Pancreatitis is one of those diseases that may not manifest itself for a long time, thereby complicating the process of subsequent treatment. However, there are a number of signs by which an attentive person can detect certain changes in his body and respond to them in time. One of these signs is stool.
Feces with pancreatitis change quite a lot, so it is important to pay attention to this and consult a doctor, even if there is nothing else to worry about. If you doubt whether the appearance of feces is normal, you can always find a photo on the Internet and compare. If the pancreas malfunctions, the stool becomes liquefied, does not come out immediately, but in small parts, and contains undigested food particles, which indicates a lack of enzymes.
There are quite a lot of options for the shape and consistency of stool with pancreatitis, but we can highlight those that are most common:
- Thin and long, resembling a ribbon. This option indicates problems with the sigmoid colon and tumor processes.
- The so-called "sheep's balls", indicating the presence of constipation and ulcers.
- Unshaped chair.
Healthy human feces
Whatever lifestyle a person leads, in medicine there are standards regarding his waste products:
- ratio of dense particles and water 20/80%;
- stool frequency at least once every two days;
- bowel movements should occur easily, without causing discomfort;
- the average stool volume of a healthy person is 150–400 grams per day;
- the feces should be cylindrical in shape and light, contrary to the popular joke that the feces of a healthy person sink, slowly sinking to the bottom.
A healthy lifestyle is the key to good health. Active people who play sports rarely experience bowel problems
Changes in stool substance
The main sign of the development of a pathological process in the pancreas is the appearance of pain in the hypochondrium, 50-60 minutes after eating fatty, salty, sweet, spicy or fried foods. After which, the development of the following symptoms may be observed:
- the contents of the intestines begin to ferment;
- gas accumulation occurs, which causes intoxication;
- bloating appears in the abdominal area;
- diarrhea occurs.
If no measures are taken to eliminate the pathology, then structural changes in the pancreas can lead to death. Laboratory researchers pay special attention to the color of stool during pancreatitis, changes in its consistency and substance.
With the development of pancreatitis, stool takes on a mushy appearance with a liquid state. Bowel movements occur in small portions. The stool may contain fats, meat fibers and other components of undigested food, which is evidence that there is a deficiency of enzymes that facilitate the absorption and digestion of ingested food products. The presence of undigested fats in stool can cause frequent stools, as well as their transformation into a liquid and foamy state. The urge to defecate may occur up to 3-4 times a day. The stool substance may have the following states:
- a ribbon-like appearance, indicating a pathological change in the sigmoid intestine, the development of a tumor and the appearance of spasms in the sphincter;
- a small spherical appearance resembling sheep feces indicates the development of constipation or ulcerative lesions;
- cylindrical appearance, indicates the normal volume of plant and animal foods in the intestinal cavity;
- shapeless excrement indicates a vegetarian diet; feces contain a large amount of fiber.
The optimal state of the norm of fecal substance should contain the following ratios:
- dense fractions – 20%;
- water – up to 80%;
- The frequency of stool can be up to two times a day, but not less than once in 48 hours.
Normally, during bowel movements there should be a feeling of relief, without unnecessary discomfort and pain. No more than 400 grams should be consumed per day. feces, but when eating plant foods, the amount of stool may increase, and when eating fatty foods, the volume of stool decreases. A light state of feces is considered normal, ensuring a smooth sinking to the bottom in the water.
Changes in stool depending on the form of pancreatitis
Stool with pancreatitis directly depends on the stage of the disease and concomitant diseases. The most obvious violations occur during the period of exacerbation, the feces acquire a gray color with a pearlescent tint. This disease is complicated by constipation, indicating an inflammatory process in the digestive tract.
After the transition of acute pancreatitis to chronic pancreatitis, diarrhea overtakes a person. Loose stools can be explained by several reasons:
- in the case of pancreatitis of alcoholic origin, the digestive tract, weakened by toxins, cannot cope with its functions;
- Disturbance of microflora entails the appearance of dysbacteriosis;
- there is an acute shortage of enzymes necessary for complete digestion of food;
- intestinal motility is disrupted.
