easy procedure and requires special experience at this particular age. A thinner endoscope is also needed.
In most cases, if reflux disease is suspected, fiberoscopy is not done, but treatment is prescribed immediately.
Another option for confirming painful reflux is daily monitoring of acidity in the esophagus. The procedure is not available everywhere, even for adults. It is unrealistic to do this to a baby under one year old outside of selected gastroenterological centers.
stomach ultrasound in Russia ?
An excellent way to exclude a rare but very dangerous condition manifested by vomiting in infants - pyloric stenosis.
But for other situations it is useless.
As evidence, I will present the results of a comparison with the gold standard - a daily study of pH in the esophagus:
- sensitivity (up to 95%)
- specificity (11%)
Low specificity means that a positive examination result can occur too often in healthy children.
This is why ultrasound of the stomach is not included in the guidelines for diagnosing reflux disease in both children and adults.
So.
We came to the conclusion that after the differential diagnosis stage, the most logical and simple way out for a doctor who suspects reflux disease in an infant is to start treatment with anti-acid drugs.
Treatment of gastroesophageal reflux disease in Germany
Treatment for GERD will depend on the symptoms, age of the child, and overall health. In many cases, diet and lifestyle changes can help relieve GERD.
For babies:
- After feeding, keep your baby upright for 30 minutes.
- When bottle feeding, make sure the nipple is filled with milk. This will prevent your baby from swallowing too much air while eating. Try different nipples.
- Allow your baby to burp several times during feeding. Belching with a full stomach can cause reflux more often.
For children:
- Monitor your child's nutrition. Limit fried and fatty foods, mint, chocolate, caffeinated drinks, soda and tea, citrus fruits (including juices) and tomato products.
- Use smaller portions. Add small snacks between meals if your child is hungry. Don't let your child overeat.
- If your child is overweight, see a specialist for help with healthy weight loss.
- Eat dinner early, at least 3 hours before bed.
Your doctor may also recommend:
- Drug therapy. There are medications that help reduce the amount of acid in the stomach, which in turn reduces heartburn. These medications may include an H2 blocker or a proton pump inhibitor
- Calorie supplements. Some babies with reflux are unable to gain weight because they vomit frequently. If this is the case, your doctor may suggest: Adding rice cereal to your baby's diet. Give your child more calories by adding a prescribed supplement. Change the child's diet from milk or soy if the child has allergies
- Feeding through a tube. Some babies with reflux also have other problems, such as congenital heart defects or premature birth. These children often become sleepy and tired after eating or drinking. Other babies vomit after eating. These babies do better if they are constantly fed a small amount of milk. In both of these cases, tube feeding may be offered: baby formula or breast milk is given through a tube that is placed in the nose called a nasogastric tube. The tube passes through the throat into the esophagus. Catheter feeding may be used in addition to bottle feeding.
- Surgery. In severe cases of reflux, surgery may be performed. This option is usually recommended if the child is not gaining weight due to vomiting, has frequent breathing problems, or has severe irritation in the esophagus. Most often, the operation is performed laparoscopically through small incisions in the abdomen. A small tube with a camera at the end is placed into one of the incisions. Surgical instruments are inserted through other incisions. The surgeon looks at the screen to see the stomach and other organs. The upper part of the stomach is wrapped around the esophagus, which significantly reduces reflux. What are the complications of GERD Some babies and children with GERD cannot vomit. But their stomach contents still move up the esophagus and spill into the windpipe, which can cause asthma or pneumonia. The vomiting that plagues many babies and children with GERD can cause problems with weight gain and poor nutrition.
Over time, due to excess stomach acid in the esophagus, it can also lead to:
- Inflammation of the esophagus, called esophagitis
- Ulcers in the esophagus that may be painful and bleed
- Lack of red blood cells from bleeding ulcers (anemia)
And this is where the problems begin.
Small but already available statistics show not very convincing benefits from such treatment.
The results obtained are worse than in adults.
Why?
There are different versions.
The most convincing thing in my opinion is that some of the symptoms that bother the baby are not associated with reflux at all.
The baby will not say that he is tormented by heartburn or that he does not sleep and arches due to unpleasant sensations behind the sternum.
We are only guessing.
If we see no other explanation for complaints other than reflux disease, but have not received an effect from 4-8 weeks of treatment, we need to reconsider the situation from different angles.
Perhaps something was missed...
There is one more nuance. While proton pump inhibitors have not received official approval for children under one year of age in Russia, they can only be prescribed by decision of a medical commission.
