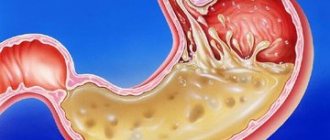
Under the influence of aggressive hydrochloric acid and enzymes found in the contents of the stomach and duodenum, inflammation occurs in the mucous membrane of a distant part of the esophagus, and erosions are likely to occur, leading to disruption of the passage of food.
The main diagnostic criterion for gastroesophageal disease is heartburn or acid regurgitation. It is believed that the presence of heartburn 1 or more times per week over the past 12 months is a clinical criterion for the diagnosis of GERD.
Causes of gastroesophageal disease
Single reflux of stomach contents into the esophagus can occur in almost all people. The disease is indicated when reflux becomes frequent and prolonged, accompanied by clinical symptoms and or damage to the esophageal mucosa. A number of factors play a role in the development of the disease.
The main role is played by dysfunction of the lower esophageal sphincter due to a decrease in its tone. Another reason may be an anatomical change in the esophagogastric junction that occurs when a hiatal hernia occurs. The occurrence of reflux is also facilitated by overfilling the stomach with food and impaired gastric motility. In addition, the following conditions may contribute to the development of this disease:
- diseases of the stomach and duodenum, such as chronic gastroduodenitis, peptic ulcers, gastro- and duodenostasis, which slow down gastric emptying and the movement of food masses into the intestines;
- disorders of autonomic nervous regulation;
- violation of the regime and quality of nutrition, overeating, abuse of fatty foods;
- excess body weight;
- taking certain medications;
- food allergies;
- smoking, excessive alcohol consumption;
- the presence of foci of chronic infection;
- stress;
- excessive physical activity;
- constipation;
- prolonged stay in an inclined position;
- pregnancy;
Complications
The result of aggressive contents entering the esophagus can be damage to the esophageal mucosa; due to regular exposure to an aggressive environment, an inflammatory process develops, which leads to the appearance of reflux esophagitis - inflammation of the lower parts of the esophagus. If left untreated, an ulcer may form - damage to the esophageal wall down to the submucosal layer. In severe cases there is a risk of bleeding. After the ulcer has healed, scars may remain that can cause stricture. The result of deterioration in the patency of the esophagus will be dysphagia in combination with heartburn, which only aggravates the situation.
One of the severe complications is Barrett's esophagus syndrome, in which the squamous cell epithelium in the esophagus is replaced by columnar gastric epithelium - metaplasia, and the likelihood of degeneration into cancer increases by 30-40 times.
Forms of gastroesophageal reflux disease (GERD)
According to modern concepts, there are three forms of the disease:
- endoscopically negative reflux disease, manifested by heartburn without erosive changes in the esophageal mucosa.
- endscopically positive (erosive) reflux disease with a progressive course and possible development of complications in the form of ulcers, bleeding, strictures.
- Barrett's esophagus is a condition in which irreversible changes occur in the lining of the esophagus, with a high risk of further malignant degeneration.
Clinical symptoms of GERD
Clinical symptoms of GERD are divided into esophageal and extraesophageal.
Esophageal symptoms
Heartburn “a burning sensation ascending from the stomach or lower chest to the neck.” With severe heartburn, this feeling may spread to the lateral chest and neck area, reaching the lower jaw. Heartburn may be accompanied by a feeling of “a warm wave rolling up to the throat” associated with the reflux of gastric contents. Heartburn may appear or worsen when bending forward, straining, lying down, or after eating. Standing, swallowing saliva, drinking a few sips of water, or taking antacids may reduce its intensity.
Regurgitation (or regurgitation) is the passive movement of stomach contents into the esophagus and then into the oral cavity. Often accompanied by a feeling of acidity or bitter taste in the mouth. It is provoked or aggravated by a horizontal position of the body, tilting the body, or an increase in intra-abdominal pressure. Regurgitation can lead to the reflux of contents into the pulmonary tract (aspiration) and lead to the development of laryngitis, cough, asthma and pneumonia. Belching is one of the variants of regurgitation. The main component is not gastric contents, but air. It can also be bitter or sour. Dysphagia, a feeling of food being “stuck” when swallowing and passing through the esophagus. At the initial stages of the disease, dysphagia occurs due to impaired motor function of the esophagus and is intermittent. In advanced cases with esophageal stricture, dysphagia becomes persistent.
