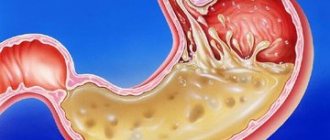
Gastroesophageal reflux disease (GERD) - This is one of the most serious and complex pathologies of the esophagus. The disease can significantly impair the patient's quality of life. As it progresses, it leads to dangerous complications, including Barrett's esophagus and adenocarcinoma. GERD affects both men and women equally often and is difficult to treat. Experienced specialists at the ACMD clinic will help you get rid of the unpleasant manifestations of GERD once and for all. Do not delay your visit to the doctor, contact us at the first symptoms!
Causes of the disease
Often, reflux disease occurs due to a decrease in the tone of the lower esophageal sphincter, and this, in turn, occurs when drinking caffeine and alcohol, smoking, or in the case of pregnancy under the influence of hormonal factors. What other reasons could there be for the development of GERD? Treatment of any ailments with antispasmodics, analgesics, or calcium antagonists can lead to gastroesophageal reflux disease. Also, its occurrence is possible against the background of increased intra-abdominal pressure caused by ascites, obesity, and flatulence. Conditions for reflux are created by a diaphragmatic hernia, when the pressure on the lower region of the esophagus in the chest decreases. An increase in intragastric pressure and the reflux of stomach contents into the esophagus can occur with abundant and hasty consumption of food, since then a lot of air is swallowed along with it. The same consequences are caused by the presence in the diet of excess amounts of foods containing peppermint, rich in animal fats, hot seasonings, fried foods, and carbonated water. A duodenal ulcer can also cause the development of GERD.
Esophagitis: symptoms
The most striking and specific symptom of GERD is heartburn with or without the penetration of stomach contents into the oral cavity. Feelings of heartburn:
- “chill” at the bottom of the throat;
- burning and stinging in the throat;
- bitter or sour taste in the mouth;
- lump in the throat;
- nausea and stomach pain.
Frequent attacks of heartburn can lead to irritability, insomnia, anorexia, and chronic aspiration of stomach contents into the respiratory tract. Signs of chronic aspiration: cough, hoarseness, sore throat.
Distal reflux esophagitis may be accompanied by:
- pain when swallowing;
- esophageal bleeding;
- pain in the chest area;
- an unpleasant taste in the mouth that does not go away even after brushing your teeth.
Due to constant throat irritation, patients with GERD may develop chronic pharyngitis or laryngitis. At the same time, symptoms characteristic of the listed diseases are added (pain when swallowing, swelling of the throat, intoxication).
Symptoms
It is advisable to begin treatment of reflux disease as early as possible, otherwise its manifestations can cause many problems. When the contents of the stomach (and this includes food, digestive enzymes, and hydrochloric acid) enter the esophagus, its mucous membrane is irritated, inflammation begins, and GERD occurs. Symptoms and treatment in this case are typical for many esophageal disorders. So, the signs of the disease are usually the following:
- heartburn - a burning sensation in the area behind the sternum;
- hoarseness and cough - with GERD, treatment of such manifestations is carried out by taking prokinetics, and they occur already when reflux reaches the vocal cords and larynx and causes their inflammation;
- pain behind the sternum - usually felt after eating rough food;
- bleeding from the veins of the esophagus - this symptom can be observed if complications develop in the form of ulcers or erosion. If the bleeding is small, blood is usually found in the stool, and the stool itself turns black; if it is massive, blood comes out of the mouth.
In addition to esophageal symptoms, GERD also manifests itself extraesophageal. These are digestive disorders (flatulence, abdominal pain, nausea); pathologies of the pharynx and oral cavity (caries, sore throat, destruction of tooth enamel); damage to the ENT organs (polyps of the vocal cords, rhinitis, laryngitis, otitis media); damage to the respiratory system (pneumonia, bronchial asthma, bronchitis, emphysema, bronchiectasis); ailments of the cardiovascular system (angina pectoris, arrhythmia, arterial hypertension).
GERD: Algorithm of treatment tactics
Vladimir Trofimovich Ivashkin , academician of the Russian Academy of Medical Sciences, Doctor of Medical Sciences:
– We are moving on to our next series of lectures. And now Tatyana Evgenievna Polunina will tell us about the algorithm of treatment tactics in patients with gastroesophageal reflux disease.