I’ll answer the question right away: why is treatment only with anti-acid drugs discussed?
general information
GERD is traditionally considered an adult pathology, but according to statistics, it affects about 15% of children, and the likelihood of developing the problem increases with age. If before the age of 5 the disease is detected, on average, in one child out of a thousand, then between the ages of 5 and 15 years it affects almost every fourth child.
Constant irritation of the esophagus often leads to inflammation. In addition, the reflux of acid provokes damage to the bronchi (in 4 out of 5 cases, GERD is accompanied by the development of bronchial asthma), premature tooth decay, and an increase in diseases of the ENT organs. Lack of treatment significantly increases the risk of developing esophageal cancer in adulthood.
Alternative drugs - is there a place for them?
Nothing reassuring.
Drugs with a local protective effect - antacids (Phosphalugel is approved for infants) and alginates (for example, popular in the UK) have shown themselves to be even weaker. And this is logical, since their local effect is too limited in time.
Prokinetics , in particular Motilium in suspension, which is very popular in Russia, have a very weak evidence base and are not recommended by guidelines.
We will discuss the topic of prokinetics for GERD separately later.
3, total, today
Living with Gastroesophageal Reflux Disease
Many children outgrow this problem by 1 year of age; for other children, medication, lifestyle and diet changes can help reduce reflux, vomiting and heartburn.
Do not delay visiting the doctor if your child:
- Has reflux and is not gaining weight
- Has signs of asthma or pneumonia. These include coughing, wheezing, or difficulty breathing.
Before your visit, write down the questions you want answered. When you visit, write down the names of new medications, treatments or diagnoses, and any new recommendations your doctor gives you.
What determines the results of endoscopic treatment?
The method has many technical nuances, so the results of its application vary significantly. Cure after one endoscopic procedure ranges from 25 to 95%, and the final results of treatment in different hands range from 40 to 97%. More reliable results were obtained when using non-absorbable pastes - Teflon, Deflux, Dam+. The best results were observed with: primary procedures, low-grade reflux, the absence of gross anomalies of the ureteric orifice and bladder pathology.
What are the clinical manifestations of VUR?
An attack of acute pyelonephritis is the first clinical manifestation of the presence of vesicoureteral reflux in most children. The disease begins with an increase in temperature above 38.0 without catarrhal symptoms. In urine tests, the number of leukocytes and the amount of protein increase. Blood tests also determine a high level of leukocytes and an increase in ESR. Children with acute pyelonephritis are referred for inpatient treatment, after which a urological examination is usually performed. Occasionally there are complaints of pain in the abdomen or in the lumbar region on the affected side. In newborns, suspicion of reflux most often arises when dilation of the pelvis (pyelectasia) is detected according to ultrasound.
How is secondary reflux treated?
In case of secondary VUR, the diseases leading to its occurrence are treated (treatment of cystitis, bladder dysfunction, restoration of urethral patency). The probability of disappearance of secondary reflux after eliminating the cause ranges from 20 to 70%, depending on the disease. Less commonly, “self-healing” of secondary VUR occurs in congenital pathology. Often, even after eliminating the cause, secondary reflux persists, then treatment is carried out using surgical methods.
Why is vesicoureteral reflux dangerous in children?
In children, VUR is the most common cause of secondary renal shrinkage and impaired renal function. Reflux interferes with the removal of microflora that penetrates the urinary tract, leading to chronic inflammation of the kidneys (pyelonephritis). In addition, when urinating, the pressure in the renal pelvis increases sharply, causing damage to the kidney tissue. The outcome of chronic inflammation occurring against the background of impaired urine outflow is scarring of the kidney tissue with loss of kidney function (secondary kidney shrinkage, nephrosclerosis). Scarring of the kidney is often accompanied by persistent high blood pressure, which is difficult to respond to conservative therapy, which necessitates removal of the kidney.
What are the causes of PMR?
There are several main factors leading to dysfunction of the valve in the lower part of the ureter. Increased pressure in the bladder, together with insufficient fixation of the ureteric orifice, is accompanied by shortening of the valve section of the ureter and the occurrence of VUR. Chronic cystitis (inflammation) disrupts the elasticity of the tissues at the mouth of the ureter, contributing to the disruption of valve closure. A special place among the causes of VUR is occupied by congenital anomalies of the vesical ureter, including various variants of the anatomy of the ureterovesical junction.
How is the reflux treatment method chosen?