Signs of the disease also include pain and discomfort in the epigastric region, pain in the chest, behind the sternum.
Extraesophageal manifestations of GERD
Symptoms of diseases of neighboring organs that can be caused by reflux:
- Cardiac symptoms (pain in the left half of the chest, heart rate abnormalities) can be triggered by reflux, hypermotility of the esophagus. Unlike angina, these pains have several features: they have a burning tint, have a retrosternal localization without irradiation, are caused by food intake, appear when changing body position and subside after taking drugs that reduce acidity.
- Pulmonary manifestations (cough, asthma attacks) are associated with vagal irritation and the appearance of bronchospasm or with the entry of stomach contents into the bronchi during regurgitation and the development of chronic bronchitis, repeated pneumonia, bronchial asthma and fibrosis of the lung tissue.
- ENT manifestations (hoarseness and loss of voice, dysphonia, sore throat, neck, hypersalivation) are associated with inflammation of the posterior wall of the larynx, pharynx, and the development of chronic laryngitis and pharyngitis.
- Dental manifestations (burning tongue, cheeks, impaired taste, caries) are caused by oxidation of saliva in the oral cavity, damage to the mucous membrane and demineralization of tooth enamel.
- Gastric (rapid saturation, fullness, distension of the stomach, nausea, bloating, flatulence.
Publications in the media
Gastroesophageal reflux disease (GERD) is the development of inflammatory lesions of the distal part of the esophagus and/or characteristic symptoms due to repeated reflux of gastric and/or duodenal contents into the esophagus. Endoscopically positive gastroesophageal reflux disease—endoscopic examinations reveal reflux esophagitis. Endoscopically negative gastroesophageal reflux disease - there are no endoscopic manifestations of esophagitis.
Frequency. Symptoms of GERD are detected in almost half of the adult population, endoscopic signs - in more than 10% of people who have undergone endoscopic examination. Berrett's esophagus develops in 20% of patients with reflux esophagitis (0.4% of the population).
Etiology • Surgical interventions on or near the esophageal opening of the diaphragm: •• Vagotomy •• Resection of the cardia of the stomach •• Esophagogastrostomy •• Gastric resection •• Gastrectomy • Hiatal hernia • Peptic ulcer of the stomach and duodenum • Pylorospasm or pyloroduodenal stenosis • Scleroderma • Exogenous intoxications: •• Smoking •• Alcohol • Pregnancy • Drugs that can reduce the tone of the LES: •• Anticholinergic drugs •• B2-adrenergic receptor agonists and theophylline •• Calcium channel blockers and nitrates • Insufficiency of the cardiac sphincter in obesity.
Pathogenesis. Gastroesophageal reflux due to LES dysfunction. Variants and causes of dysfunction of the LES: • reduced tone of the LES at rest • prolonged or repeated transient relaxation of the LES • transient increase in intragastric and intra-abdominal pressure (with flatulence, constipation, obesity, pyloric spasm) • delayed gastric emptying • changes in esophageal motility • dilatation of the stomach • weakening mechanical factors supporting the antireflux barrier (diaphragmatic crura and cardioesophageal angle of His) • short esophagus.
Pathological anatomy • Changes are localized mainly in the distal part of the esophagus: •• limited (single erosions and ulcers without a tendency to merge) •• diffuse •• confluent, circularly covering the mucous membrane of the esophagus • In mild cases - moderate hyperemia and edema of the mucous membrane • In severe cases course - erosions, ulcers, scars, shortening of the esophagus, columnar cell metaplasia of the epithelium (Berrett's ulcer), longitudinal wrinkling of the esophagus (Berrett's syndrome) • In 8–10% of cases, ulcers become malignant.
Classification of reflux esophagitis • Grade A - one (or more) mucosal lesion less than 5 mm, limited to the mucosal fold • Grade B - one (or more) mucosal lesion more than 5 mm, limited to the mucosal fold • Grade C - one (or more) mucosal lesions extending to 2 or more mucosal folds but occupying less than 75% of the esophageal circumference • Grade D—one (or more) mucosal lesions extending to 75% or more of the esophageal circumference.
