- home
- general surgery
- Gastroesophageal reflux disease
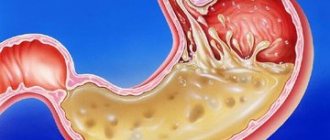
Gastroesophageal reflux disease (GERD) is a chronic disease of the digestive system in which, as a result of spontaneous or regularly repeated reflux of gastric or duodenal contents into the esophagus, an inflammatory process of the wall of its distal section develops. This disease is the most common among diseases of the digestive system; it is diagnosed in a third of the adult population.
The cause of reflux is most often the failure of the sphincter located at the border of the stomach and esophagus. Also, reverse reflux of contents can occur when the motor function of the upper part of the digestive tract is impaired. Unfavorable factors influencing the development of the disease are smoking, excess weight, diaphragmatic hernia, taking certain medications, and stress.
Symptoms of gastroesophageal reflux disease
The main symptom of the disease is persistent heartburn, its occurrence does not depend on food intake or physical activity. It can occur on an empty stomach or after eating, during active movements, especially when bending the body, and even in a lying position. Belching and regurgitation of food often occurs.
Pain may appear - bursting or burning, localized in the epigastrium, behind the sternum and even in the left hypochondrium; often the pain intensifies after eating or physical activity, and nausea and vomiting may occur. In advanced cases, difficulties with swallowing appear - dysphagia; The cause of this disorder may be impaired motility or narrowing of the lumen of the esophagus - stricture. Also, the symptoms of GERD can be supplemented by drooling during sleep, and hoarseness is possible after waking up.
Treatment of GERD and hiatal hernia
Intestinal obstruction: a practical guide for doctors
Definition
A condition in which the passage of contents in the gastrointestinal tract is slow, difficult, or completely stopped.
Frequency
Occurs in approximately 3% of palliative patients. Most often in ovarian cancer (25‒40%), colorectal cancer (10‒15%), cancer of the stomach, bile ducts, pancreas, endometrium, bladder, prostate.
Classification
According to the level of occurrence , it is clinically advisable to focus on four levels of obstruction of the gastrointestinal tract:
upper (proximal):
- esophageal, usually at the level of the transition from the esophagus to the stomach;
- at the level of the gastric outlet or proximal small intestine;
lower (distal):
- obstruction of the distal small intestine;
- obstruction of the large intestine.
According to etiology , at any level, obstruction can be functional (dynamic, impaired peristalsis), or mechanical (organic), or combined.
According to the degree of disruption of the passage of intestinal contents - complete or partial.
According to the clinical course - transient (acute) or persistent (chronic).
Patients may experience recurrent episodes of obstruction that resolve after a few days of GI rest. The frequency and duration of episodes of obstruction tend to increase, and eventually it becomes complete and irreversible. The prognosis is usually unfavorable, with an average life expectancy of 1–3 months.
Causes
Oncological diseases:
- a tumor in the abdominal cavity compresses the intestines and nerve plexuses from the outside - functional obstruction (retroperitoneal disease → visceral neuropathy);
- tumor inside the intestinal lumen (mechanical obstruction);
- tumor invasion of the nerve plexus and the occurrence of pseudo-obstruction (dynamic obstruction, often in ovarian cancer).
Consequences of treatment for cancer or its symptoms:
- adhesive process;
- radiation damage to the small intestine - post-radiation ischemic fibrosis;
- chemotherapy (the neurotoxicity of drugs can lead to the development of fecal stagnation in the upper intestines);
- treatment with opioids and, to a lesser extent, other drugs that lead to inhibition of gastrointestinal motility.
Not related to cancer:
- decreased intestinal tone, for example: coprostasis, electrolyte imbalance;
- constipation, fecal blockages against the background of cachexia, asthenia, physical inactivity;
- diverticulitis, infarction of the intestinal wall, hernias, adhesions, pancreatitis.
Pathophysiology
As a result of obstruction,:
- accumulation of swallowed liquid and saliva, gastric, pancreatic and bile secretions inside the intestine above the site of obstruction;
- impaired absorption of sodium ions and water through the intestinal wall due to intestinal distension and the associated entry of sodium ions and water into the intestinal lumen;
- increased intraintestinal pressure, which leads to colic, pain, nausea and vomiting.
Clinical features
The main symptoms depend on the level, etiology, severity and duration of obstruction.