Symptoms of pancreatitis
Symptoms of pancreatitis depend on its form. The acute form of inflammation is characterized by sharp pain in the left upper abdomen, and in the chronic form, symptoms may not be observed at all. Common signs of pancreatitis are:
- pain in the upper abdomen that radiates to the back;
- nausea or vomiting;
- indigestion;
- hiccups
In response to inflammation in pancreatitis, body temperature often rises. Cholecystitis, an inflammation of the walls of the gallbladder, has similar symptoms (nausea, vomiting, fever, abdominal pain). Therefore, to make a correct diagnosis, a consultation with a gastroenterologist is necessary, who can prescribe a blood test (biochemical, liver tests), ultrasound of the liver, cholegraphy (x-ray of the liver and bile ducts).
Features of diarrhea with pancreatitis
Digestive dysfunction is the main symptom of diseases associated with inflammation of the pancreas.
The stool takes on a mushy consistency, and the urge to have a bowel movement appears after every meal.
There are a number of features of stool with pancreatitis:
- During antibacterial therapy, stool becomes yellow and resembles plasticine in consistency.
- With pancreatitis, the color of stool changes to gray or very light, and undigested fats add shine to it;
- Feces have a foul odor and become very viscous (it is difficult to wash off clothes and is difficult to wash off surfaces).
Lack of medical care or untimely initiation of treatment can lead to very unpleasant consequences, the basis of which is dehydration:
- weight loss;
- inflammation of the mucous membranes;
- anemia;
- acute lack of vitamins and minerals;
- insomnia;
- apathy against the background of permanent neurosis.
One of the most alarming symptoms of pancreatitis is black diarrhea. Any doctor, hearing such a complaint, will be seriously concerned about the patient’s condition, since this indirectly indicates internal bleeding. It is blood that can color stool black.
Sometimes black stool is the result of eating foods that contain dye. Activated carbon has the same effect.
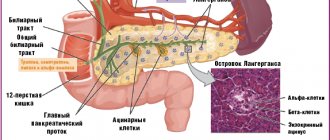
Pancreatitis is inflammation of the pancreas.
The pancreas is a long, flat organ located in the upper abdomen behind the stomach. It produces enzymes that aid digestion and hormones that regulate blood sugar levels.
Pancreatitis can be acute or chronic.
Acute pancreatitis occurs suddenly and usually resolves quickly, but severe cases cause complications and can be life-threatening.
Chronic pancreatitis occurs over a long period of time; it is characterized by irreversible and progressive changes in the pancreas. Exacerbations of the chronic process may occur.
Mild cases of pancreatitis often do not require treatment, but severe cases require emergency medical attention.
Synonyms Russian
Acute pancreatitis, chronic pancreatitis.
English synonyms
Acute pancreatitis, chronic pancreatitis.
Symptoms
Symptoms of acute pancreatitis:
- pain in the upper abdomen,
- abdominal pain radiating to the back (girdling pain),
- bloating in the upper abdomen,
- nausea,
- vomit,
- abdominal pain when palpated,
- rapid pulse,
- low blood pressure.
Symptoms of chronic pancreatitis:
- aching pain in the upper abdomen, can be girdling, intensifies 40-60 minutes after eating,
- stomach upsets,
- nausea, bloating,
- weight loss,
- frequent, greasy, foul-smelling stools.
General information about the disease
Normally, the pancreas produces enzymes, which then enter the duodenum in the form of pancreatic juice, where they become active and participate in the breakdown of proteins, fats and carbohydrates. The enzyme amylase plays a major role in the digestion of carbohydrates; lipase promotes the breakdown of fats.
The pancreas also produces hormones - insulin and glucagon. They regulate blood sugar (glucose) levels.