With both surgical and endoscopic treatment, good treatment results can be obtained. However, in practice, treatment results in different clinics vary significantly. As a rule, the surgeon uses the method that he is better at and which allows him to obtain acceptable treatment results. In Russian healthcare, the choice of surgical method is determined by the guidelines adopted in a given institution. Nephrologists are less likely to refer patients for surgical treatment, observing children and providing antibacterial treatment and infection prevention. It should be noted that this approach is justified with low degrees of reflux and the absence of urinary tract infection.
The article presents the results of an analysis of the possible causes of the development of gastroesophageal reflux (GER) in young children, and the principles of differential diagnosis. The modern principles of diet therapy, pharmacotherapy and surgical treatment of GER in young children are considered.
Gastroesophageal reflux in infants
The results of analysis of possible causes of gastroesophageal reflux (GER) in infants, the principles of differential diagnosis are presented. The modern principles of dietotherapy, pharmacotherapy and surgical treatment of GER in infants are examined.
The lack of a clear understanding of the clinical picture of gastroesophageal reflux (GER) in young children, clear criteria for differential diagnosis between this disease and regurgitation, underestimation of the severity of complications of GER and the prescription of therapy that is inappropriate to the severity of the condition lead to a chronic course of the disease from an early age, a decrease in the quality of life and in rare cases even to disability.
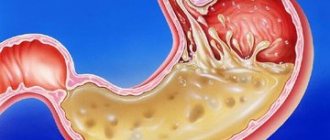
Currently, gastroesophageal reflux is considered to be the involuntary reflux of gastric or gastrointestinal contents into the esophagus due to a permanent or transient decrease in the tone of the lower esophageal sphincter, which disrupts the physiological movement of the bolus of food and is accompanied by the entry into the esophagus of unusual contents that can cause physical and chemical damage to its mucosa shells. Traditionally, a distinction is made between physiological GER, which does not cause the development of reflux esophagitis, and pathological GER, the presence of which leads to damage to the mucous membrane of the esophagus with the formation of reflux esophagitis and associated complications.
Clinical symptoms of GER differ significantly in children of different ages and are determined by the known anatomical and physiological features of the development of the digestive tract. In newborn children, the esophagus is funnel-shaped with the greatest narrowing in the cervical part; up to a year, the diaphragmatic narrowing is absent or weakly expressed, which contributes to frequent regurgitation of food. By the time the baby is born, the mucous and submucous membranes of the esophagus are well developed, and the muscle layer is poorly expressed. The formation of full-fledged esophageal muscles continues throughout the first decade of a child’s life. In newborns and infants, the entrance to the stomach is wide, the distal part of the esophagus is located above the diaphragm, there is a physiological insufficiency of the cardiac sphincter, which is located at the level of the diaphragm or below it, and the predominantly horizontal position of the child contributes to low pressure in the lower esophageal sphincter. In older age, the cardiac sphincter moves relative to the diaphragm lower into the abdominal cavity, the legs of the diaphragm contract during inhalation and increase pressure in the area of the lower esophageal sphincter. In the first year of life, children also experience weak development of the circular muscle layer of the cardiac part of the esophagus, the angle of His is not sufficiently pronounced, and the cardiac part of the stomach is not completely covered by the loop of Willis.
The described features, with harmonious physical development of a child in the first year of life and the absence of concomitant pathology, as a rule, do not lead to the formation of pathological GER. In children of the first year of life, regurgitation is considered as the equivalent of physiological GER and is recognized as an almost normal physiological phenomenon in children in the first months of life.
According to a survey of parents, 948 healthy children over 13 months old, regurgitation from 1 to 4 times a day was observed in every second child up to 3 months of age; at 10-12 months, regurgitation was observed in 5% of children. According to the literature, the peak frequency of regurgitation is observed at the age of 4 months (in 67% of children), sharply decreases from 61 to 21% at the age of 6-7 months, and they spontaneously disappear 12-18 months after birth [1, 2].
Pathological GER occurs in 8-10% of children in the first year of life [3, 4]. This disease can develop in children born prematurely, who have suffered chronic intrauterine hypoxia, asphyxia during childbirth, natal trauma to the cervical spine, who suffer from food allergies and lactase deficiency, and also have a family history of diseases of the upper digestive tract, in particular GERD. V.F. Privorotsky (2006) identified unfavorable factors in the early history of children with GERD, among which perinatal pathology occurs in 72.5%, a burdened allergic history in 49.6%, and early artificial feeding in 37.4% [5].
