Pylorospasm in newborns
The basis of treatment is to reduce the number of regurgitations, normalize weight and prevent possible complications of pyloric spasm. The initial treatment for the disease is non-drug methods: they give the desired effect in 80% of cases. A complex effect on the body through diet, routine activities and medications ensures positive dynamics in 1-2 weeks.
Non-drug treatment
Treatment begins with diet and postural therapy. It is recommended to increase the number of feedings, reduce the size of a single serving, and feed the baby at the same time. An artificially fed newborn is prescribed adapted antireflux formulas. If excessive regurgitation or vomiting occurs, the baby should be fed additionally.
It is recommended to keep the baby upright for 30-40 minutes after feeding to prevent regurgitation. Positioning the newborn on his side or stomach when laying him down helps prevent aspiration of vomit. Additionally, it is recommended to eliminate the influence of stressful situations on the child: normalize sleep, create a comfortable and quiet environment at home. A relaxing abdominal massage and baths with a calming effect are effective.
Pharmacotherapy
If lifestyle changes do not improve and regurgitation does not stop, your doctor will prescribe medications. Treatment is carried out in a course until the child’s condition normalizes. Criteria for the effectiveness of pharmacotherapy include weight gain, relief of vomiting, and elimination of symptoms of hyperexcitability. Medicines used to treat pylorospasm in newborns:
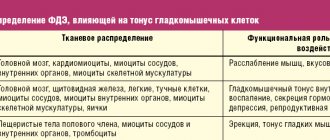
- Antispasmodics, muscle relaxants.
They are used to relax smooth muscles and normalize peristaltic contractions of the stomach. The spasm at the exit site of the stomach is eliminated, and food easily enters the small intestine. - Sedatives, adaptogens.
They help restore adequate functioning of the autonomic nodes in children with increased excitability. If they are ineffective, mild tranquilizers are used. - Vitamin complexes
. Preference is given to B vitamins: the drugs improve the conduction of nerve impulses and stabilize the activity of the ANS.
Hospital treatment
If dehydration and electrolyte disturbances develop, the newborn is treated in a hospital setting. Saline solutions are prescribed orally or parenterally: the choice of route of administration depends on the severity of the child’s condition. Surgical treatment is indicated for the development of complications when there is hypertrophy of muscle fibers.
What is regurgitation?
Regurgitation in infants is considered to be the spontaneous release of a small amount of just eaten food (milk or formula) into the baby’s mouth from the stomach.
Content:
1. Types of regurgitation |
00:56 (in video) 2. Physiological causes of regurgitation | 01:40 (in video) 3. Functional causes of regurgitation | 02:43 (in video) 4. Permissible frequency of regurgitation 05:13 (in video) 5. Until what age can regurgitation continue | 05:47 (in video) 6. Is it necessary to feed the baby after spitting up | 06:23 (in video) 7. Actions when spitting up | 07:11 (in video) 8. Congenital pathologies of the gastrointestinal tract, as a cause of regurgitation 9. Actions to prevent regurgitation Online consultation with a pediatrician (Breastfeeding Specialist)
Online consultation
During the consultation, you will be able to voice your problem, the doctor will clarify the situation, interpret the tests, answer your questions and give the necessary recommendations.
Disease prevention
Preventive measures for colic in children come down to monitoring the nutrition of the nursing mother and following other pediatrician’s instructions from the first days of life.
During the first year of a child's life, it is especially important to regularly visit a qualified pediatrician and follow all his instructions. Doctors at the pediatric medical department have the necessary qualifications and experience to treat the youngest patients. If your baby experiences anxiety, often cries and sleeps poorly, then consult a pediatrician at SM-Clinic.
Sources:
- N.I. Ursova. Infantile intestinal colic. Modern data // Issues of modern pediatrics, 2011, vol. 10, no. 2, pp. 125-131.
- I.A. Belyaeva. Intestinal colic in newborns and infants: from diagnostic issues to differentiated correction // Issues of modern pediatrics, 2011, v. 10, no. 2, pp. 137-140.
- E.S. Keshishyan, Doctor of Medical Sciences, Professor, E.K. Berdnikova. Functional intestinal colic. Tactics for their correction in young children // Medical Council, 2013, pp. 106-109.
Grek Elena Anatolyevna Clinic
Author of the article
Grek Elena Anatolyevna
Doctor of the highest qualification category
Specialty: gastroenterologist
Experience: 24 years
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Causes
There are primary and secondary forms of pylorospasm, which occur against the background of various pathologies.
Primary pylorospasm occurs as a result of:
- disturbances in the timely receipt of relaxing stimuli at the pyloric receptors, which occur when the nervous system malfunctions,
- vitamin deficiency (especially group B),
- severe fatigue (physical or mental),
- reflexively, with irritation in the area of the initial parts of the intestine or the area of the ileocecal angle (the place of transition of the small intestine to the large intestine),
- intoxication with nicotine or morphine,
- disturbances in the functioning of the autonomic nervous system (increased tone of the vagus nerve).