Clinical picture • Heartburn is the most characteristic symptom (83% of patients), appears as a result of prolonged contact of acidic (pH <4) gastric contents with the mucous membrane of the esophagus. Heartburn increases with errors in diet, drinking alcohol, carbonated drinks, physical stress, bending over and in a horizontal position • Belching increases after eating, drinking carbonated drinks • Regurgitation of food increases with physical stress and in a position conducive to regurgitation • Dysphagia of an intermittent nature, which is associated with hypermotor dyskinesia of the esophagus • Pain in the epigastrium (in the projection of the xiphoid process) or behind the sternum - appears soon after eating, intensifies when bending the body, in a horizontal position • Less commonly, odynophagia occurs, a feeling of a lump in the throat when swallowing, pain in the ear and lower jaw, chest pain that can be provoked by physical activity • Extraesophageal manifestations of GERD - chronic cough, pneumonia, dysphonia, broncho-obstruction, dental erosion, etc. - are caused by the ingress of gastric contents onto neighboring organs and the vagal reflex between the esophagus and the lungs.
Diagnostics • X-ray examination lying on the back or in an upright position with a strong anterior tilt of the patient: reflux of barium sulfate into the distal parts of the esophagus, X-ray picture of esophagitis • Endoscopic examination with biopsy: reflux esophagitis of varying severity, prolapse of the gastric mucosa into the esophagus, true shortening esophagus, reflux of gastric and/or duodenal contents into the esophagus. In the case of endoscopically negative GERD, there are no signs of esophagitis • Esophagotonokymography (manometry) - decrease in expiratory sphincter pressure, destructuring of the sphincter, increase in the number of transient relaxations of the LES, decrease in the amplitude of peristaltic contractions of the thoracic esophagus • Daily pH-metry - the main method for diagnosing GERD and monitoring the effectiveness of treatment . It is recommended to evaluate: the total time of reduced acidity with pH<4 (the most significant criterion) in a standing and lying position; total number of refluxes per day; number of reflux lasting more than 5 minutes; duration of the longest reflux • Bilimetry is performed to identify alkaline (bile) reflux • Scintigraphy is indicated to identify motor-evacuation disorders of the esophagus • Omeprazole test - clinical symptoms of GERD are significantly reduced within 3-5 days of daily intake of 40 mg omeprazole • Bernstein test - if present GERD injection of 0.1 N HCl solution into the esophagus leads to the appearance of clinical symptoms, incl. and in the case of endoscopically negative GERD.
TREATMENT
Non-drug measures • Lifestyle changes •• Smoking cessation •• Normalization of body weight •• Raising the head end of the bed •• Avoid stress on the abdominal muscles, bending the body, wearing tight belts • It is undesirable to take drugs that reduce the tone of the LES (nitrates) , calcium antagonists, theophylline, progesterone, antidepressants) • Diet: limiting foods that increase gas formation, spicy, very hot or cold foods; avoid drinking alcohol, foods that reduce the tone of the LES (onions, garlic, pepper, coffee, chocolate, etc.); Avoid overeating, last meal no later than 3-4 hours before bedtime.
Drug therapy is carried out for at least 8–12 weeks, followed by maintenance therapy for 6–12 months • Antacids and alginates •• Usually prescribed 1.5–2 hours after meals and at night •• Effective in the treatment of moderate and infrequent symptoms • Prokinetics - domperidone, metoclopromide, cisapride 10 mg 4 times a day • Proton pump inhibitors (omeprazole, lansoprazole, rabeprazole) in regular or double dosage. In cases of severe esophagitis, they are usually required to be prescribed in combination with prokinetics.
Surgical treatment • Indications for surgical treatment •• Complications of GERD (esophageal strictures, recurrent bleeding, Berrett's esophagus) •• Ineffectiveness of drug therapy in young patients •• Combination of GERD with bronchial asthma, refractory to adequate antireflux therapy • Antireflux operations, such as Nissen fundoplication .