During the fetal period of intrauterine development, organs are formed and their functions mature. Among premature newborns (gestation period less than 38 weeks), acidic GER is diagnosed in 24% using 24-hour pH testing, of which 50% of children with intrauterine growth retardation and only 17% without intrauterine growth retardation [6]. With antenatal use of corticosteroids, acidic GER is found in 41% of premature newborns (gestational age greater than 34 weeks), and in the group of children who did not receive antenatal treatment with corticosteroids - in 16% [7]. A pathological pregnancy, prematurity, intrauterine growth retardation in the presence of regurgitation may most likely indicate the presence of GER due to an immature lower esophageal sphincter. An adequate assessment of this situation allows timely initiation of complex antireflux therapy.
Considering the topography of the nuclei of the vagus nerve innervating the esophagus, natal damage to the cervical spine may be one of the reasons for the formation of pathological GER. Such injuries occur most often (up to 86.5%) because during even normal childbirth the greatest load falls on the cervical spine [8]. In addition to persistent regurgitation and vomiting, various spinal deformities (torticollis, kyphosis, etc.), as well as pain associated with passive movements in the spine, can be observed. X-ray examination usually confirms the presence of injury. Vertebral displacements are detected in 20% of newborns with a birth injury; in 10.4% of children with a cervical spine injury, spondylograms show signs of subluxation in the middle atlanto-axial joint (Cruvelier’s joint) [8].
In children of the first year of life, an allergy to cow's milk proteins (CMP) induces the development of reflux in 15-21% of cases [9]. BCM-induced GER does not have typical clinical symptoms, traditional antireflux therapy is ineffective, which prompts further diagnostic searches, especially considering the high frequency of the described pathology [10].
Lactase deficiency is characterized by frequent, foamy, watery stools, abdominal colic, as well as regurgitation and vomiting. The development of GER in this pathology is caused by antiperistaltic contractions of the small and large intestine due to impaired motility and increased intraluminal pressure in the intestine. With a deficiency of disaccharidases, undigested carbohydrates accumulate in the lumen of the small intestine, osmotic pressure increases with excess water entering the intestinal lumen. Disaccharides are utilized by microflora, a large amount of organic acids and carbon dioxide is formed, which causes pronounced acidification of the intraluminal contents of the intestine and increased motility [11].
At an early age, GER has clear clinical manifestations. It is characterized by regurgitation in combination with weight loss, vomiting fountain, with an admixture of blood or bile, respiratory disorders up to the development of apnea and sudden death syndrome, unusual movements of the head and neck (Sandifer syndrome) associated with episodes of reflux and the presence of a hiatal hernia diaphragm [12].
A detailed study of Sandifer syndrome using intraesophageal pH-metry, cutaneous electromyography and video recording revealed a statistically significant association between contraction of the rectus abdominis muscles with the onset of reflux episodes, as well as an association of reflux episodes with the child's posture. It is hypothesized that contraction of the abdominal wall may induce GER. Researchers believe that GER may cause the development of Sandifer syndrome even in the absence of clinical symptoms of reflux, macroscopically detectable esophagitis and hiatal hernia. Despite the absence of typical symptoms of GER and the ineffectiveness of conservative antireflux therapy, Sandifer syndrome can disappear (resolve) after fundoplication surgery [13].
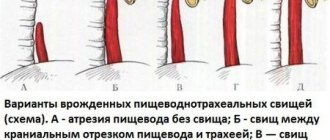
Differential diagnosis of pathological GER must be carried out with malformations of the organs of the upper digestive tract: congenital stenosis of the esophagus, achalasia cardia, chalasia cardia, congenital short esophagus, duplication of the esophagus, pyloric stenosis, sliding hiatal hernia, neuromuscular diseases. The results of an endoscopic study carried out in children with complaints of persistent vomiting mixed with bile, mucus, blood, showed clear age-related dynamics in the detection of malformations: in the early neonatal period, 12% of the examined children were found to have: esophageal atresia, hiatal hernia, atresia or duodenal membrane, Ladd syndrome; in the late neonatal period, pyloric stenosis (86%) and hiatal hernia (14%) were found in 9% of children; in children aged 1-12 months, only hiatal hernia (5.6%) was diagnosed among gastrointestinal malformations [14].
Certain difficulties arise in the differential diagnosis of clinical symptoms of congenital pyloric stenosis and pyloric spasm (table).