Mechanical esophageal obstruction , as a rule, manifests first with dysphagia when swallowing solid foods, then dysphagia when swallowing liquids.
Obstruction at the level of the pylorus of the stomach or proximal parts of the small intestine is characterized by large losses of gastric, pancreatic secretions, bile due to profuse repeated vomiting that is painful for the patient and the rapid development of water and electrolyte disorders (hypohydration, metabolic alkalosis, hypokalemia, hypochloremia, hyponatremia). In this case, as a rule, there is no pronounced bloating, the passage of gases and the presence of stools persist for some time. Even in the absence of oral nutrition, the stomach requires emptying from incoming saliva (~1500 ml/24 hours) and secreted gastric juice (~1500 ml/24 hours). That is, if the patient vomits less than 2-3 liters per day, it means that some part of the food passes beyond the level of obstruction.
A feature of obstruction of the distal parts of the small intestine, as well as obstruction of the large intestine, is the erasure of clinical symptoms in the early stages of the development of the disease and, at the same time, a greater opportunity for conservative measures. In this case, signs of impaired passage through the intestines come to the fore: pain, severe bloating, vomiting is less common, and endotoxicosis quickly progresses. The likelihood of developing infectious complications is much higher with low than with high obstruction.
Abdominal pain in the presence of a malignant neoplasm is a constant and early sign of obstruction (90% of cases):
- occurs from compression by a tumor, stretching of the enlarged liver capsule or increased intra-abdominal pressure (ascites, massive tumor, etc.);
- severe constant pain may be a signal of intestinal strangulation;
- acute paroxysmal pain with intervals of relative relief is possible;
- the higher the level of obstruction, the more intense the pain;
- usually relieved by opioids.
Colic is often found in mechanical obstruction (75%) and is practically absent in dynamic obstruction. Episodes of colic are accompanied by an audible rumbling sound. They are poorly anesthetized by opioids, but are reduced or stopped by antispasmodic drugs.
Vomit . The higher the level of obstruction, the more severe the vomiting. In the later period, it becomes indomitable, the vomit takes on the appearance and smell of intestinal contents.
Stretching is an intermittent symptom (more common with low obstruction), accompanied by a tympanic sound when percussing the abdomen.
Intestinal sounds may be completely absent with functional obstruction, and with mechanical obstruction they may be active and clearly distinguishable (rumbling in the abdomen). The "sound of a falling drop" is rare.
Retention of stool and gases is a pathognomonic sign of intestinal obstruction, an early symptom of low-grade obstruction. If its character is high at the beginning, especially under the influence of therapeutic measures, there may be multiple stools, often liquid due to the “filter” effect - the passage of liquid and retention of the dense part of the intestinal contents above the area of obstruction and bowel movement located below the area of obstruction. It is necessary to be as careful as possible and not rush to regard this symptom as diarrhea (thin, watery discharge against the background of a corresponding diagnosis, for example, carcinomatosis).
Survey
Based on anamnesis and clinical examination of the abdomen, surgical protocols. Additional examinations are carried out in case of planning/possibility of surgical treatment (computed tomography, endoscopy). X-ray examination of the intestine in patients with progressive obstruction is indicated if palliative surgery is planned to relieve symptoms of obstruction and to differentiate between mechanical obstruction and severe constipation (Table 1).
Table 2 presents symptoms that allow for differential diagnosis of small and large intestinal obstruction.
Treatment
Depends on the type of obstruction, the severity of the situation (for example, complications of peritonitis), prognosis (the trajectory and stage of the disease must be taken into account) and patient preferences. Treatment should be determined in accordance with the decisions of the multidisciplinary team, the patient and his family. Intestinal obstruction in the palliative setting is rarely acute.
Drug treatment of obstruction
Medical treatment should focus primarily on relieving pain, nausea, and vomiting and, if possible, resolving partial obstruction. Administration of drugs is carried out, as a rule, through continuous subcutaneous infusion (CSI) or subcutaneously (SC). The stepwise diagram presented below (Scheme 1) reflects the general approach to treatment. Dosages of medications may need to be titrated over several days to achieve optimal effect.
Stage I. Possible functional obstruction (no colic, peristalsis disturbances):
- metoclopramide/Cerucal 30-40 mg/24 hours via NPI and 10 mg subcutaneously if necessary;
- if there is an effect, increase the dose up to 100 mg/24 hours.
