Pathophysiology
The content of the article
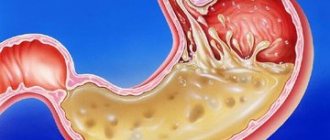
Under normal conditions (in a healthy person), the contents of the gastric juice with high acidity periodically enter the esophagus, but internal protective mechanisms either reduce the amount of acid secreted to a minimum or remove the acid, which is quickly removed by “cleansing” the esophagus. Therefore, symptoms of acid irritation of the esophagus are not felt or are minimal.
Mechanisms that protect the esophagus from stomach acid include the lower esophageal sphincter (sphincter) and normal esophageal motility (motility). When these mechanisms are disrupted, reflux occurs and symptoms of GERD occur.
Gastroesophageal reflux
How is the operation performed using a modified technique?
During the operation, a symmetrical cuff is formed from the upper part of the stomach, covering the esophagus at 270°. The anterior right side of the esophagus remains free; The cuff created in this way strengthens the lower esophageal sphincter and prevents the backflow of stomach contents. In the presence of a hiatal hernia, the lower part of the esophagus and the upper third of the stomach are first separated from the adhesions and returned to their natural position. The diaphragmatic hole is sutured to normal size. To prevent relapse and perform diaphragmocruroplasty, I use mesh implants, which reduces the risk of recurrence of the disease from 65% to 1%.
Surgery for reflux esophagitis is performed through laparoscopic access: all manipulations are performed through several small punctures on the anterior abdominal wall. In the future, the puncture marks become almost invisible. The operation is performed using endoscopic equipment equipped with a miniature video camera, which allows all manipulations to be carried out under visual control as accurately as possible. Since important structures (vagus nerve, blood vessels) are located in the surgical area, there is virtually no risk of damage to them.
During the operation, when isolating the esophagus and stomach, I use a dosed tissue ligation device LigaSure (USA), which is capable of “sealing” vessels without the risk of damage to surrounding tissues, as well as the development of bleeding. At the same time, the duration of the operation is reduced. The use of modern suture material promotes rapid recovery.
Etiology: a new approach
The prevailing theory (since 1935) is that GERD occurs when acidic stomach acid spills from the stomach into the esophagus, chemically and mechanically damaging the lining of the esophagus, causing burns, irritation, erosions, and ultimately more serious consequences. However, this traditional theory of chemical and mechanical irritation of the esophageal mucosa cannot fully explain many things associated with the onset, symptoms and course of GERD.
There are now reports that GERD may be an immune-mediated inflammatory disease caused by immune reactions rather than direct chemical damage to the lining of the esophagus by gastric juices. The hypothesis about the etiology of immune GERD is confirmed by one of the clinical studies conducted in the USA. The study results were published in the Journal of the American Medical Association.
Preliminary data from this study showed that T-cell esophagitis, basal cell hyperplasia, and spleen cell hyperplasia were observed in patients with severe GERD treated effectively with proton pump inhibitors (PPIs) after PPI discontinuation, but with resistant superficial cells.
According to study leader at the Dallas Veterans Medical Center, Dr. Kerry Dunbar, This finding suggests that the pathogenesis of reflux disease may be related more to inflammatory mediators and cytokines than to chemical damage to the esophageal mucosa.
The inflammatory immune theory of GEB could more easily and better explain not only the onset and course of the typical symptoms of this disease, but also the pathophysiology of the complications of this pathology - metaplasia of the esophagus and Barrett's mucosa.
Barrett's esophagus
Recent experimental studies in rats also suggest that GERD is more related to immune rather than chemical acid damage to the esophageal mucosa. Reflux and chemical acid irritation are thought to only initiate immune inflammatory responses in the esophageal mucosa and therefore play a less important role.
If the immuno-inflammatory theory of the etiopathogenesis of GERD turns out to be correct, it may be necessary to reconsider the existing regimen for the treatment and prevention of relapses of GERD. It is possible that the location and role of antisecretory drugs (PPIs, H2 blockers) may change.
It is assumed that the immune theory of reflux disease can explain in more detail the causes and essence of not only typical, but also recently described atypical forms (so-called subtypes) of GERD.
Researchers suggest that PPIs and H2 blockers may remain the most important drugs for treating GERD, but treatment regimens for this disease should also include drugs that affect the immune-inflammatory response cascade, especially for more severe and refractory forms of GERD.