The diagnosis is made on the basis of an X-ray examination of the gastrointestinal tract with barium. With pyloric stenosis, there is a delay in the passage of barium from the stomach into the intestines for more than 12-24 hours; with pylorospasm, there may be a delay of barium in the stomach for 6-9 hours [15]. Clinical symptoms of GER can occur with a cyst or tumor of the mediastinum, vascular malformations due to compression of the esophagus and impaired peristalsis. Particular caution, despite existing screening, should be exercised if metabolic disorders are suspected.
With GER, characteristic signs of damage to organs that are anatomically closely related to the esophagus, the so-called extra-esophageal symptoms, may occur, but the vivid clinical picture often leads away the diagnostic search with the maximum focus of the doctor’s attention on the affected organ. Clinical masks of GER can manifest as damage to the ENT organs, bronchopulmonary and cardiovascular systems, and teeth.
Otorhinolaryngological symptoms of GER include constant coughing, a feeling of tickling and hoarseness of the voice (hoarse crying in infants), ear pain, and frequent otitis media. If for the mucous membrane of the esophagus the duration of contact with acidic (pH≤4) refluxate for 75 minutes over 24 hours is considered normal, then the mucous membrane of the laryngeal part of the pharynx can withstand such contact for no more than 15 minutes [16]. Damage to the mucous membrane of the larynx and pharynx - laryngeal (pharyngolaryngeal) acid reflux - occurs due to the reflux of the contents of the stomach and duodenum into the pharynx due to failure of the upper esophageal sphincter. Reflux appears periodically, depends on lifestyle, most often occurs in an upright position, heartburn is not a characteristic symptom, while normal clearance of the esophagus is preserved, esophagitis is rarely detected. Among children (age 3-34 months) with laryngotracheomalacia, GER was detected in 87%, while in the group without lesions of the ENT organs - in 39% [12].
It must be remembered that if in the first year of life a child often suffers from otitis and pneumonia in the presence of persistent regurgitation, then there is a high probability of having GER, which requires an appropriate examination and the prescription of pathogenetic therapy. Among children with respiratory disorders, pronounced GER was detected by pH-metry in 42% of cases, in children of the control group (without respiratory disorders) - in 8% [17].
In addition to chronic pneumonia, lesions of the bronchopulmonary system with GER include recurrent and chronic bronchitis and the formation of bronchial asthma. The frequency of GER in bronchial asthma in children is 55-80%. Characteristic clinical symptoms include attacks of coughing and/or choking mainly at night or after a heavy meal, a proven combination of respiratory and esophageal symptoms, a positive effect from trial antireflux therapy, prolonged course of bronchial asthma despite adequate therapy, non-atopic variants of bronchial asthma. Interestingly, GER can cause recurrent pneumonia in the absence of esophagitis, although normal results of pH monitoring do not exclude the diagnosis of GER as a cause of recurrent pneumonia [18].
One can think of a high supply of refluxate (usually acidic) with the appearance of erosions of tooth enamel and the rapid development of caries. GER-associated cardiovascular manifestations include arrhythmias (due to the initiation of the esophagocardial reflex) and pain in the cardiac region.
Among children over 1 year of age suffering from lesions of the digestive tract, GER occurs in 8.7-17% [5], and its occurrence can be caused by pathological conditions of both the esophagus and lower esophageal sphincter, and underlying organs. A key role is played by motility disorders of the upper and lower digestive tract. Among children with chronic constipation, lesions of the esophagus and cardio-esophageal junction are detected in 45%, depending on the nature of the pathology of the colon and the severity of stool retention; duodenogastric reflux is detected in 77.2%, accompanies inflammatory changes in the upper digestive tract, promotes the development of alkaline and mixed GER [19]. Duodeno-gastric reflux is an important pathogenetic factor in the formation of GER and is a manifestation of duodenal dyskinesia, that is, a violation of its tone, peristalsis and evacuation. The cause of duodenal dyskinesia can be not only its functional disorders, but also various developmental anomalies (high intestinal fixation, duodenum mobile, membranous atresia). Obstacles to the passage of food through the duodenum can be created by scar deformations of the bulb due to erosive and ulcerative processes, annular pancreas, external scars, cords or accessory ligaments (ligamentum cysto-duodeno-colicum), gastroptosis.
The cause of the development of GER may be an inflection of the stomach, which contributes to the formation of cardia insufficiency, or a sliding hiatal hernia.