Tatyana Evgenievna Polunina , professor, doctor of medical sciences:
– Dear Vladimir Trofimovich, dear colleagues! The presentation will present: epidemiology, pathophysiology, clinical manifestations, classification, diagnosis and modern treatment algorithm for gastroesophageal reflux disease. Particular attention will be paid to the modern three-step approach to the treatment of gastroesophageal reflux disease, according to which a rational choice of drugs is proposed.
Gastroesophageal reflux disease is a chronic, relapsing disease that is potentially dangerous due to its complications. About 40% of the world's adult population regularly experience heartburn. But gastroesophageal reflux disease appears as an iceberg. At the top are the symptoms, in particular heartburn, and at the bottom is a real iceberg, which can manifest itself in other clinical manifestations. In particular, these are bronchospasm, chest pain, obstruction, laryngitis, and so on.
In the epidemiology of acid-related diseases in the last millennium, you see an increase in gastroesophageal reflux disease, aka, esophageal carcinoma. And this explains such close attention to this nosology. According to Igor Veniaminovich Maev and Professor Trukhmanov, the constituent forms of gastroesophageal reflux disease include the non-erosive form - 68%, erosive esophagitis - 37% and Barrett's esophagus, a formidable complication of gastroesophageal reflux disease, is 3%.
GERD is a disease that reduces quality of life and is associated with the release of acidic contents from the stomach into the esophagus. The prevalence of GERD is widely underestimated. Some researchers suggest that GERD affects about 50 million people in Europe and 21 million people in the United States.
Extraesophageal manifestations of gastroesophageal reflux disease are very often a bronchopulmonary pathology, which is manifested by a dry cough, attacks of difficulty breathing, hoarseness, and an unpleasant taste. Laryngological symptoms and, accordingly, cardiological ones will be discussed in more detail in the next slide.
But the main factors in the formation of gastroesophageal reflux disease are decreased motility of the esophagus, decreased pressure of the lower esophageal sphincter, reflux of acid, pepsin, bile acids, slower gastric emptying from solid foods and impaired motility of the antrum of the stomach. Great importance is currently attached to the acid pocket, which is very important for the reflux of acid from the stomach, namely from the cardiac part of the stomach into the esophagus. It's presented here. A hiatal hernia complicates the course of gastroesophageal reflux disease. And this option always requires special endoscopic control.
This slide presents the symptoms. Heartburn is a key symptom, pain behind the breastbone, regurgitation, pain when passing food down the esophagus (odynophagia), feeling of a lump in the throat (dysphagia), bad taste in the mouth, persistent dry cough, hoarseness of the voice, episodes of difficulty breathing, rapid heartbeat and arrhythmia. With such symptoms, patients come not only to a gastroenterologist or therapist, but also to pulmonologists, ENT specialists, and cardiologists. And it is very important to have contacts with specialists in related specialties, because it is these symptoms that in some cases cause problems for pulmonologists, in particular dry cough, who cannot find out the cause. And accordingly, diagnostics are carried out to find out the true cause.
You see that heartburn ranks first according to statistics. Both hoarseness and cough are 4-7%, flatulence, sleep disturbance, indigestion, chest pain, nausea, sore throat, epigastric pain - this is the situation that is typical for patients with gastroesophageal reflux disease. Here are the epidemiological criteria of the Mail Clinic, which are fundamental in all epidemiological studies, in particular 15 clinical studies: 1 time per month is considered rare symptoms, but 1 time per week heartburn is the equivalent of gastroesophageal reflux disease. And if it repeats within 12 months, then it is clinically possible to make a diagnosis of gastroesophageal reflux disease.
“Masks” of GERD, about which we have already said that there is a pseudocardial form, ENT pathology, otology, bronchopulmonary and gastroenterological, so to speak, the main form. They are presented on this slide. Many faces. I would like to draw your attention to the presence of the Los Angeles endoscopic classification, which is key and is used in the Russian Federation and other countries.
In particular, by stages. You see. Grade A is one lesion (or more) of the mucous membrane, which is limited to the folds, and the length is 5 millimeters. Grade B is a damage of more than 5 millimeters, grade C - naturally, this lesion extends to two or more folds of the mucous membrane, but occupies less than 75%. And grade D is damage to the mucous membrane, which extends to 75% or more.