Stage II. Possible mechanical obstruction
- hyoscine butylbromide/Neoscapan, Spanil, Buscopan 60-120 mg/24 hours via NPI and 20 mg subcutaneously if necessary, usually the maximum dose is 300 mg/24 hours;
- it is possible to use levomepromazine/Tizercin 6.25‒25 mg/24 hours subcutaneously (titration);
- instead of levomepromazine, haloperidol 2.5-5 mg/24 hours can be prescribed via NPI and 1 mg subcutaneously if necessary;
- if levomepromazine has a pronounced sedative effect, olanzapine/Zyprexa is prescribed (difficulty in prescribing! neuroleptic!) 1.25-2.5 mg subcutaneously at night.
Stage III (when hyoscine butyl bromide is not sufficient to control vomiting, is not available, or provides more rapid relief):
- octreotide/Octretex (somatostatin analogue and antisecretory agent);
- in the presence of colic, it is used together with hyoscine butyl bromide;
- in the absence of colic, they replace hyoscine butyl bromide in the following dosages: 100 mcg (emergency s.c.) or NPI (500 mcg/24 hours), maximum dose 1000 mcg/24 hours.
If vomiting continues, it is necessary to limit the intake of food through the mouth: nasogastric suction or venting/unloading gastrostomy may be necessary.
Relief of individual symptoms (see also Appendix 1)
Reduction of edema of the intestinal wall and peritumoral edema - dexamethasone: doses are selected individually at the rate of 6-8 mg 1-3 times per day subcutaneously or intravenously (8-16 mg subcutaneously or intravenously in the first half of the day). It also acts as a co-analgesic and antiemetic. If there is a positive effect, treatment can be continued orally. If ineffective within three days, cancel. But if the patient has been receiving dexamethasone for a longer period of time, discontinuation should be done gradually, reducing the dose by 2 mg every three days.
Stimulation of gastrointestinal motility - metoclopramide 30-120 mg/24 hours NPI or in divided doses (DR) subcutaneously every 4-6 hours. Monitor the clinic: if colic worsens - cancel.
Nausea and vomiting - haloperidol 3-5 mg/24 hours NPI or DR; levomepromazine 6.25‒25 mg/24 h NPI or DR; ondansetron 8‒16 mg/24 h NPI or DR. Nausea is also relieved by subcutaneous hydration in excess of 500 ml/day (with care not to increase abdominal distension and bloating). Antisecretory drugs such as octreotide and dexamethasone (due to their anti-inflammatory effect) will also help resolve problems with nausea and vomiting.
Colic - opioids NPI, DR, buccal, sublingual or transdermal for proper absorption of painkillers, which cannot be provided by oral administration; titrate the dose. For persistent colic, despite taking opioids, anticholinergic drugs are prescribed: hyoscine butyl bromide (Neoscapan, Buscopan, Spanil) 40–100 mg/24 h NPI or DR). The drugs reduce intestinal motility, resulting in decreased fluid secretion and smooth muscle peristalsis. The dose of anticholinergic drugs should be reduced after 1–2 days of use; if there is no stool, in this case you should consider surgery. If this is impossible/inappropriate, hyoscine butylbromide is prescribed po 10 mg 4 times a day.
Chronic pain - opioids NPI, DR, buccal, sublingual or transdermal to ensure proper absorption of pain medications; titrate the dose.
Constipation - laxatives: petroleum jelly (the safest drug, from 1 to 5 teaspoons from 1 to 4 times a day); docusate/Norgalax (incompatible with vaseline oil) - only if rectal use is possible; lactulose/Duphalac - titrate the dose with caution, starting from 3-5 ml (promotes an increase in osmotic pressure and, as a result, an increase in the volume of intestinal contents); cleansing enemas with caution (preferably oil, small volume 100-200 ml); manual release of the rectum (with anesthesia).
Stenting/ostomy
They are used in cases where conservative treatment of gastrointestinal obstruction in patients with a prognosis of life of more than two months within 48–72 hours does not bring results.
Esophageal obstruction
Stenting and bougienage are used to relieve dysphagia in patients with esophageal or proximal gastric cancer. Endoscopically inserted stents quite effectively alleviate the symptoms of obstruction, saving the patient from having an ostomy. Most patients experience rapid relief. Mortality from this procedure is low, but the complication rate is relatively high. Possible complications: chest pain requiring additional anesthesia - usually resolves within 2-3 days, bleeding, esophageal perforation, fistula formation, gastroesophageal reflux, aspiration, compression of the respiratory tract.