A clear relationship has been established between the frequency of pathological conditions of the upper digestive tract and periods of physiological traction: 6-7 years, 9-10 years and 12-14 years [20]. The rapid growth of the child, imbalances of individual organs and systems of the body are reflected in the appearance of symptoms of insufficiency of physiological sphincters and dyskinesia of the upper digestive tract, in particular the appearance of GER (nausea, heartburn, belching of air and sour, vomiting of food). In this clinical situation, it is advisable to assess the physical development of the child, the rate of increase in height and body weight over the period of time preceding the onset of complaints, as well as to identify the presence of undifferentiated connective tissue dysplasia syndrome and possible instability of the cervical spine.
According to the recommendations of ESPGHAN (2005), treatment of regurgitation should be carried out sequentially in several stages: explanatory work with parents for the purpose of psychological support, normalization of the feeding regimen and the amount of food consumed, postural therapy to improve the gravitational clearance of the esophagus, increase the tone of the LES, adequate dietary therapy.
When breastfeeding, breast milk thickeners are used. Babies over 1-2 months of age can be given a heavier meal before each feeding, such as 1 teaspoon of dairy-free rice porridge.
When artificial feeding, specialized anti-reflux adapted milk formulas (AMC) are used, the viscosity of which increases due to the introduction of thickeners into their composition - gum or starch (rice, corn).
Currently, the following anti-reflux mixtures containing gum are available - Nutrilon AR (Nutricia, the Netherlands), Humana AR (Humana GmbH, Germany), Frisov (Frisland, the Netherlands), Nutrilak AR (Nutritek, Russia), Babushkino Lukoshko AR (Nutribio, Russia ). These formulas are used in a volume of no more than 1/3-1/2 of the total volume of the formula received at each feeding, and are given to the child before using the usual adapted milk formula. They are not recommended for use in full at each feeding for a long time due to the fact that thickening the food bolus with gum makes it difficult to absorb a number of nutrients, such as protein, fats, iron, zinc, manganese, which does not occur when using digestible carbohydrates [21].
Another category of specialized anti-reflux formulas containing digestible polysaccharide starch is recommended to completely replace the previously obtained milk formula; long-term use is indicated in order to achieve a lasting effect. A new mixture NAN antireflux (Nestle, Switzerland) has appeared in the line of antireflux mixtures with starch, which has an effect on various mechanisms leading to regurgitation.
The mixture contains potato starch as a thickener, which imparts optimal viscosity, is completely digested and well absorbed, has low osmolarity and low enzymatic potential, and is less susceptible to fermentation by microflora, which prevents the occurrence of functional discomfort and colic in the intestines. The protein component is represented by moderately hydrolyzed protein, which is easily digested and evacuated from the stomach at the rate of breast milk, which reduces intragastric pressure and helps reduce regurgitation. In addition, moderately hydrolyzed protein promotes the formation of soft stools, prevents allergies to cow's milk protein, and has an optimal amino acid composition for full growth. Additionally, the probiotic B. lactis 10×6 COE/g was added to the mixture in order to improve the condition of the microflora and immunonutrients (zinc, selenium, nucleotides).
If diet therapy is ineffective, it is necessary to move on to the subsequent stages of treatment of regurgitation, including the use of prokinetics, H2-histamine receptor blockers, proton pump inhibitors (not all of the listed pharmacological groups are registered in Russia for use in the neonatal period). In the absence of drug therapy, esophagitis can persist for a long time and within 1 year of life there is no normalization of morphological changes in the esophageal mucosa, despite the disappearance of symptoms of GER [22]. The results obtained indicate subclinical persistence of esophageal damage from an early age, which necessitates the need for population-based epidemiological studies of GERD, a long-term study of a cohort of families in which GERD was registered in early childhood, and identification of risk groups (with the onset of the disease in early childhood) for severe complications of GERD [23].
According to A.B. Alkhasova (2007), indications for surgical treatment of GER are the recurrent nature of the disease, the ineffectiveness or futility of drug therapy (100%), hiatal hernia (30%), stenosing RE (28%), esophageal metaplasia (22%), lag in physical development (46%), respiratory complications (19%), persistent vomiting (12%). In 64% of cases there are more than 2 indications for surgical treatment. Currently, the main method of surgical correction of GER in children is laparoscopic fundoplication. The Nissen cuff creates a valve mechanism that prevents the occurrence of pathological GER. In this case, all pH measurements decrease to normal values, which indicates the presence of physiological reflux [24].