With pancreatitis, enzymes are activated directly in the pancreas. This can occur under the influence of alcohol, blockage of the pancreatic duct with a stone, due to exposure to viruses, due to injury and a number of other reasons. The result is the so-called self-digestion of the pancreas, which causes inflammation, swelling and damage to the organ.
Repeated attacks of acute pancreatitis can contribute to its transition to a chronic form.
The scars that form after attacks of pancreatitis reduce the number of working pancreatic cells. This reduces the production of enzymes, which especially affects the digestion of fats - the feces become fatty and plentiful. Due to insufficient digestion, a person does not receive enough nutrients, which leads to weight loss. A decrease in the number of cells that produce insulin causes the development of diabetes.
The causes of acute and chronic pancreatitis can be:
- alcoholism (70-80%) – acute pancreatitis is usually preceded by several years of regular alcohol abuse;
- gallstones – in this case there may be no symptoms for a long time, so acute pancreatitis occurs completely unexpectedly for the patient;
- abdominal surgery;
- taking certain medications, in particular furosemide and oral contraceptives;
- smoking;
- cystic fibrosis;
- hereditary predisposition;
- high levels of calcium in the blood (hypercalcemia);
- high levels of parathyroid hormone in the blood (hyperparathyroidism);
- high levels of triglycerides in the blood (hypertriglyceridemia);
- infections (cytomegalovirus, mumps, etc.);
- abdominal injuries;
- pancreas cancer.
Pancreatitis can lead to the following serious complications.
- Pulmonary dysfunction. Acute pancreatitis can lead to lung damage, which is associated with large amounts of pancreatic enzymes entering the blood and the development of systemic inflammation.
- Infections. Acute pancreatitis may increase the vulnerability of the pancreas to infectious agents. Inflammation of the pancreas caused by infection requires intensive treatment, including removal of the affected tissue.
- Kidney failure. Acute pancreatitis sometimes leads to kidney failure, which is so severe that it requires filtering the blood (hemodialysis).
- Pancreas cancer. Long-term inflammation of the pancreas in chronic pancreatitis increases the risk of developing pancreatic cancer.
- Pseudocysts. Acute pancreatitis can lead to the accumulation of fluid in peculiar bubbles in the pancreas. The rupture of such a pseudocyst is fraught with internal bleeding and the spread of infection.
Who is at risk?
- Regular drinkers.
- People who tend to overeat are associated with an increase in the amount of fat (triglycerides) in their blood.
- Patients with stones in the gall bladder or bile ducts.
- Recently undergone abdominal surgery.
- Pancreatic cancer sufferers.
Diagnostics
In case of acute severe abdominal pain, acute pancreatitis is always suspected first. In this case, the determination of the content of pancreatic enzymes in the blood and urine is of key importance in making a diagnosis.
- Pancreatic amylase. The level of amylase, an enzyme secreted by the pancreas and responsible for the digestion of carbohydrates, increases significantly with pancreatitis. In acute pancreatitis, it increases within 2-12 hours from the onset of symptoms and remains elevated for 3-5 days (may exceed the norm by 5-10-20 times). Since amylase is also found in the salivary glands and other organs, its increase is not always associated with pancreatic disease and an increase in pancreatic amylase is specific for damage to the pancreas.
In chronic pancreatitis, amylase levels may remain normal.
- Amylase in urine corresponds to the level of amylase in the blood, but increases with a delay of 6-10 hours.
- Lipase. The level of lipase in the blood, an enzyme secreted by the pancreas and responsible for the digestion of fats, also increases significantly with pancreatitis. This occurs within 24-48 hours after the onset of an attack of acute pancreatitis and persists for up to 12 days. Lipase, unlike amylase, is found only in the pancreas, so its increase is more specific to damage to the pancreas. In cases of chronic pancreatitis, an increase in blood lipase levels is observed more often than an increase in amylase.
- Blood elastase. Another enzyme produced by the pancreas, an increase in which is characteristic of acute pancreatitis.
- C-reactive protein. Reflects the presence of active inflammation. It can be significantly increased in acute pancreatitis, but is not specific only for this disease.