The Montreal Gastroenterology Consensus, which was held in 2005, proposed dividing gastroesophageal reflux disease into esophageal syndromes and extraesophageal syndromes. Esophageal syndromes without damage to the esophagus are a typical reflux syndrome and, accordingly, reflux chest pain syndrome. With damage to the esophagus, these are refluxoesophagitis, esophageal stricture, Barrett's esophagus and esophageal adenocarcinoma.
But extraesophageal symptoms, when a connection is established with gastroesophageal reflux disease, are just cough, reflux asthmatic syndrome, laryngitis, erosion of tooth enamel. The alleged connection with GERD is pharyngitis, sinusitis, recurrent otitis media, idiopathic pulmonary fibrosis.
Complications of gastroesophageal reflux disease are esophageal strictures. In particular, Barrett's esophagus is one of the most dangerous complications. And you see: here is the morphological shape of Barrett's esophagus with a normal esophagus, and how the edges of the velvety red mucosa are clearly defined, which is located on the pale mucosa of the esophagus, which the endoscopist has the right to place simply by visual inspection.
Barrett's esophagus is an acquired condition that is a complication of gastroesophageal reflux disease and is the replacement of stratified squamous epithelium with non-cylindrical epithelium with the phenomenon of intestinal metaplasia. It is a precancerous condition and occurs in 6-12% of patients with symptoms of gastroesophageal reflux disease. And most often - in 90-95% of cases - it is not diagnosed. Most often, this option in good clinics is established using not only endoscopic examination and chromatin staining, but also with NBI radiation, which is carried out during the examination. Most often this is 1% of the population.
Among patients, the age group of Barrett's esophagus, you see, begins to increase in patients from 50 years of age. It is dominated by men most often. But I want to say that from the age of 30 there is already a decent increase in statistics for Barrett's esophagus at the present time, and these data are currently being discussed. Because the sudden development of Barrett's esophagus is a very important point that requires monitoring.
Endoscopic classification is presented on this slide. You can see that there are both short segments and long segments in Barrett's esophagus, depending on the degree of damage to the mucous membrane and the length of the lesion, which is presented here on this slide.
Symptoms. There are no specific symptoms. These are frequent and prolonged attacks of heartburn, usually more than five years, dysphagia, nausea, chest pain. But weight loss (because food causes discomfort and pain) occurs quite often. During endoscopy, the columnar intestinal epithelium has a specific red color and “velvet” appearance. Easily distinguished from the thin, pale, glossy-surfaced normal squamous epithelium of the esophagus.
I would like to show you the film. Endoscopically - you can see here the length of the tongue damaging the esophagus. It is very important to pay attention to the edges of this tongue, measure the length, and take a biopsy in the required place. Biopsies are taken in five different locations. The location of the biopsy must be determined - this is a very important point. And you see different versions of Barrett's esophagus, which are presented here on microfilm. And, accordingly, different stages of damage and different species positions that endoscopists observe. They definitely record this on camera and take a biopsy from the edge.
Chromoesophagogastrography can be performed with methylene blue, and it is actively absorbed by the intestinal epithelium, “staining” areas of intestinal metaplasia. This is very important, because metaplasia can be of the large or small intestinal type, or complete or incomplete, which indicates different morphological stages. Metaplasia is a concept that is very important and includes the persistent replacement of differentiated cells of one type with differentiated cells of another type while maintaining the main species of the tissue. Metaplasia is a relatively benign change in tissue structure in response to chronic physical or chemical irritation.
Here is a goblet cell - a sign of intestinal metaplasia. It is a very important element. Accordingly, the count of goblet cells, as well as the structure of the epithelium, is a stage of dysplasia. And the histological stages of Barrett’s esophagus are necessarily indicated in the morphological protocol, because the patient’s management tactics depend on this; observation is necessarily indicated. Here in the first picture - there is no dysplasia. And a low degree of dysplasia, which implies a low number of goblet cells and, accordingly, small intestinal metachondria, is a fairly common option. And a high degree of dysplasia, which implies a large number of goblet cells and requires monitoring very clearly once every three or six months.
Suppression of clinical manifestations of gastroesophageal disease is the goal of treatment of Barrett's esophagus. Healing of erosive esophagitis, prevention of the development of adenocarcinoma.