Complications • Benign stricture of the esophagus • Ulceration of the esophagus • Bleeding from latent to profuse from the ulcerated mucous membrane of the esophagus • Cicatricial changes in the esophagus, up to its shortening and stenosis • Laryngospasm • Pulmonary aspiration • Berrett's esophagus.
Abbreviations. GERD - gastroesophageal reflux disease; LES - lower esophageal sphincter
ICD-10 • K21 Gastroesophageal reflux
Appendix • Berrett's syndrome is a chronic peptic ulcer of the lower esophagus with an epithelium resembling that of the cardial mucosa; esophageal stricture, most often develops as a result of gastroesophageal reflux “Berretta's esophagus • Berretta's esophagus is a complication of GERD in the form of metaplasia of the mucous membrane of the distal esophagus into the small intestinal epithelium. Berrett's esophagus is considered a precancerous condition • Schatzki rings - membranes of the mucous membrane in the lower third of the esophagus, narrowing or closing its lumen, of unknown etiology; the disease is more common in patients with gastroesophageal reflux. Diagnosis - X-ray contrast study using barium sulfate confirms the diagnosis when constriction is detected in the lower part of the esophagus. Treatment is esophageal dilatation and antireflux surgery. The course is chronic, progressive. Synonym. Ring syndrome in the lower part of the esophagus. ICD-10. Q39.4 Esophageal membrane.
Variants of the course of reflux disease
The classic version of the disease is manifested by a combination of heartburn, the frequency and intensity of which coincides with the intensity of inflammation and regurgitation. More often, exacerbations occur 1-2 times a year, but a rarely recurrent variant of the course of the disease with exacerbations once every 2-3 years can also occur.
Complications of GERD include the erosive-ulcerative variant of the disease, because it causes bleeding and perforation of the esophagus. Narrowing of the esophagus is also a serious complication of GERD.
Features of GERD in young people
In young people (under 30 years of age), the clinical picture is dominated by pain and dysphagia. Moreover, the development of the disease is often combined with dysfunction of the autonomic nervous system.
Features of GERD in older people
In older people, on the contrary, an asymptomatic or low-symptomatic course of the disease often occurs. Among the complaints, heartburn predominates, which, as the disease progresses, is joined by pain when food passes through the esophagus. Sometimes such chest pain resembles pain due to coronary heart disease.
Features of GERD in obese people
For most people with increased body weight, complaints of dysphagia come to the fore; only a third have chest pain and less than a quarter experience heartburn. This is due to the fact that against the background of obesity, the motor-evacuation function of the stomach is disrupted and gastric secretion decreases.
Features of GERD in obese people
GERD and bronchial asthma have a pronounced mutually aggravating effect. Irritation of the esophageal mucosa by acidic gastric contents causes bronchospasm, and microaspiration of hydrochloric acid into the respiratory tract can further worsen the situation. The presence of bronchial asthma, in turn, leads to a decrease in the tone of the esophagus and a more frequent occurrence of regurgitation and heartburn. Therefore, such mutual aggravating influence requires more intensive treatment of both diseases.
Features of GERD in obese people
The identification of this combination of diseases as a separate variant is due to the fact that there is drug interaction between gastric secretion blockers and antiplatelet/anticoagulant drugs. As a result of this interaction, the drug effect may be reduced, which immediately worsens the course of coronary artery disease.
Diagnosis and treatment
To identify the disease, the clinical picture is assessed and some diagnostic procedures are performed: x-ray of the esophagus and stomach; daily pH monitoring inside the esophagus; esophagogastroscopy with biopsy histology and chromoscopy (detection of superficial disorders of the esophageal mucosa).
The main goal of treatment for GERD is to provide maximum relief from the symptoms of the disease, restore quality of life, eliminate reflux, heal the inflamed esophageal mucosa, and prevent complications and recurrences of the disease. Conservative therapy of GERD involves the patient's adherence to dietary nutrition and daily routine; as well as the use of special medications (antacids, H2 receptor blockers and proton pump inhibitors, prokinetics) to normalize the proper functioning of the gastrointestinal tract.