Diagnosis of chronic pancreatitis is based on detecting signs of calcification of the pancreas, impaired digestion of fats (copious, fatty feces) and the development of diabetes mellitus.
- A coprogram (general stool analysis) allows you to assess the quality of the body’s absorption of nutrients (with chronic pancreatitis, the amount of fat in the stool increases, fat and proteins can be found in undigested form).
- Coprological elastase is the gold standard for determining decreased secretion of enzymes by the pancreas. Elastase is formed in the intestine under the action of pancreatic juice enzymes and then remains unchanged, excreted from the body in feces. A decrease in its amount in feces indicates impaired pancreatic function.
Research:
- Ultrasound of the abdominal cavity makes it possible to judge swelling and inflammation of the pancreas in acute pancreatitis, the presence of stones in the gall bladder and bile ducts, and to identify the presence of pseudocysts. Also, using ultrasound, you can detect foci of calcification of the pancreas, characteristic of chronic pancreatitis.
- Computed tomography (CT) provides a more detailed image of the pancreas and its ducts, which greatly helps in diagnosing pancreatitis.
- An endoscopic ultrasound test looks for inflammation and blockage in the bile ducts or pancreas.
Long-term chronic pancreatitis increases the likelihood of pancreatic cancer, so additional examinations aimed at early detection of this disease may be prescribed.
The scope of the examination is determined by the attending physician.
Treatment
Acute pancreatitis
An acute attack of pancreatitis requires emergency hospitalization. During treatment, measures are taken to relieve pain. Complete fasting for several days is mandatory, since food intake provokes the release of pancreatic enzymes, which aggravates the patient's condition. Fluids, nutrients and medications are given only intravenously. If pancreatitis is caused by a gallstone blockage, surgery may be required to remove it. Surgery may also be necessary to remove damaged areas of the pancreas.
Chronic pancreatitis
Treatment of chronic pancreatitis comes down to preventing exacerbations, relieving pain and replacing the functions of the pancreas:
- giving up alcohol,
- moderate consumption of fatty foods,
- taking enzymes to facilitate digestion,
- control of sugar levels and, if necessary, insulin therapy.
Prevention
To prevent the development of pancreatitis, it is recommended:
- do not abuse alcohol,
- eat more vegetables and fruits,
- monitor your body weight.
Recommended tests
- Serum total amylase
- Pancreatic amylase
- Total amylase in daily urine
- Lipase
- Serum elastase
- Coprological elastase
- Coprogram
- Plasma glucose
Is green really safe?
In the absence of any changes in the diet of a person suffering from inflammation of the pancreas, the stool should always be the same. If the stool suddenly turns green, this clearly indicates the presence of bile in it. In such cases, you should immediately inform your doctor, who will prescribe a therapeutic diet. In addition, the following measures should be taken:
- exclude fatty, fried, smoked, any types of canned food, sweets;
- completely avoid alcohol, coffee and carbonated drinks.
The presence of traces of bile in the stool may indicate excessive production of enzymes or their stagnation. Only a doctor can definitely dispel doubts
In addition to diet, it is necessary to use medications that can only be prescribed by a specialist, based on test results.
Measures to normalize the color of stool
To get rid of diarrhea, adhere to the treatment table, which is recommended by the doctor. Patients with pancreatitis always need a special diet. Often, diet No. 5 is used to treat the pancreas.
You can eat the following foods:
The ideal solution is when the treatment table is compiled for a specific patient, taking into account all the features of the pathology.
If there is mucus in the feces, the patient is prescribed hospital treatment or surgery. The laparoscopic method is often used.
To prevent a radical method, restoration of the intestinal microflora is required, which is carried out using enemas. The procedure is carried out up to 3 times a day for about 5 days. After cleansing, you need to drink probiotics, products that contain bifidobacteria and lactobacilli.
The process of normalizing stool includes therapeutic measures with medication.
- Analgesics.
- Antibiotics.
- Painkillers.
- Vitamins.