Here is an algorithm for the diagnosis and treatment of gastroesophageal reflux disease, which was presented in Switzerland in the city of Stadt by an expert who deals with gastroesophageal reflux disease, is a new European treatment algorithm and it is based on three stages. Three stages: self-medication, treatment with a general practitioner and a specialist. I would like to point out that episodic symptoms of heartburn, which can be treated with over-the-counter drugs, such as antacids, in particular Maalox, alginates, and only then drugs from the group of proton pump inhibitors, in some cases histamine H2 blockers, are added. This is a situation that comes out at the stage of self-medication. Accordingly, if treatment is effective, it continues. If the symptoms cause concern, then you should consult a general practitioner. Alarming symptoms: dysphagia, bleeding, anemia, weight loss, suffocation, chest pain, frequent vomiting - these are moments of alarming symptoms, which, of course, require contacting a gastroenterologist.
A consultation with a therapist implies optimization and the inclusion in the first place not of antacids, but of proton pump inhibitors, which are long-acting drugs that block the secretion of hydrochloric acid. And in addition to the combination, drugs from the group of antacids are included, in particular Maalox, alginates, and the duration of this treatment is from 4 to 8 weeks. If this is a confirmed diagnosis of gastroesophageal reflux disease.
If treatment is effective, step therapy followed by discontinuation at relapse is therapy that requires tapering after 4 to 8 weeks at the lowest effective dose. If the treatment is ineffective, the dose of inhibitors is increased - not once, but twice a day and, accordingly, antacid drugs are prescribed for at least four weeks, with a re-examination and the doctor’s decision on patient management tactics. An alternative diagnosis in the absence of effectiveness should be considered and the presence of alarming symptoms requires referral to a gastroenterologist.
An appointment with a gastroenterologist, of course, optimizes therapy based on the results of the examination. Endoscopy is a mandatory test. And for non-erosive gastroesophageal reflux disease or gastroesophageal reflux disease, class A and B, respectively, include the duration of treatment, which depends on 4-8 weeks, respectively. Both class C and D are 8 weeks. Accordingly, the issue of the duration of maintenance therapy is decided depending on the effectiveness of treatment, and proton pump inhibitors in some cases are prescribed from 3 to 6 months on demand.
I would like to say that this algorithm does not imply pathogenetic treatment, but symptomatic treatment. And unlike previous algorithms, much attention is paid to drugs from the antacid group, because in this situation they are very important drugs that improve compliance.
Well, diet and lifestyle are very important points. In particular, the harmful effects of smoking should be excluded, hot and cold foods should be excluded; avoid the consumption of acidic foods, tangerines, sour fruits, foods that increase gas formation, Coca-Cola, coffee, carbonated drinks, excess fat, chocolate, spices. In particular, garlic, onions, peppers, and other spicy foods. Avoiding alcohol, especially carbonated alcohol, is also an important point; red wine is a risk factor for the development of gastroesophageal reflux disease. You should not eat several hours before bedtime or overeat. Normalizing body weight is key. And to reduce the intensity of reflux, moderate elevation of the head of the bed at night is recommended. Avoid straining the abdominal muscles, bending over, and wearing tight belts that provoke reflux. Do not assume a horizontal position after eating or eating various foods.
Regarding antacids, I would like to draw your attention to drugs from the group of combined antacids, in particular Maalox, which is capable of neutralizing hydrochloric acid, adsorbing pepsins, bile acids, and lysolecithins. And thus potentiates the cytoprotective properties on the mucous membrane. Pay attention to the safety of taking the drug, which is very important, which does not affect motor skills and does not cause electrolyte disturbances, which has been proven in a number of studies by Russian and foreign authors.
I would like to draw your attention to the fact that Maalox is a drug that has been used for quite a long time. And the work of Vladimir Trofimovich Ivashkin on the study of these properties of the drug, Trukhmanov, Maev, our famous gastroenterologists, who confirmed that magnesium and aluminum hydroxide are active components, which in interaction also have a rapid action and a delayed prolonged action of up to 3.5 hours. The acid-binding ability of this drug is much higher than its competitors, in particular calcium carbonate, magnesium oxide, sodium bicarbonate and other drugs.
Maalox has a cytoprotective effect, but one must understand that one drug will not be able to relieve heartburn in patients with gastroesophageal reflux disease and erosive esophagitis. Therefore, in an open multicenter study that was conducted, in particular published in clinical gastroenterology, I would like to draw attention to the fact that the combination with a proton pump inhibitor - Rabeprazole, Omeprazole, Esomeprazole, Lanso- and Pantoprazole - naturally, the compliance of these drugs is much higher if we We have a combination of these medications, therefore rapid healing of erosion. Effective prevention and therapy of other acid-related diseases, in particular stress-induced ulcers, are points that are very important to consider. And the rational use of drugs in the arsenal of treatment of gastroesophageal reflux disease and acid-related diseases requires, of course, a combination of these drugs.