Important
A nasogastric tube provides decompression and can help control nausea, but prolonged use should be avoided.
Duodenal pyloric obstruction
Stents/bougies/probes . Contraindications for stenting are the patient’s condition, intestinal perforation with peritonitis, stenosis of the lower third of the rectum (can cause tenesmus, incontinence, risks of stent migration), multiple areas of obstruction below the stenting site, peritoneal carcinomatosis. The most common complications of stenting in this part of the gastrointestinal tract: biliary tract obstruction (50%), stent migration (up to 14%), repeated obstruction (up to 10%), intestinal perforation (from the stent guide), pressure necrosis, balloon dilatation, etc. ( up to 6%), bleeding (5%), functional disorders of the stent (inability to pass the narrowing site, problems with opening, up to 4%), tumor invasion (2%), fistula (1%). The mortality rate of the procedure is up to 4%.
Gastrojejunostomy . Provides longer survival and a lower risk of need for reintervention than stenting in patients with malignant gastric outlet obstruction. However, in the short term, stenting is more favorable.
Important: Gastrojejunostomy is indicated for long-term prognosis.
Percutaneous gastrostomy in patients with gastroduodenal or proximal small bowel obstruction and persistent vomiting can relieve symptoms and is performed in cases where best possible medical treatment has failed. This will avoid the need for prolonged use of a nasogastric tube, decompress the intestines and relieve nausea and vomiting. Patients can even enjoy eating and drinking while evacuating stomach contents through a gastrostomy tube.
Absolute contraindications for gastrostomy placement: portal hypertension, massive ascites, predisposition to bleeding, active gastric ulcer; relative: multiple previous surgical interventions in the upper abdomen, colonostomy, infected abdominal injuries.
Complications of percutaneous gastrostomy: bleeding from the peristome or intestinal wall, retroperitoneal/gastric erosion or ulceration, perforation or peritonitis, fistula, stent migration (can cause gastric outlet obstruction, pancreatitis, cholangitis, catheter obstruction or torsion, contact of gastric contents with the skin).
Obstruction of the distal small/large intestine
Research data show that the survival rate of patients after stenting and other surgical interventions for obstruction of this section of the gastrointestinal tract is 56%, and life expectancy does not exceed 60 days. Surgical anastomoses with bypass can alleviate the patient’s condition and improve the quality of life in recent days. These procedures are performed when drug treatment is ineffective and the expected survival time is several weeks or months.
Surgery such as palliative resection, anastomosis, or colostomy is effective for patients who meet the following criteria:
- there is a single discrete mechanical obstruction caused by postoperative adhesions or an isolated tumor, such as terminal ileal carcinoid;
- the patient’s general condition is satisfactory (that is, the patient is independent and active), life expectancy is more than 2 months;
- the patient agrees to surgery.
Additional important indicators of the condition indicating in favor of surgical treatment: absence of ascites due to carcinomatosis; large palpable tumor in the abdominal cavity; distant metastases, especially in the lungs; pleural effusion or evidence of liver and kidney failure.
Complications after surgical interventions are quite high: fecal fistula (7‒10%); repeated obstruction (30‒40%); seam divergence; sepsis.
Useful tips
In all cases: careful oral care, ice for resorption.
Some patients, carers or staff are concerned about restricting oral caloric intake: this may require discussion.
If the obstruction is partial, dietary changes are recommended, for example:
- fractional consumption of liquid or puree foods and/or specialized products in small volumes and low fiber content;
- avoiding carbonated drinks that fill the stomach with gas;
- sometimes the patient chooses to install a long-term nasogastric tube or consider a venting/unloading gastrostomy to be able to take food by mouth;
- Parenteral nutrition is generally of no benefit in patients with limited anticancer treatment options or severe general conditions.
Most patients require subcutaneous infusions of medications because oral administration and absorption of medications is ineffective.
It is necessary to regularly review the treatment regimen, as symptoms may change and resolve spontaneously.