- Hormones.
- Calcium.
The use of enzymatic agents promotes the excretion of digestive juice in the required volume, which leads to an improvement in overall well-being and normalization of the stool color consistency in pancreatitis.
Since problems with bowel movements develop due to stress and emotional overstrain, the doctor will prescribe sedative medications.
To determine the sugar norm, you need to indicate your sugar or select your gender to get a recommendation, move the slider to the required level, click the show button.
Pancreatitis is one of the most serious diseases that can occur in any person, regardless of age and gender. Violation of the functionality of the pancreas completely affects the digestive processes and causes gas formation, bloating and diarrhea. Among other things, feces also change with pancreatitis. To make an accurate diagnosis, specialists prescribe an ultrasound of the abdominal cavity, as well as general urine and blood tests and a stool test to study its substance, consistency and color, which indicates the degree of pathological disorder in the area of parenchymal organs.
Blood in stool
The most dangerous symptom of pancreatitis, causing anxiety among doctors and fear among patients, is the presence of fresh blood in the stool. There may be several reasons for its appearance:
- tumor processes in the gastrointestinal tract;
- cracks and ruptures of the colon;
- acute inflammatory processes.
At the first detection of blood during a bowel movement, you should immediately consult a doctor, as this may indicate acute pancreatitis.
For diagnosis, the smallest details are very important: the thickness of the clots, their color, the presence of other symptoms
There are symptoms that, in the presence of bloody stool, should prompt you to immediately go to a medical facility:
- painful bowel movements;
- nausea, vomiting, dizziness;
- significant decrease in blood pressure;
- temperature increase.
The occurrence of uncharacteristic bowel movements
Pancreatitis can cause not only diarrhea, but also constipation. As constipation develops, red blood may appear in the stool, indicating a fissure in the anus.
To normalize stool, it is necessary to adhere to a certain dietary regimen, which mainly includes the use of:
- fresh fruit and vegetable crops;
- cereals;
- from sweets – marshmallows and jelly;
- dry bread.
But the main features of the dietary diet are developed individually for each patient.
In some cases, with the development of pancreatitis, mucus may form in the stool. With this phenomenon, therapy can only be prescribed in a hospital setting, up to and including surgical intervention.
The color of a person's bowel movements is not a sufficient factor for making an accurate diagnosis. If any modification of the stool appears, it is necessary to consult a specialist and undergo the necessary examination methods.
Feces with pancreatitis change characteristics due to a deficiency of pancreatic enzymes, which is visible even to the naked eye. If you notice an uncharacteristic odor or color in your stool, especially if you notice that it doesn’t flush well or sticks to the walls of the toilet, consult a doctor and get examined.
Diagnosis of pancreatitis
One of the very first and most reliable tests prescribed for the diagnosis of pancreatitis is a coprogram.
At the initial stages, in laboratory conditions, they find out whether there are traces of undigested food in the stool, the presence of which indicates a lack of enzymes
There are rules for collecting material for analysis, because only if the necessary techniques are followed will the result be reliable. Basic recommendations:
Blood counts for pancreatitis
- before collection, try to avoid taking medications as much as possible;
- follow a therapeutic diet;
- collect feces in a sterile container;
- the material must be fresh (overnight storage in the refrigerator is possible);
- women undergoing analysis during menstruation must use a tampon, having previously carried out hygienic procedures.
A stool test for pancreatic elastase is a reliable way to determine whether inflammation of the pancreas is occurring and to what extent. The fact is that elastase is an enzyme produced by the gland, which, passing all the way through the gastrointestinal tract, does not change either qualitatively or quantitatively. The accuracy of this analysis is 93%. A low level of elastase indicates the development of pancreatitis, and can also be detected in diabetes mellitus.
For a chronic disease, it is recommended to retake this test annually to monitor changes.
Chronic pancreatitis
With chronic pancreatitis, scarring of the pancreas tissue occurs, which is why the functions of the pancreas gradually deteriorate. A characteristic symptom of chronic pancreatitis is the appearance of fatty stools with an unpleasant odor - steatorrhea.