In conclusion, I would like to say that by rationally using the capabilities of modern antacids in the treatment of non-erosive reflux disease, the doctor provides neutralizing, adsorbent and cytoprotective effects, significantly increasing the quality of life of patients. According to modern research and accumulated experience, for gastroesophageal reflux disease, monotherapy with antisecretory drugs is not always sufficient. And in most cases, it is impossible to completely relieve the symptoms of GERD without the use of antacids, one of which is the drug Maalox. As a means of pathogenetic therapy for GERD, it can be used for a long time (2-3 months). Its use gives a quick effect when we cannot quickly stop heartburn with proton pump inhibitors.
In conclusion, I would like to say that GERD has many faces. We have various manifestations and various specialties, in particular in pulmonology, cardiology, ENT specialists are currently focused on the fact that the symptoms associated with the “masks” of GERD are always very important and they can be relieved with drugs that are available not only to gastroenterologists, but also doctors of various specialties.
Diagnostics
Until GERD is diagnosed by a gastroenterologist, there is no point in starting treatment, because treatment methods should be selected based on the characteristics of the pathological process. To identify reflux disease and determine the mechanism of its development, the following methods are used:
- X-ray of the esophagus. With such a study, erosions, strictures, ulcers, and hernias can be detected.
- Endoscopy of the esophagus. This procedure also reveals inflammatory changes.
- Scintigraphy with radioactive technetium. The study involves taking ten milliliters of egg white with Tc11: the patient takes sips of this drug every twenty seconds, and at this time a picture is taken on the halo-chamber every second for four minutes. This method makes it possible to assess esophageal clearance.
- Manometric examination of the esophageal sphincters. This procedure allows you to detect changes in sphincter tone.
- Monitor pH in the lower esophagus. Such a study is necessary in order to select individual therapy and monitor the effectiveness of medications.
Complications of GERD
Gastroesophageal reflux disease can lead to the development of many dangerous complications. The most common complications are:
- chronic esophagitis;
- peptic ulcer of the esophagus;
- esophageal strictures;
- Barrett's esophagus;
- adenocarcinoma of the esophagus.
Especially often, patients with advanced forms of GERD encounter Barrett's esophagus syndrome. Abnormal columnar epithelium appears in the lower esophagus. Complications can be provoked by: lack of treatment for GERD, asymptomatic course of the disease, old age over 50 years. Barrett's esophagus has no specific symptoms. It is diagnosed during endoscopy with a biopsy of the esophageal mucosa.
GERD can cause narrowing of the esophagus as a result of scarring of the damaged lining. This complication develops mainly in older people with a long course of reflux disease. It is treated through surgery, during which an endoscopic dilation of the esophagus is performed.
GERD: treatment
The goal of therapeutic measures for this disease is to eliminate its symptoms, combat reflux and esophagitis, improve the quality of life, and prevent complications. Conservative therapy is most often used; surgical treatment of GERD is indicated only in extreme cases. Let's take a closer look at ways to combat the disease. The set of activities includes:
- adherence to a diet and a certain lifestyle;
- taking antacids, antisecretory drugs and prokinetics.
Recommendations for diet and regimen
Regardless of the stage and severity of GERD, treatment involves constant adherence to certain rules:
- Do not lie down or lean forward after eating.
- Do not wear tight clothes, corsets, tight belts, bandages - this leads to an increase in intra-abdominal pressure.
- Sleep on a bed in which the part where the head is located is raised.
- Do not eat at night, avoid large meals, do not eat too hot food.
- Quit alcohol and smoking.
- Limit consumption of fats, chocolate, coffee and citrus fruits, as they are irritating and reduce LES pressure.
- Lose weight if you are obese.
- Stop taking medications that cause reflux. These include antispasmodics, β-blockers, prostaglandins, anticholinergic drugs, tranquilizers, nitrates, sedatives, calcium channel inhibitors.
GERD: classification and features of different forms
There are two main forms of GERD:
- Non-erosive - the most common, characterized by swelling and inflammation of the esophageal mucosa, but does not lead to the formation of wounds.
- Erosive - leads to the appearance of ulcers and erosions on the surface of the esophageal mucosa under the influence of an aggressive gastric environment.