The latest guide to GERD in children - 1
I will post the latest NASPGHAN/ESPGHAN guideline in the form of abstracts
Advice and comments are welcome.
Definition:
Gastroesophageal reflux (GER) is the release of stomach contents into the esophagus with the presence/absence of regurgitation and vomiting.
Gastroesophageal reflux disease (GERD) is a condition where GER causes unpleasant symptoms that affect the child’s well-being and/or lead to complications.
These definitions were used in the NASPGHAN/ESPGHAN guideline in 2009 and the NICE guideline in 2015.
What does GERD refer to?
General symptoms.
- Discomfort/irritability
- Stunting
- Refusal to eat
- Sandifer syndrome
Gastrointestinal symptoms
- Repeated regurgitation with/without vomiting in older children
- Heartburn/chest pain
- Epigastric pain
- Vomiting blood
- Dysphagia (difficulty swallowing)/odynophagia (painful swallowing)
Respiratory symptoms.
- Cough.
- Stridor.
- Wheezing.
- Hoarseness.
Manifestations of GERD in the esophagus:
- Esophagitis.
- Esophageal strictures.
- Barrett's esophagus.
Common manifestations of GERD.
- Anemia.
- Erosion of tooth enamel.
Manifestations from the respiratory tract.
- Apnea.
- Asthma.
- Repeated aspiration pneumonia
- Repeated otitis media.
Algorithm for infants with suspected GERD in the absence of red flags.
- Elimination of overeating.
- Thickeners.
- Continue breastfeeding.
↓
If there is no effect:
For 2-4 weeks, exclusion of milk protein from the mother’s diet or transfer to a hydrolyzate/amino acid mixture.
↓
If there is no effect:
Referral to a pediatric gastroenterologist or, if not possible, a course of anti-acid therapy for 4-8 weeks (in Russia, anti-acid therapy for children under one year of age is still off label).
Red flags are signs in babies that should make the doctor wary and think about a more serious cause of spitting up.
Are common:
Mass loss
Lethargy, apathy
Fever
Increased irritability, painful behavior
Dysuria - urinary disorders
Regurgitation occurs after 6 months or persists after 12-18 months
Neurological:
Rapid growth of head circumference or bulging fontanelle
Convulsions
Micro/macrocephaly - unusually large or small head circumference for age
Gastrointestinal - from the gastrointestinal tract:
Frequent vomiting
Night vomiting
Vomiting bile or blood
Chronic diarrhea
Rectal bleeding
Bloating
Discussion of diagnostic techniques for GERD.
X-ray of the stomach.
Routine use, especially in uncomplicated GERD, is not indicated, but fluoroscopy may be used in certain situations (presence of red flag symptoms, poor response to conventional therapy) or to exclude anatomical abnormalities - diaphragmatic hernia, malrotation, pyloric stenosis, antrum membrane , stenosis and duodenal membrane, narrowing of the esophagus, Schatzki ring, achalasia, esophageal stricture, external compression of the esophagus. The study is also relevant for children after antireflux operations.
Thus, there is no evidence to support the use of barium testing for the primary diagnosis of GERD in children.
Ultrasound.
When compared with a 24-hour study of pH in the esophagus, ultrasound shows high sensitivity (up to 95%), but low specificity (11%).
Ultrasound is not recommended for routine diagnosis of GERD.
The usefulness of ultrasound has been noted in cases of suspicion of certain conditions with symptoms similar to GERD (primarily pilostenosis), to exclude other diagnoses manifested by discomfort and vomiting (hydronephrosis, ureteropelvic obstruction, gallstones, ovarian torsion).
Like X-rays, ultrasound can determine the diaphragmatic hernia, the length and position of the lower esophageal sphincter relative to the diaphragm, and the size of the angle of His.
FGDS.
Erosion in the esophagus visible during FGDS, in the presence of an appropriate clinical context, confirms the diagnosis of GERD.
Meanwhile, GERD can occur in the absence of endoscopic or histological changes in the esophageal mucosa.
The general opinion of experts is that there is insufficient data to support the use of FGDS with/without biopsy for the diagnosis of GERD in children.