Thank you for your help in preparing the materials:
Kravchenko T.V. (Chief Physician of the State Budgetary Healthcare Institution, Center for Emergency Medicine, Department of Healthcare),
Gurkin S.P. (Deputy Chief Physician for the organization of inpatient care of the State Budgetary Healthcare Institution of the Central Clinical Hospital of the Department of Healthcare),
Ibragimova A. N. (Head of the branch of the First Moscow Hospice named after Vera Millionshchikova, State Budgetary Healthcare Institution of the Center for Emergency Medicine of the Department of Healthcare).
List of sources:
- Abuzarova G.R. Nevzorova D.V. Pain management in palliative care. Practical guide for the doctor. Moscow, 2022.
- Chronic pain syndrome (CPS) in adult patients in need of palliative care. 2016, ICD 10: R52.1/ R52.2.
- Intestinal obstruction: classification, pathogenesis, clinical picture, differential diagnosis, treatment, complications. https://studopedia.org/8-169456.html.
- Clinical recommendations: acute intestinal obstruction of tumor etiology. Moscow, 2014.
- National clinical guidelines “Acute non-tumor intestinal obstruction”. Adopted at the XII Congress of Surgeons of Russia // “Current Issues in Surgery” (Rostov-on-Don, October 7-9, 2015).
- Introducing Palliative Care Fifth Edition. Editors Twycross R., Wilcock A., 2016.
- Jang SH, Lee H., Min BH, Kim SM, Kim HS, Carriere KC, Min YW, Lee JH, Kim JJ Palliative gastrojejunostomy versus endoscopic stent placement for gastric outlet obstruction in patients with unresectable gastric cancer: a propensity score-matched analysis . Surg Endosc. 2022 Oct;31(10):4217-4223. doi:10.1007/s00464-017-5480-6. Epub 2022 Mar.
- Hospice and Palliative Care Training for Physicians. Unipac Self-Study Program, 2008.
- Lanarkshire Palliative Care Guidelines, 2012.
- ProCare Hospice Care. Hospice Medication Utilization Guidelines. Eds. S. Shah, M. Madison.
- Tradounsky G. Palliation of gastrointestinal obstruction Canadian Family Physician // Le Médecin de famille canadien, 2012. Vol 58: 648‒652.
You can download the practical guide “Intestinal obstruction in palliative care” in pdf format here:
Practical guide_Intestinal obstruction.pdf
Complications
The result of aggressive contents entering the esophagus can be damage to the esophageal mucosa; due to regular exposure to an aggressive environment, an inflammatory process develops, which leads to the appearance of reflux esophagitis - inflammation of the lower parts of the esophagus. If left untreated, an ulcer may form - damage to the esophageal wall down to the submucosal layer. In severe cases there is a risk of bleeding. After the ulcer has healed, scars may remain that can cause stricture. The result of deterioration in the patency of the esophagus will be dysphagia in combination with heartburn, which only aggravates the situation.
One of the severe complications is Barrett's esophagus syndrome, in which the squamous cell epithelium in the esophagus is replaced by columnar gastric epithelium - metaplasia, and the likelihood of degeneration into cancer increases by 30-40 times.
Preventive measures
Proper nutrition as a preventive measure for esophageal cancer.
Preventive measures include the following:
- It is important to constantly see a doctor for diseases such as barretta and ahalakhia.
- Watch your diet. It is harmful to eat excessively hot or cold food. Minimize the consumption of pickled foods and hot spices. A lack of vitamins can also affect the condition of the digestive organs, including the esophagus.
- Do not smoke or abuse alcoholic beverages.
- Drink purified water.
- Eat more vegetables and fruits, which are high in fiber.
- Treat your teeth in a timely manner, take care of your oral cavity - food should enter the esophagus well chewed.
Diagnostics
- The main method for diagnosing gastroesophageal reflux disease is fibrogastroscopy, which allows assessing the condition of the mucosa, the degree of changes in the wall of the esophagus, in the stomach and duodenum. During the procedure, you can perform a biopsy - take particles of pathologically altered tissue for histological examination; Based on this analysis, treatment is planned.
- Another effective method is radiography, during which a stricture, diaphragmatic hernia, or esophageal ulcer can be detected.
- To determine the level of gastric secretion and the presence of reflux, daily pH measurements are performed.
Depending on the course of the disease, the patient may be prescribed other examination methods: esophageal manometry, ultrasound, ECG, and may need to consult an otolaryngologist.