Information prepared for you by:
Molodkina Olesya Anatolyevna
— gastroenterologist, leading specialist of the clinic, Ph.D. Conducts receptions in the clinic building on Usachev.
Complications of GERD
The most common complication is erosive and ulcerative damage to the esophagus. In turn, the course of esophageal ulcers can be complicated by the development of bleeding, perforation of the ulcer, or the formation of a stricture (scar narrowing) of the esophagus.
In addition, the healing process of esophageal ulcers can occur by replacing the damaged area with intestinal-type epithelium, the so-called. “intestinal neoplasia”, i.e. lead to Barrett's esophagus. Barrett's esophagus is a disease in which a change in the structure of the epithelium of the esophagus occurs, and it is replaced by cells that are not typical for the mucous membrane of this section. There are several options for such replacement: transitional epithelium, gastric epithelium and intestinal epithelium. It is the latter option that is unfavorable from a prognostic point of view, since replacement with intestinal-type epithelium (“intestinal metaplasia”) is a risk factor for the development of esophageal cancer.
Diagnosis of gastroesophageal reflux disease
The main diagnosis of GERD is based on characteristic complaints that bother the patient. Additional examination methods are necessary to determine the stage of the disease, identify its complications and plan treatment.
Endoscopic examination of gastroesophageal disease
FGDS is the main method for confirming the presence of esophagitis, identifying or excluding hiatal hernia, combined lesions of the stomach and duodenum. A biopsy from the esophagus can confirm the presence of Barrett's esophagus and assess the risk of developing a malignant tumor.
Treatment of gastroesophageal reflux disease
Surgical and conservative treatment of gastroesophageal disease is possible based on the type of pathological transformations in the esophagus. Conservative treatment is aimed at eliminating the manifestations of the disease, preventing the reflux of stomach contents into the esophagus, treating inflammation and includes the use of medications and diet.
One of the important conditions for successful treatment is nutritional correction and lifestyle changes. In this case, both the nature of the food and its volume, and diet are important:
- It is necessary to avoid foods that irritate the esophagus or increase the formation of gas.
- It is necessary to adjust the amount of food, avoid eating before bed or at night.
- Quitting smoking, reducing body weight, and avoiding tight clothing, belts, and corsets that increase intra-abdominal pressure are very important.
Author's technique of modified fundoplication
During the operation, I use a Toupet partial fundoplication of 270 degrees, in which a cuff is created from the stomach wall to prevent the reflux of stomach contents into the esophagus. Thanks to the improved technique, for which a patent has been received, the functioning of the sphincter between the stomach and esophagus remains undisturbed, while the gag reflex and belching - protective functions - are also preserved.
The surgical intervention is performed using laparoscopy, using high-quality endoscopic equipment, which allows all manipulations to be performed with maximum precision, without the risk of damaging the structures located in this area: vessels, fascial spaces, vagus nerve. During laparoscopic surgery, I create a functional valve between the stomach and esophagus, which allows the patient to do without medications in the future. Due to the fact that all manipulations are performed through 3-4 small incisions, an excellent cosmetic result is guaranteed, since after healing, the marks from the incisions will become almost invisible.
When isolating the stomach and esophagus, I use the LigaSure device for dosed electrothermal tissue ligation, thanks to which the vessels can be “sealed” without damaging the surrounding tissues. The use of the latest generation of absorbable suture material and anti-adhesion barriers allows the operation to be performed quickly and efficiently.
If there are several diseases that require surgical treatment, in our clinic the patient can count on a simultaneous operation. Instead of several interventions, the interval between which should be 5-6 weeks, the person being operated on during one anesthesia can immediately get rid of a number of diseases.
Patients are discharged, as a rule, on days 1-3, and after 2-3 weeks they return to their usual activities. For the first two months you will have to adhere to a strict diet; over the next six months, the diet will gradually expand. In the future, a person who has undergone treatment in our clinic will be able to do without medications and without following a strict diet. We managed to reduce the number of relapses during the first year to 2%; five years after the operation, this figure does not exceed 4%.
I have performed more than 2000 operations on the stomach and esophagus, the accumulated experience is summarized in three monographs and more than 50 scientific publications, which can be found in professional peer-reviewed publications published in our country and abroad.