Some notes on the role of the FDS:
When FGDS is still useful:
- to examine mucous membranes in the presence of certain threatening signs (for example, vomiting blood)
- to determine complications of GERD (Barrett's esophagus, strictures)
- to diagnose factors predisposing to GERD (diaphragmatic hernia)
- for the diagnosis of diseases similar to GERD (eosinophilic esophagitis, infectious esophagitis)
Important:
There are no studies in children or adults demonstrating that microscopic esophagitis without visible erosions and associated complaints is adequate for the diagnosis of GERD, although in certain clinical contexts microscopic esophagitis indicates the presence of pathological acid reflux, determined by pH-metry.
The role of histological examination is important in the following situations:
- eosinophilic esophagitis
- Crohn's disease
- Barrett's esophagus
- infections, etc.
Safety of FGDS.
FGDS under general anesthesia is a safe procedure in pediatric practice.
According to an analysis of the pediatric endoscopy database PEDS-CORI (Pediatric Endoscopy Database System Clinical Outcomes Research Initiative), the emergency complication rate was 2.3% (10,236 procedures were analyzed in 9,234 children), with a complication rate of 1.7% for general anesthesia vs 3.7% for i.v. sedation. According to observation data of almost 400 children after FGS with general anesthesia, most of the complications or side effects were not serious, of which about a third were temporary hoarseness and sore throat.
The role of endoscopy in the assessment of extraesophageal symptoms.
The incidence of erosive esophagitis in children with purely extraesophageal symptoms is unknown, and the assessment situation is complicated by the widespread use of proton pump inhibitors.
Up to 32% of children with purely extraesophageal symptoms (eg, cough only or other respiratory manifestations) have microscopic esophagitis, and up to 8% have evidence of eosinophilic esophagitis.
Therefore, the main reason for performing EGD in this group may be to exclude diseases masquerading as GERD, such as eosinophilic esophagitis.
FGD is also useful in excluding candidal esophagitis in children receiving inhaled steroids and in excluding esophagogastric junction obstruction (due to fundoplication or untreated or partially treated achalasia).
When is it better to perform FGDS - before treatment or during anti-acid treatment?
The issue has become very relevant in recent years against the backdrop of discoveries related to eosinophilic esophagitis (EoE).
Initially, the diagnosis of EoE was made when esophageal eosinophils were detected with more than 15 eosinophils per field of view with normal pH-metry results or after a lack of response to an eight-week course of proton pump inhibitors (PPIs).
After a subgroup of PPIs, sensitive EoE, was discovered, it became clear
that in some patients with EoE, after a course of PPI, the morphological signs of inflammation disappeared and these patients received erroneous diagnoses of non-erosive GERD, a hypersensitive esophagus, or were subjected to additional unnecessary examinations.
In light of this, guidelines for adults suggest performing FGDS with a biopsy outside of anti-acid therapy.
The advantage of this approach is that the patient receives the correct diagnosis already during the first endoscopy, but there is also a disadvantage - a second endoscopy may be required to assess the effectiveness of treatment.
Regarding children, there is no clear position yet; the issue is resolved individually in discussion with patients and their families.
Biomarkers of extraesophageal manifestations of GERD (pepsin level in saliva, bronchoalveolar lavage, middle ear fluid, some other indicators) are not yet recommended by experts for use.
Esophageal manometry.
Experts do not support the use of manometry to diagnose GERD, but the method may be considered for diagnosing motility disorders.
Scintigraphy.
There is insufficient evidence to support the use of scintigraphy to diagnose GERD in children.
Scintigraphy may sometimes be used in the absence of response to standard therapy or to rule out other diagnoses/triggers (eg, delayed gastric emptying).
Trial treatment with proton pump inhibitors.
A short 1-2 week course of PPI is used to diagnose GERD in adults (sensitivity 78% - 83%).
Experts assessed the results of five randomized clinical trials in infants and found insufficient evidence to recommend empirical PPI treatment in infants to confirm GERD.
When assessing the effectiveness of empirical PPI therapy in older children, experts had no doubt about its usefulness, but there were disagreements about the duration of the course. As a result, a longer course of empirical therapy was recommended—4–8 weeks.
A course of PPI as a diagnostic test for extraesophageal symptoms.
Two randomized clinical trials were analyzed (long-term in children with asthma and short in infants) and found no benefit from this approach, so experts do not recommend a course of proton pump inhibitors as a diagnostic test for extra-esophageal symptoms of GERD.
PH-metry.