For a free written consultation, in order to identify the hiatal hernia and determine the degree of damage to the esophagus, as well as choosing the correct surgical treatment tactics, you can send me a complete description of gastroscopy, x-ray of the esophagus and stomach with barium for the hiatus, preferably an ultrasound of the abdominal organs, age and main complaints must be indicated. In rare cases, if there is a discrepancy between complaints, X-ray data and FGS, it is necessary to perform daily pH measurements and manometry of the esophagus. Then I will be able to give a more accurate answer to your situation.
Consequences of intestinal obstruction
The development of obstruction triggers a cascade of pathological processes that affect the body systemically. With tumor obturation, the onset, as a rule, is blurred due to incomplete occlusion of the intestinal lumen, but as the tumor grows, the situation worsens. Acute obstruction, as a rule, develops due to complete obstruction of dense feces in the area of the intestine narrowed by the tumor.
In the first time after the development of obstruction, there is an increase in intestinal peristalsis. It's as if he wants to overcome an obstacle. As intestinal contents accumulate, the intestinal wall becomes overstretched, water-electrolyte and metabolic disturbances occur, motor function sharply weakens, and then intestinal paralysis occurs.
At the second stage, disturbances in the secretory-resorptive activity of the intestine and disturbances in parietal digestion develop, the enzymatic activity of enterocytes is blocked, as they are rejected, and the regenerative activity of the crypts is first inhibited and then completely stopped.
Under such conditions, the activity of intestinal bacteria and the so-called symbiont digestion is activated. It is not physiological and is inferior in efficiency to normal, parietal digestion. As a result, rotting and fermentation occurs, as well as the accumulation of a large number of products of incomplete breakdown of proteins, some of which have a toxic effect. [9]
As the process progresses, the immune defense mechanisms are disrupted, which leads to the active proliferation of anaerobic bacteria that secrete exo- and endotoxins. They act systemically on the body - they disrupt tissue microcirculation, lead to central nervous system disorder, and disrupt cellular metabolism. Due to these effects, the permeability of the intestinal wall to bacteria increases, and they can spread into the abdominal cavity, blood and lymph flow, causing peritonitis and even sepsis.
Water and electrolyte disturbances also progress. Due to disruption of the intestine, increased filtration of fluid occurs; it is not absorbed back and accumulates in the afferent loop of the intestine. Under normal conditions, about 10 liters of liquid enter the gastrointestinal tract per day (including food, drink, saliva and secretions of the digestive glands). About 8-9 liters should be absorbed back, but this does not happen due to impaired reabsorption. Fluid accumulates in the adductor section of the intestine, causing it to expand. This, in turn, leads to reflex vomiting, which further worsens dehydration. Against this background, electrolyte disturbances quickly develop, which ultimately lead to renal and heart failure. [1.10]
Book a consultation 24 hours a day
+7+7+78
Treatment
The goal of treatment is to relieve the symptoms of GERD and prevent the development of complications. For this purpose, medications are prescribed to neutralize the contents of the stomach or reduce its acidity. When taking medications, the patient also needs to constantly follow a diet; in case of obesity, weight normalization is recommended.
However, drug therapy is effective as long as the patient takes the medication; symptoms usually return after the end of the course of treatment. It should also be taken into account that long-term use of drugs that affect the acidity of gastric juice increases the risk of malignancy; suppression of secretion prevents the digestion of food, which entails a number of other disorders.
If drug therapy is ineffective, patients are recommended to undergo surgery. The indication for surgical treatment of GERD is the presence of complications, hiatal hernia, the appearance of strictures, ulcers, Barrett's esophagus, etc., as well as the presence of extra-esophageal symptoms: hoarseness, chest pain.
The purpose of surgery for GERD is to create a mechanism that prevents the reflux of stomach contents into the esophagus. Most domestic surgeons perform Nissen fundoplication. During the intervention, the fundus of the stomach is wrapped around the esophagus 360 degrees; This creates a cuff that prevents reflux.
However, this technique has its drawbacks. For example, the formation of a valve in the cardia zone leads to the fact that regurgitation or vomiting - natural protective mechanisms - is lost. With large portions during meals or when drinking carbonated drinks, it becomes impossible to remove them through the cardia, the stomach swells, pain and a feeling of heaviness appear. Often, 1-2 years after Nissen surgery, a relapse occurs due to cuff slippage.