The Los Angeles classification distinguishes the following degrees of GERD:
- A – one damage to the mucosa, limited to the esophageal folds, with a diameter of no more than 5 mm;
- B – one or more lesions of the mucous membrane, limited to the esophageal folds and not merging with each other, with a diameter of more than 5 mm;
- C – numerous lesions of the mucous membrane, occupying less than 70% of the circumference of the esophagus;
- D – numerous confluent lesions of the mucous membrane of the esophagus, occupying over 70% of its circumference.
Medicines for reflux disease. Antacids and alginates
Such drugs for the treatment of GERD are used when manifestations of the disease are moderate and infrequent. Antacids should be taken after each meal (after one and a half to two hours) and at night. The main drug from this group is “Almagel”. Alginates create a thick foam on the surface of the stomach contents and, due to this, return to the esophagus with each episode of reflux, thereby providing a therapeutic effect. Due to the content of antacids, alginates produce an acid-neutralizing effect, at the same time they form a protective film in the esophagus, which creates a pH gradient between its lumen and the mucosa and thus protects the mucosa from the negative effects of gastric juice.
Modern treatment of gastroesophageal reflux disease
Treatment for GERD is aimed at combating symptoms and preventing consequences. It can be conservative and medicinal. First, doctors suggest the patient try to change their lifestyle:
- get rid of excess weight;
- switch to a normal regime of wakefulness and rest;
- give up bad habits (smoking, alcohol);
- switch to a balanced, gentle diet.
Diet is the main method of non-drug treatment of GERD. You need to eat small portions 5 times a day. It is recommended to avoid evening overeating (the last meal should be at least 2 hours before bedtime). You need to include more vegetables in your diet. Meat should be consumed after boiling or steaming. Spices, fatty foods, fried foods, carbonated drinks, and sour fruits are excluded from the diet. Dishes should not be too hot or cold.
Patients should avoid situations that increase abdominal pressure. You cannot wear tight trousers, belts, corsets, sweaters, or bandages. It is not recommended to jump, lift weights, or perform intense exercises that strain the abdominal muscles. Ideal sports for people with GERD: swimming, cycling, walking.
If heartburn attacks occur only when lying down, it is recommended to raise the head of the bed or choose a larger pillow. You should not lie down immediately after eating or drinking.
The patient will have to give up medications that can provoke attacks of GERD. Such drugs include:
- nitrates and nitrate-like agents;
- nifedipine, Theophylline, Progesterone;
- antidepressants and antispasmodics;
- non-steroidal anti-inflammatory drugs.
If symptoms of GERD persist, you need to switch to drug therapy. Help to get rid of the manifestations and complications of the disease:
- drugs from the group of proton pump inhibitors;
- combined antacids;
- dioctahedral smectite;
- prokinetics.
Drug treatment for GERD lasts from 4 to 8 weeks. After the main course, you need to undergo maintenance therapy lasting 6-12 months.
Complicated and advanced forms of GERD are treated surgically. To correct a defect in the esophagus, antireflux surgery is performed. In case of a hiatal hernia, a fundoplication is prescribed - suturing the stomach to the diaphragm around the opening of the esophagus, thereby creating a cuff that regulates the passage of food.
Prokinetics
These drugs restore the normal physiological state of the esophagus by increasing the tone of the lower sphincter, improving clearance and enhancing peristalsis. The main means of pathogenetic therapy for GERD is the prokinetic drug Motilium. It normalizes the motor activity of the upper digestive tract, restores active gastric motility and improves antroduodenal coordination. Motilium is well tolerated when long-term therapy is necessary and reduces the percentage of disease relapses.
Pathophysiology
The content of the article
Under normal conditions (in a healthy person), the contents of the gastric juice with high acidity periodically enter the esophagus, but internal protective mechanisms either reduce the amount of acid secreted to a minimum or remove the acid, which is quickly removed by “cleansing” the esophagus. Therefore, symptoms of acid irritation of the esophagus are not felt or are minimal.
Mechanisms that protect the esophagus from stomach acid include the lower esophageal sphincter (sphincter) and normal esophageal motility (motility). When these mechanisms are disrupted, reflux occurs and symptoms of GERD occur.