Assessed 7 studies on the value of pH testing in children.
The difficulty for experts was that normal values for children are not clearly known due to ethical restrictions on performing invasive procedures in healthy children. When used in this case as the gold standard for diagnosing GERD, complaints and physical examination data, the authors of one of the studies concluded that the determination of the reflux index (the percentage of time at which the pH in the esophagus is less than 4) has a sensitivity of 50% and a specificity of 82%. .
Limitations associated with pH measurement technology.
- There is a lack of an adequate “gold standard” for evaluating pH data. In early studies, pH-metry data were compared with data from manometry, endoscopy, scintigraphy, clinical symptoms, and barium studies. But all these technologies have their limitations and produce many false positive results.
- The invasive nature of the procedure, for ethical reasons, limits its use in healthy children, who can serve as a control group.
- Non-acidic reflux in infants and children is common in children, and pH testing does not detect refluxes with a pH above 4 (in children this is 45-89% of all refluxes).
- pH-metry does not readily identify high refluxes (the entire length of the esophagus), making the technology inadequate for assessing extraesophageal symptoms.
- The desire to assess the relationship of a symptom with an episode of reflux is one of the main indications for pH-metry, but patients or their parents often cannot assess the symptoms in time, which makes it difficult to establish a reflux-symptom correlation. The time frame within which a symptom can be associated with an episode of reflux also continues to be debated.
Despite these limitations, the working group identified several indications for pH testing when more accurate pH impedance testing is not available:
- Diagnosis of acid-related conditions: pH testing can be useful in correlating symptoms with episodes of acid reflux. This is important for the differential diagnosis of non-erosive GERD and other disorders such as hypersensitive esophagus or functional heartburn, as well as to clarify the causes of conditions such as dental erosion.
- Relate persistent symptoms to episodes of acid reflux.
- To evaluate the effectiveness of anti-acid therapy. In patients with persistent symptoms or esophagitis in high-risk groups (achalasia, cystic fibrosis, neurological patients) during anti-acid treatment, pH measurement allows assessing the severity of acid breakthroughs, since patients in these groups often do not achieve adequate acid suppression on standard doses.
Experts see no evidence to support the routine use of pH testing to diagnose GERD.
Other techniques related to pH measurement.
Wireless pH measurement (sensors like clips are endoscopically placed in the esophagus and the results are read remotely within 1-5 days) - convenient for certain groups of patients (children with neurological disorders, autism, chronic cough due to cystic fibrosis, children athletes) and can increase accuracy research by increasing the duration of observation.
Oropharyngeal pH-metry—showed low sensitivity in studies on adults and children and is not recommended.
Determination of pH of exhaled air condensate—according to preliminary data, sensitivity is insufficient.
12, total, today
Treatment of gastroesophageal reflux disease
According to current guidelines, GERD is treated in stages. Goal of treatment: control the symptoms of the disease, treat esophagitis, prevent relapses of esophagitis and complications of the disease.
Treatment of GERD consists of the following steps:
- Lifestyle changes and control of gastric juice secretion (antacids, PSI, H2B).
- If necessary, surgical treatment is used, and corrective antireflux surgery is performed.
Non-pharmacological measures include the following:
- Reducing excess weight;
- Refusal of certain drinks and foods (alcohol, chocolate, citrus fruits, tomatoes), mint, coffee, onions, garlic;
- Frequent meals at regular intervals;
- Sleep at least 3 hours after eating, with your head raised (~ 20 cm);
- Limiting squats, bending, etc.
Eating frequently at regular intervals
Antacids
Until the 1980s, antacids were the standard treatment for mild forms of GERD. They are still used to reduce symptoms of mild reflux. Antacids are taken after each meal and before bed.
Taking antacids before bed
Antacids are also useful for side effects: they relieve constipation (aluminum antacids: ALternaGEL, Amphojel), they can increase loose stools (magnesium antacids: Phillips Milk of Magnesia). Aluminum hydroxide increases the pH of the stomach contents to >4 and inhibits the proteolytic activity of pepsin, reducing the symptoms of indigestion. Antacids do not reduce the frequency of reflux, but they do reduce the acidity of the fluid.
Magnesium hydroxide suppresses the symptoms of acidosis and improves digestion. Magnesium hydroxide antacids osmotically retain fluids in the intestine, which distends the intestinal wall, stimulates intestinal motility, and softens stools (laxative effect). When interacting with hydrochloric acid of gastric juice, magnesium hydroxide is converted into magnesium chloride.