Characteristic symptoms of a hiatal hernia
With a hiatal hernia, the valve-pressure mechanism is disrupted, which, as a rule, leads to pathological reflux of acidic stomach contents into the esophagus - gastroesophageal (gastroesophageal) reflux occurs. Both with paraesophageal hernia, which occurs in only 5% of patients, and with the most common type, diagnosed in 90% of cases - axial or sliding hiatal hernia, the first symptoms are most often associated with the reflux of gastric contents into the esophagus.
The disease may be asymptomatic if the function of the valve-pressure mechanism remains adequate. The absence of typical symptoms of a hiatal hernia is observed in half of the patients in the early stages of the disease. But in the absence of adequate treatment, clinical manifestations become more expressive, and complications develop over time. What are the main symptoms of a hiatal hernia?
There are “esophageal” manifestations of the disease, which include:
- Heartburn is persistent and painful, caused by the entry of acidic contents from the stomach into the esophagus; it can occur after eating or on an empty stomach, regardless of body position, intensifying with bending or physical activity.
- Belching - with sour or bitter contents, and even air, which occurs more often in an upright position and when bending over, after which a feeling of relief appears.
- Regurgitation—regurgitation—occurs after eating and can occur even in a lying position, with no previous nausea.
- Dysphagia, a feeling of “lump in the throat”, is a characteristic sign of hiatal hernia, meaning disturbances that occur during the passage of food through the esophagus; Mostly there is a feeling of a lump in the throat and pain when passing not only solid food, but also liquid.
- Pain - in the upper abdomen, behind the sternum, in the left hypochondrium, which can radiate to the shoulder blade or shoulder. Most often, the pain is associated with eating and intensifies in a horizontal position. Painful sensations can range from discomfort to bursting or burning pain, with a feeling of lack of air, and may resemble angina pectoris.
- Vomiting, nausea
“Extraesophageal” manifestations of a hiatal hernia include:
- Reflex shortness of breath
- Reflex angina, feeling of heart rhythm disturbance
- Cough, hoarseness
In fixed paraesophageal hernias, unlike sliding esophageal hernias, symptoms are constantly present; treatment in this case requires immediate treatment, since such hernias are more often susceptible to strangulation.
With a large hernia of the hiatal hernia, symptoms may be supplemented by shortness of breath due to compression of the organs and the vagus nerve. Long-lasting, frequent hiccups occur when the diaphragm spasms. Drooling, coughing, episodes of respiratory arrest during sleep, and hoarseness in the morning complete the picture of the disease.
Author's technique of modified fundoplication
During the operation, I use a Toupet partial fundoplication of 270 degrees, in which a cuff is created from the stomach wall to prevent the reflux of stomach contents into the esophagus. Thanks to the improved technique, for which a patent has been received, the functioning of the sphincter between the stomach and esophagus remains undisturbed, while the gag reflex and belching - protective functions - are also preserved.
The surgical intervention is performed using laparoscopy, using high-quality endoscopic equipment, which allows all manipulations to be performed with maximum precision, without the risk of damaging the structures located in this area: vessels, fascial spaces, vagus nerve. During laparoscopic surgery, I create a functional valve between the stomach and esophagus, which allows the patient to do without medications in the future. Due to the fact that all manipulations are performed through 3-4 small incisions, an excellent cosmetic result is guaranteed, since after healing, the marks from the incisions will become almost invisible.
When isolating the stomach and esophagus, I use the LigaSure device for dosed electrothermal tissue ligation, thanks to which the vessels can be “sealed” without damaging the surrounding tissues. The use of the latest generation of absorbable suture material and anti-adhesion barriers allows the operation to be performed quickly and efficiently.
If there are several diseases that require surgical treatment, in our clinic the patient can count on a simultaneous operation. Instead of several interventions, the interval between which should be 5-6 weeks, the person being operated on during one anesthesia can immediately get rid of a number of diseases.
Patients are discharged, as a rule, on days 1-3, and after 2-3 weeks they return to their usual activities. For the first two months you will have to adhere to a strict diet; over the next six months, the diet will gradually expand. In the future, a person who has undergone treatment in our clinic will be able to do without medications and without following a strict diet. We managed to reduce the number of relapses during the first year to 2%; five years after the operation, this figure does not exceed 4%.
I have performed more than 2000 operations on the stomach and esophagus, the accumulated experience is summarized in three monographs and more than 50 scientific publications, which can be found in professional peer-reviewed publications published in our country and abroad.