Gastroesophageal reflux
Proton pump inhibitors
If GERD with esophagitis is diagnosed, treatment with prokinetics is carried out in combination with proton pump inhibitors. As a rule, the new generation drug “Pariet” is used. Due to its use, acid secretion is reduced, and there is a positive dynamics in the clinical manifestations of the disease. Patients report a decrease in the intensity or even complete disappearance of heartburn, and a decrease in pain. For GERD, the treatment regimen with prokinetics and proton pump inhibitors is as follows: 20 milligrams of the drug “Pariet” and 40 milligrams of the drug “Motilium” are prescribed per day.
Antisecretory drugs, H2 receptor blockers
This is the first-line treatment for mild to moderate GERD and grade I-II esophagitis. Four H2 blockers are commonly used in clinical practice: ranitidine, famotidine, cimetidine, and nizatidine. They are more effective in suppressing unstimulated secretion of gastric juice with food and are therefore recommended on an empty stomach or at night.
H2 blockers are effective in the treatment of mild esophagitis (70-80% of patients recover), as well as in antirecessive treatment and prevention of relapses. The effectiveness of H2 blockers decreases with long-term use, leading to tachyphylaxis. An H2 blocker is recommended for patients suffering from nocturnal reflux symptoms, especially in Barrett's temple.
Therapy for young children
In babies, reflux causes frequent burping. Treatment consists of several stages:
- Postural therapy. You need to feed the baby in a sitting position, holding him at an angle of 45-60 degrees. At the end of feeding, this position must be maintained for another twenty to thirty minutes, after which the baby can be placed on his back, with his head elevated at an angle of 30 degrees.
- Dietary correction. It is recommended to reduce the child’s daily feeding volume, while increasing the total number of feedings. If breastfeeding is carried out, the mother should take breast milk thickeners. Formulas containing gum, such as Nutrilon AR, Nutrilak AR, Humana AR, or rice starch, such as Enfamil AR, are recommended for bottle-fed infants.
- Treatment of GERD in young children is also not complete without taking prokinetic drugs (Motilium, Motilak, Cerucal), antacids (Phosphalugel) and antisecretory drugs (Losec). The dosage should be selected only by a specialist.
Therapy in older children
Correcting the child’s lifestyle is of great importance in the treatment of reflux disease.
- The end of the bed, where the head is located, should be raised by at least fifteen centimeters. This simple measure can reduce the duration of acidification of the esophagus.
- It is necessary to introduce dietary restrictions for the child: reduce the fat content in the diet and increase the protein content, reduce the amount of food consumed, exclude irritating foods (citrus juices, chocolate, tomatoes).
- It is necessary to develop the habit of not eating at night and not lying down after eating.
- It is necessary to ensure that the child does not wear tight clothes or sit bent over for a long time.
As a drug treatment, as in adults, antacid drugs are used, usually in the form of a suspension or gel (Almagel, Phosphalugel, Maalox, Gaviscon), prokinetic agents (Motilak, Motilium) , "Cerucal"). The choice of a specific medication and determination of the dosage is carried out by the attending physician.
Surgical intervention
Sometimes, to restore normal function of the cardia, it is necessary to resort to surgery aimed at eliminating reflux. Indications for surgical treatment are as follows:
- complications of GERD (repeated bleeding, strictures);
- ineffectiveness of conservative therapy;
- frequent aspiration pneumonia;
- diagnosing Barrett's syndrome with high-grade dysplasia;
- the need of young patients with GERD for long-term antireflux therapy.
Reflux is often treated by fundoplication. However, this method is not without drawbacks. Thus, the result of the operation entirely depends on the experience of the surgeon; sometimes after surgery there remains a need for drug treatment, there is a risk of death. Currently, various endoscopic techniques have been used to influence foci of metaplasia: electrocoagulation, laser destruction, photodynamic destruction, argon plasma coagulation, endoscopic local resection of the esophageal mucosa.
Therapy with folk remedies
In the initial stages of GERD, alternative treatment can be very helpful. In general, at these stages you can cope with the disease simply by following an antireflux regimen and changing your lifestyle. If the disease is mild, instead of antacids to relieve heartburn, you can use various traditional medicines that strengthen and protect the esophageal mucosa, improve sphincter tone and reduce the acidity of gastric juice. In severe cases of the pathological process, it will not be possible to do without drug therapy, and in the presence of complications, surgical intervention is generally required. Therefore, treatment of GERD with folk remedies is rather an auxiliary and preventive method. It can be used as a complement to highly effective drug therapy regimens. Herbal medicine is very popular among people. Here are several traditional medicine recipes for the treatment of reflux disease.