Methods for examining children with suspected GER include fibroesophagogastroduodenoscopy with a biopsy of the esophageal mucosa, 24-hour pH-metry of the esophagus and stomach, manometry of the external esophageal sphincter, ultrasound of the esophagus, X-ray contrast study of the upper digestive tract, radioisotope study of the evacuation function of the stomach, magnetic resonance imaging of the cervical spine.
A balanced, multilateral, objective assessment of the condition of a child with clinical symptoms of GER will make it possible to make the correct diagnosis and carry out competent treatment and preventive measures.
Table
Differential diagnosis of congenital pyloric stenosis and pylorospasm
| Symptoms | Pylorospasm | Pyloric stenosis |
| Vomiting and regurgitation | from birth | more often from 2 weeks of life |
| Character of vomiting | frequent, intermittent | rarer and more constant |
| Amount of vomit | a small amount | “fountain”, the amount of vomit exceeds the amount of food eaten |
| Constipation | often, but sometimes the stool is independent | rare |
| Number of urinations | slightly reduced (to 10) | sharply reduced |
| Peristalsis of the stomach | rarely observed | in the form of an hourglass |
| Body mass | does not change or decreases moderately | sharp drop, less at admission than at birth |
| Gatekeeper | not palpable | palpable thickened |
| Secretion of gastric juice | normal | sharply increased |
| Acid-base balance | metabolic acidosis | alkalosis |
| Exicosis and decreased concentration of Cl ions | rarely | often |
M.I. Dubrovskaya
Russian State Medical University, Moscow
Dubrovskaya Maria Igorevna - Candidate of Medical Sciences, Associate Professor of the Department of Childhood Diseases No. 2
Literature:
1. Nelson SP, Chen EH, Syniar GM et al. Prevalence of Symptoms of Gastroesophageal Reflux During Infancy A Pediatric Practice-Based Survey. Arch Pediatr Adolesc Med. 1997; 151(6): 569-572.
2. Vandenplas Y., Belli, Benhamou P. et al. A critical appraisal of current management practices for infant regurgitation - recommendations of a working party. Eur J Pediatr 1997; 156: 343-357.
3. Sacre L., Vandenplas Y. Gastroesophageal reflux associated with respiratory abnormalities during sleep. J Pediatr Gastroenterol Nutr 1989; 9: 28-33.
4. Vandenplas Y., Goyvaerts H., Helven R. et al. Gastroesophageal reflux, as measured by 24-hour pH-monitoring, in 509 healthy infants screened for risk of sudden infants death syndrome. Pediatrics 1991; 88: 834-840.
5. Privorotsky V.F. Heterogeneity of gastroesophageal reflux disease in children: Abstract of thesis... Dr. med. Sci. St. Petersburg, 2006. 43 p.
6. Sadowska-Krawczenko I., Korbal P., Czerwonka-Szaflarska M. Influence of selected neonatal diseases on the incidence of gastroesophageal reflux in preterm neonates Med Wieku Rozwoj. 2005 Jul-Sep; 9(3 Pt 1): 317-24.
7. Sadowska-Krawczenko I., Czerwionka-Szaflarska M., Korbal P. Is antenatal corticosteroid administration associated with increased acid gastroesophageal reflux in preterm neonates? Med Wieku Rozwoj. 2004 Apr-Jun; 8(2 Pt 2): 359-64.
8. Ratner A.Yu. Neurology of newborns: acute period and late complications. M.: BINOM. Knowledge Laboratory, 2005. 368 p.
9. Salvatore S., Vandenplas Y. Gastroesophageal Reflux and Cow Milk Allergy: Is There a Link? Pediatrics 2002; 110:5:972-984.
10. Shumilov P.V., Dubrovskaya M.I., Yudina O.V. et al. Eosinophilic inflammatory diseases of the gastrointestinal tract and food allergies in children. Issues of modern pediatrics 2007; 6:4:43-53.
11. Mukhina, P.V. Shumilov, Chubarova A.I., et al. Modern approaches to the diagnosis and treatment of disaccharidase deficiency in children. Difficult Patient 2006; 4:9:12-16.
12. Pediatric Gastrointestinal Disease. Fourth edition. Hamilton, Ontario BC Decker. 2005. 2227 rub.
13. Frankel EA, Shalaby TM, Orenstein SR Sandifer syndrome posturing: relation to abdominal wall contractions, gastroesophageal reflux, and fundoplication. Dig Dis Sci. 2006; 51(4): 635-40.