New antacids and antirefluxants
Alginic acid salts have been used clinically to relieve symptoms of heartburn and esophagitis for over 30 years. Alginic acid salts have a unique mechanism of action: when interacting with gastric acid, alginates precipitate and form a gel that covers the esophageal mucosa with a protective layer and promotes its restoration.
In vitro and in vivo studies have shown that alginates combine carbon dioxide and some antacid components. Recent kinetic studies have shown that alginates bypass acidic contents and reach the esophagus before the esophageal contents, protecting the organ mucosa from mechanical and chemical irritation from hydrochloric acid. According to clinical studies, alginates also act as a physical barrier, thereby more effectively suppressing reflux.
Alginate products contain antacids, which are acid neutralizing agents that reduce heartburn, but studies have not shown that the effectiveness of these combination drugs depends on their neutralizing properties.
The clinical effectiveness of alginate preparations depends on many factors: the amount and penetration of carbon dioxide released, the characteristics of the molecule, additional ingredients (aluminum, calcium) that have a positive potentiating effect.
Alginate preparations remain in the stomach for several hours, so they last significantly longer and are more effective in suppressing the symptoms of GERD than traditional antacids, they begin to work quickly and last a long time. Alginate preparations are completely safe and are therefore used to reduce the symptoms of reflux in infants, children and pregnant women.
For example, one of these magnesium alginate preparations, Refluxaid, is used in European countries to reduce the symptoms of reflux and acidosis in GERD, peptic ulcers, esophagitis, functional dyspepsia, and other functional and inflammatory diseases of the gastrointestinal tract, manifested by heartburn, reflux, and epigastric discomfort.
Refluxaid drug
The magnesium alginate in Rexluxaid is a natural substance extracted from seaweed. The drug has a high viscosity, which increases anti-reflux effectiveness and duration of action. It has emulsion and swelling properties.
Studies have shown that the highly viscous compound Refluxaid, when ingested into the stomach, creates a physical barrier that binds and neutralizes gastric juice, thereby protecting the esophagus from symptoms of reflux: heartburn, burning behind the sternum, chest pain, epigastric discomfort, etc. Taking these The medication reduces heartburn, acid regurgitation, dysphagia and odynophagia (difficulty swallowing and pain) are reduced, and extrazophaginic symptoms of GERD are also suppressed - cough, hoarseness.
Refluxaid is a prescription medication. It is used for episodic relief of symptoms of acidosis, reflux and esophagitis, on demand or in combination with anti-reflux medications (antisecretory PPIs, H2 blockers, prokinetics).
It has been found that when a person sleeps, magnesium alginate can remain in the stomach for up to 8 hours without breaking down—enough time for the patient to get a good night's sleep. Taking reflux before bed may improve the quality of sleep in a patient with GERD because the symptoms caused by nocturnal reflux will be suppressed.
Symptoms
The clinical picture depends on the severity of the inflammatory process and the condition of the esophageal sphincter; reflux esophagitis is accompanied by a complex of dyspeptic, pulmonary and cardiac disorders. The main symptoms of reflux esophagitis are:
- Heartburn, manifested as a burning sensation behind the sternum, in the area of the xiphoid process, is the most characteristic symptom, occurring in more than ¾ of patients. Unpleasant and painful sensations can appear after eating, during physical activity, bending the body, and even in a horizontal position; wearing a tight belt can provoke heartburn.
- Belching that occurs after eating or carbonated drinks is the second most common symptom of reflux esophagitis. It can appear even in a horizontal position of the body, but more often during physical activity.
- Dysphagia is difficulty passing food that occurs when the motility of the upper parts of the digestive tract is impaired or when stricture is a narrowing of the lumen of the esophagus.
- Odynophagia is a retrosternal or interscapular pain that occurs when food passes through the esophagus. Painful sensations can radiate to the intercostal space and even resemble an angina attack.
- Regurgitation is regurgitation in which the contents of the stomach enter the oral cavity. Appears regardless of body position and physical activity of a person.
There are also extraesophageal manifestations involving other organs, e.g.