- combine crushed dry herb yarrow (20 grams), St. John's wort (20 grams), celandine (10 grams) and chamomile (20 grams). Pour a tablespoon of the mixture into a glass of boiling water and leave for fifteen minutes. Take the strained solution one to two glasses per day;
- mix calendula flowers (20 grams), chamomile flowers (5 grams), coltsfoot leaves (20 grams). Pour two tablespoons of the mixture into a glass of boiling water and leave for thirty minutes. Take the strained infusion before meals (twenty minutes before) one tablespoon three or four times a day;
- combine St. John's wort herb (20 grams), chamomile flowers (5 grams), plantain leaves (20 grams). Pour two tablespoons of the mixture into a glass of boiling water and leave for thirty minutes. Take the strained decoction before meals (twenty minutes before) one tablespoon three or four times a day;
- pour two tablespoons of flax seeds with two glasses of boiling water and leave for eight hours. Take the strained infusion before meals, half a glass three to four times a day for five to six weeks;
- squeeze the juice out of potatoes and take it before meals (twenty minutes before) a quarter glass four times a day for three weeks;
- Fry the buckwheat until it turns dark brown. Crush the resulting mass into powder and use a pinch three or four times a day;
- You can quickly stop heartburn by chewing a piece of horse sorrel or calamus root. These plants have the ability to reduce the acidity of gastric juice and thus reduce its damaging effect on the esophageal mucosa. Also, horse sorrel and calamus protect the mucous membrane from the harmful effects of hydrochloric acid.
New antacids and antirefluxants
Alginic acid salts have been used clinically to relieve symptoms of heartburn and esophagitis for over 30 years. Alginic acid salts have a unique mechanism of action: when interacting with gastric acid, alginates precipitate and form a gel that covers the esophageal mucosa with a protective layer and promotes its restoration.
In vitro and in vivo studies have shown that alginates combine carbon dioxide and some antacid components. Recent kinetic studies have shown that alginates bypass acidic contents and reach the esophagus before the esophageal contents, protecting the organ mucosa from mechanical and chemical irritation from hydrochloric acid. According to clinical studies, alginates also act as a physical barrier, thereby more effectively suppressing reflux.
Alginate products contain antacids, which are acid neutralizing agents that reduce heartburn, but studies have not shown that the effectiveness of these combination drugs depends on their neutralizing properties.
The clinical effectiveness of alginate preparations depends on many factors: the amount and penetration of carbon dioxide released, the characteristics of the molecule, additional ingredients (aluminum, calcium) that have a positive potentiating effect.
Alginate preparations remain in the stomach for several hours, so they last significantly longer and are more effective in suppressing the symptoms of GERD than traditional antacids, they begin to work quickly and last a long time. Alginate preparations are completely safe and are therefore used to reduce the symptoms of reflux in infants, children and pregnant women.
For example, one of these magnesium alginate preparations, Refluxaid, is used in European countries to reduce the symptoms of reflux and acidosis in GERD, peptic ulcers, esophagitis, functional dyspepsia, and other functional and inflammatory diseases of the gastrointestinal tract, manifested by heartburn, reflux, and epigastric discomfort.
Refluxaid drug
The magnesium alginate in Rexluxaid is a natural substance extracted from seaweed. The drug has a high viscosity, which increases anti-reflux effectiveness and duration of action. It has emulsion and swelling properties.
Studies have shown that the highly viscous compound Refluxaid, when ingested into the stomach, creates a physical barrier that binds and neutralizes gastric juice, thereby protecting the esophagus from symptoms of reflux: heartburn, burning behind the sternum, chest pain, epigastric discomfort, etc. Taking these The medication reduces heartburn, acid regurgitation, dysphagia and odynophagia (difficulty swallowing and pain) are reduced, and extrazophaginic symptoms of GERD are also suppressed - cough, hoarseness.
Refluxaid is a prescription medication. It is used for episodic relief of symptoms of acidosis, reflux and esophagitis, on demand or in combination with anti-reflux medications (antisecretory PPIs, H2 blockers, prokinetics).
It has been found that when a person sleeps, magnesium alginate can remain in the stomach for up to 8 hours without breaking down—enough time for the patient to get a good night's sleep. Taking reflux before bed may improve the quality of sleep in a patient with GERD because the symptoms caused by nocturnal reflux will be suppressed.