Secondary pyloropasm occurs when:
- peptic ulcer, especially when the ulcer is localized in the pyloric area,
- chronic gastritis, especially with high acidity,
- inflammation of the outlet of the stomach and the initial part of the intestine (pyloroduodenitis),
- polyposis of the stomach,
- diseases of the lower digestive tract - colitis, intestinal polyposis, Crohn's disease or chronic appendicitis,
- diseases of the biliary tract,
- adhesive process,
- inflammation in the pelvic area in women (a reflex spasm of the pylorus occurs due to the occurrence of pathological impulses).
Provoking factors for the development of pylorospasm are smoking, working in hazardous chemical industries, and taking certain medications.
Pylorospasm often occurs in infants as a result of difficult childbirth and prolonged hypoxia, immaturity or pathology of the nervous system. In adults, it usually occurs against an unfavorable painful background or when the body is exhausted.
Diagnosis of coronavirus in children
When the first signs characteristic of COVID-19 appear and/or when a child comes into contact with a person with confirmed coronavirus, you must call a pediatrician . He will examine the child, prescribe a PCR smear for coronavirus and a general blood test. Based on the test result, the pediatrician will give recommendations for caring for the child, prescribe treatment, and, if necessary, refer for consultation to other specialists (pulmonologist, otolaryngologist, ophthalmologist, etc.). If pneumonia is suspected, an X-ray or computed tomography scan of the lungs is performed.
To detect respiratory failure, you can use a pulse oximeter, a device that helps measure the concentration of oxygen in arterial blood. Pulse oximeter readings should not be lower than 96 units.
Acceptable frequency of regurgitation.
As a rule, they indicate a frequency of 6-8 times a day in small portions; you can also find data on regurgitation 2-5 times a day and a volume of ⅔ tablespoons. If the number of regurgitations increases, fever, and vomiting appear, contact your pediatrician. If weakness is added, this is a reason to call an ambulance.
Especially close attention is required when spitting up like a fountain. You need to offer the child water and carry it in a column. If the regurgitation was a one-time occurrence, there is no need to worry.
Signs of acute colic
Usually, during an attack, the child screams shrilly and unexpectedly , and shows extreme anxiety during feeding. Until the attack ends, it is almost impossible to calm the baby down - neither motion sickness, nor changing clothes, nor regurgitation help. Source: I.A. Belyaeva Intestinal colic in newborns and infants: from diagnostic issues to differentiated correction Issues of modern pediatrics, 2011, v. 10, no. 2, pp. 137-140. Lying in bed, the child tosses and turns from side to side, clenches his fists, and may blush or turn pale. You can see a “grimace of pain” on his face. The abdominal muscles become stiff and tense, which can be felt when touched. You can see bloating in the abdomen, the child is passing gas in large quantities.
Colic as a symptom
Although in medicine it is not customary to call colic either a disease or a symptom, they do occur against the background of other diseases. That is why it is imperative to show the child to the pediatrician to rule out:
- intestinal spasm;
- intestinal obstruction;
- flatulence;
- abnormal development of the gastrointestinal tract;
- disruption of the digestion process;
- lactase deficiency;
- allergies.
Helping babies with colic
It is important to organize feeding properly. The baby should not gasp for air; if he is offered a bottle, it must be held upside down at an angle of 45°. Sometimes intestinal colic can be caused by overeating. Consumption of large amounts of formula or milk in some cases provokes increased release of gases in the gastrointestinal tract. It is best to feed your baby more often, but in smaller portions.
It is recommended to periodically lay the baby on his stomach, this facilitates the passage of gases. A gas tube may be used to help relieve the child's condition. A light massage is recommended, for example, stroking the stomach in a clockwise circular motion. Warming helps a lot. Sometimes there is advice to use a heating pad. But it is much easier to iron a soft diaper and place it warm (but not hot) on your stomach. This reduces pain.
Why does my baby have colic? The reasons for this condition
The causes of colic in newborns are poorly understood, but they are thought to be related to the following:
- baby's intestinal spasms;
- air entering the esophagus during feeding or crying;
- allergies;
- lack of nutrition;
- digestive problems;
- lactose intolerance.
Foods that cause gas formation should be excluded from the child’s diet: chocolate, cocoa, coffee, legumes, fresh vegetables and fruits, sauerkraut, bananas, baked goods, muffins. A newborn baby may experience abdominal colic if a nursing mother consumes the listed products. Source: N.I. Ursova Infantile intestinal colic. Modern data // Issues of modern pediatrics, 2011, v. 10, no. 2, p. 125-131
How to understand that a baby has colic: symptoms of intestinal problems
Colic in children can be expressed in bouts of crying (they often occur in the evening), tension and bloating in the abdomen, tightening of the knees, arching of the whole body, redness of the face, and refusal to eat. Usually, with colic, a child does not calm down if you pick him up and rock him to sleep. Breastfeeding can have an effect, but not for long, usually after the end of milk intake, the baby continues to cry.
Colic can also manifest itself as:
- anxiety for no reason;
- difficulty with stool;
- sharp cries during feeding;
- flatulence.
Often colic is accompanied by acne, similar to teenage ones. This is due to the fact that during the period of colic, the mother’s hormones received in the womb leave the child’s body. Hormonal balance is disrupted.