Diabetes is a common complication of chronic pancreatitis. Due to chronic inflammation of the pancreas and an increase in its size, the following anatomical changes may be observed: narrowing of the lumen of the bile duct and adjacent structures (duodenum and colon), formation of pseudocysts in the pancreas.
Treatment of pancreatic diarrhea
Diarrhea, no matter what disease it is caused by, requires an immediate response, because it instantly leads to dehydration of the body and causes serious complications. For pancreatitis, a comprehensive approach is taken to solving this problem:
- prescribe medications;
- recommend strict adherence to a therapeutic diet;
- The use of traditional methods is allowed (with prior consultation with a specialist).
Medications
The treatment strategy for diarrhea always depends on the form of pancreatitis and the presence of concomitant diseases. Traditionally there are 2 ways:
- Oral. It consists of prescribing enzyme-containing drugs that facilitate the functioning of the pancreas (Creon, Pancreatin, Bifidumbacterin, etc.).
- Intravenous. Used in acute periods when immediate response is required. It is carried out in a hospital. Solutions of electrolyte salts are prescribed (Disol, Trisol, etc.)
When taking any medications, you should always strictly follow the instructions and prescription of the doctor.
Methods for treating pancreatitis
Treatment of pancreatitis in the acute phase is symptomatic to prevent complications. A gastroenterologist may prescribe protease inhibitors (enzymes that break down proteins) and hormones that inhibit pancreatic secretion to reduce enzymes that damage cells and increase inflammation. The treatment regimen is prescribed individually based on the results of laboratory tests (biochemical blood test, liver tests, ultrasound of the liver).
Medicines for chronic pancreatitis are prescribed to reduce pain, improve digestion and normalize hormonal levels. To normalize digestion, enzymes and vitamin complexes are prescribed individually. When treating endocrine insufficiency, the doctor usually prescribes a diet and insulin administration (for diabetes).
How to get tested
To obtain reliable data, 4 days before the test you need to switch to a special diet consisting of mashed potatoes, a small amount of other pureed vegetables, cereals, dairy products and fruits. You should not eat heavy foods (meat, fish, eggs), or those containing large amounts of plant fiber - tomatoes, beets and all types of green vegetables.
The daily amount of calories, which must be divided into 5 doses, should not exceed 2250. During this period, you cannot take enzyme preparations. If a colonoscopy or examination of the digestive system using barium was performed, stool sampling can be done after 2 days.
The day before stool collection, you should not do the following:
- enema;
- take laxatives and medications containing bismuth;
- introduce suppositories.
Women should not have stool tested during menstruation.
Before collection, it is necessary to wash the genitals and anus, urinate - there should be no urine in the stool. It is better to defecate in a special vessel and immediately take a sample from it for analysis - approximately 30 g of feces. The material is collected in a dry and clean container, filling it 30%, closed and submitted to the laboratory as quickly as possible, since after cooling the characteristics of the feces begin to change.
Reviews
Lesya, 38 years old, Dnepropetrovsk
The first course was treated with Creon, then I switched to its analogue - Pancreatin, on the advice of a doctor, since a large amount of enzymes is no longer required. The stool was liquid, but then returned to normal.
Mikhail, 26 years old, Taganrog
I have been treating pancreatitis for a year. At first I took Pancreatin, but allergies appeared and dyspepsia worsened. I was tormented by either constipation or diarrhea. I switched to Mezim, I don’t observe any side effects. The tablets work quickly.
Natalya, 40 years old, Altai
Mezim was prescribed to my mother, she had pancreatitis, lost 10 kg in 3 months, and was even referred to an oncologist. The drug normalized digestion, constipation disappeared, and she feels good, despite her age.
- How is urine collected for pancreatitis?
This site uses Akismet to reduce spam. Find out how your comment data is processed.
If you find an error, please select a piece of text and press Ctrl+Enter.