14. Dmitrieva N.V., Shatskaya E.E., Dmitriev A.V., Tkachenko T.G.. Variants of gastrointestinal disorders in newborns. // Materials of the XIII Congress of Pediatric Gastroenterologists of Russia - 2006. — P.86-87.
15. Markov A.A., Markov A.S., Nesterov D.V. Modern approaches to the diagnosis of congenital pyloric stenosis in children // Medical scientific and educational journal. - 2003. - No. 15. - P.113-120.
16. Young RJ, Lyden E, Ward B. et al. A retrospective, case-control pilot study of the natural history of pediatric gastroesophageal reflux. // Dig Dis Sci. 2007 Feb;52(2):457-62.
17. Sacre L, Vandenplas Y. Gastroesophageal reflux associated with respiratory abnormalities during sleep. J Pediatr Gastroenterol Nutr 1989;9:28-33.
18. Rudolph CD, Mazur LJ, Liptak GS. et al. Guidelines for evaluation and treatment of gastroesophageal reflux in infants and children: recommendations of the North American Society for Pediatric Gastroenterology and Nutrition. // J Pediatr Gastroenterol Nutr. 2001;32 Suppl 2:S1-31
19. Tsvetkova L.N., Tsvetkov P.M., Nechaeva L.V. et al. State of the esophagus and gastroesophageal junction in children suffering from chronic constipation // Russian Bulletin of Perinatology and Pediatrics. - 2008. - T. 6. No. 53. - P. 30-42
20. Tsvetkov P.M., Kvirkvelia M.A., Gureev A.N. et al. Deviations in the rate of physical development of a child as a risk factor for the formation of gastroesophageal reflux // Questions of pediatric dietology. - 2009. - T.7, No. 2. — P.25-29.
21. Vandenplus Y., Rudolph CDat al. Pediatric gastroenterology reflux clinical practice guidelines., JPGN. 2009 49;498-547.
22. Orenstein SR, Shalaby TM, Kelsey SF et al. Natural history of infant reflux esophagitis: symptoms and morphometric histology during one year without pharmacotherapy. // Am J Gastroenterol. 2006 Mar;101(3):628-40.
23. Gold BD Is gastroesophageal reflux disease really a life-long disease: do babies who regurgitate grow up to be adults with GERD complications? // Am J Gastroenterol. 2006 Mar;101(3):641-4.
24. Alkhasov A.B. Surgical treatment of gastroesophageal reflux in children: abstract. dis... doc. honey. Sci. - Moscow, 2007. - 51 p.
How is the diagnosis made?
The main method for diagnosing PMR is voiding cystography: a 15-20% solution of a radiopaque substance is injected into the bladder through a catheter passed through the urethra until the urge to urinate appears. 2 x-rays are taken: the first - immediately after filling the bladder, the second - during urination. Based on cystography, PMR is divided into grades from 1 to 5 grades (Fig. 1). The criteria are the level of urine reflux and the severity of dilatation of the ureter. The mildest is the first degree, and the most severe is the 5th degree of reflux.
Refluxes detected by cystography are also divided into active (during urination) and passive (outside urination with low pressure in the bladder). In addition to detecting reflux and determining its degree, cystography provides important information about the patency of the urethra and suspects bladder dysfunction. Vesicoureteral reflux, which appears from time to time, is called transient.
What is vesicoureteral reflux?
Vesicoureteral reflux (VUR) is the return flow of urine from the bladder through the ureter into the kidney. Normally, urine moves unidirectionally from the kidney through the ureter to the bladder, and the return flow of urine is prevented by a valve formed by the vesical section of the ureter. When the bladder fills, the pressure in it increases, which leads to the closure of the valve. With reflux, the valve is damaged or weakened, causing urine to flow back toward the kidney. Approximately 20% of children with a urinary tract infection are diagnosed with vesicoureteral reflux.
What are the benefits of endoscopic treatment?
The advantages of endoscopic operations for reflux are obvious: low trauma, short hospital period, minimal risk of complications. If high efficiency is achieved (at least 70-80% of permanent cure after the first procedure), then the advantages of endoscopic treatment are undeniable. At the same time, with low efficiency, the number of repeated interventions and anesthesia increases, which reduces the feasibility of using the method, so surgical treatment of reflux remains relevant. It should be noted that an incorrectly performed primary endoscopic procedure sharply reduces the effectiveness of treatment, since the orifice of the ureter is fixed in a disadvantageous position.