- bronchopulmonary: cough, attacks of respiratory discomfort or suffocation at night; the cause is the entry of small particles of stomach contents into the bronchi;
- otolaryngological: hoarseness, signs of rhinitis, pharyngitis due to refluxant entering the larynx;
- dental: thinning of tooth enamel, caries as a result of the aggressive action of acid.
If left untreated, reflux esophagitis can cause severe complications. If the wall of the esophagus is damaged down to the submucosal layer, there is a risk of ulcer formation, which can cause bleeding. Scars formed after healing can lead to stricture, a narrowing of the esophagus.
The most severe complication is Barrett's esophagus syndrome - the squamous epithelium characteristic of the esophagus is replaced by a cylindrical epithelium characteristic of the gastric mucosa. With metaplasia, the likelihood of developing cancer increases by more than 30 times.
Antisecretory drugs, H2 receptor blockers
This is the first-line treatment for mild to moderate GERD and grade I-II esophagitis. Four H2 blockers are commonly used in clinical practice: ranitidine, famotidine, cimetidine, and nizatidine. They are more effective in suppressing unstimulated secretion of gastric juice with food and are therefore recommended on an empty stomach or at night.
H2 blockers are effective in the treatment of mild esophagitis (70-80% of patients recover), as well as in antirecessive treatment and prevention of relapses. The effectiveness of H2 blockers decreases with long-term use, leading to tachyphylaxis. An H2 blocker is recommended for patients suffering from nocturnal reflux symptoms, especially in Barrett's temple.
Surgery
If conservative treatment is ineffective, if complications arise, if there is an esophageal hernia, as well as if there is pain behind the sternum or if there are extra-esophageal signs (cough, hoarseness, etc.), surgical treatment is recommended - fundoplication. The purpose of surgery for reflux esophagitis is to restore normal anatomical relationships in the area of the esophagus and stomach, creating a mechanism that will prevent the reflux of gastric contents into the esophagus.
Most surgeons in domestic clinics perform circular Nissen fundoplication; during the operation, a cuff is created - the fundus of the stomach is wrapped around the esophagus 360°, which prevents reflux in the future. But a valve formed in this way leads to the loss of natural protective mechanisms: the ability to regurgitate and vomit. Large portions of food and drinking carbonated drinks lead to the fact that, if necessary, their removal through the cardia is impossible, discomfort and pain appear. The formed cuff often slips off after 1-2 years, which leads to relapse of the disease.
Proton pump inhibitors (PPIs)
These are powerful drugs that suppress gastric secretion. Clinical studies have shown that they are most effective in treating GERD. PPIs are generally well tolerated and cause relatively few side effects. However, PPIs can disrupt calcium homeostasis, exacerbating existing cardiac conduction abnormalities. PPIs increase the risk of hip fractures in postmenopausal women.
Multiple clinical trials have concluded that PPIs are more effective than H2 blockers in controlling GERD symptoms over 4 weeks. And are more effective in treating esophagitis within 8 weeks. It also reports that no one PSI drug was found to be more effective than others in controlling GERD symptoms over 8 weeks.
Although PPIs are the most effective antisecretory drugs, their use, especially over a long period of time, is associated with many side effects. Firstly, PPIs have restrictions on their use: they cannot be used in children under 1 year of age, pregnant or lactating women. PPI use during pregnancy has been shown to increase the risk of birth defects (heart defects).
Restrictions on the use of PPIs
Research conducted in the United States shows that overuse of PPIs has dangerous consequences. Therefore, the US FDA warns doctors and patients that there should be no more than three 14-day courses of treatment per year. Long-term or frequent use of PPIs is associated with an increased risk of bone fractures, hypovitaminosis B12, electrolyte imbalances (primarily hypomagnesemia), muscle spasms, and even seizures.
Excessive suppression of gastric acid secretion when taking PPIs can cause epigastric discomfort, indigestion, increased intestinal infections (C. difficile, etc.), and the risk of aspiration pneumonia. The risk of infectious complications is even higher when PPIs are used with H2 blockers.
Prokinetics
Prokinetics are only effective in treating mild forms of GERD. If GERD is more severe, in addition to prokinetics, drugs that inhibit the secretion of gastric juice are usually prescribed.
Of the prokinetic agents, metoclopramide (10 mg/day orally) is prescribed in European clinics - this is the most commonly prescribed regimen in adults with GERD. Long-term treatment with prokinetic drugs can be dangerous, with serious, even fatal, complications.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.