Colonoscopy is a diagnostic method that is used to assess the condition of the colon mucosa. The examination is carried out using a special instrument - a colonoscope. It is a thin flexible tube with a video camera at the end. The colonoscope is inserted into the intestines through the anus.
- Execution Goals
- Preparing for a colonoscopy
- Diet before colonoscopy
- Indications and contraindications
- Diagnostic colonoscopy
- Therapeutic manipulations during colonoscopy
- Colonoscopy in a state of medicated sleep
- Methodology
- Recording the procedure on video
- Recovery after colonoscopy
- Possible complications
- Alternative diagnostic methods
- Colonoscopy results
Execution Goals
Using a colonoscope, the doctor can detect ulcers, polyps, foci of inflammation, tumors, and sources of intestinal bleeding. In addition, during the study it is possible to obtain tissue samples from the intestines for histological and cytological examination, as well as to remove polyps or other formations.
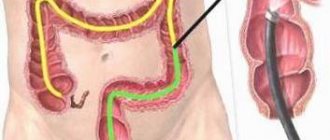
Colonoscopy, diagram
It is recommended to have your first colonoscopy at age 50. Further recommendations are given individually, depending on the results of the study. Unfortunately, most colon tumors are detected at late stages. There is only one reason here - late diagnosis of the tumor. The only way to detect a tumor at an early stage is regular examination of the colon, which allows us to identify pre-tumor pathology and remove it, or carry out other necessary treatment so that it does not degenerate into cancer. The key to curing colon cancer is early diagnosis. Early diagnosis can be achieved using endoscopy. [1]
Colonoscopy and disease diagnosis
Colonoscopy makes it possible to assess the condition of the intestines from the inside, examine its mucous membranes, assess tone and other indicators. In some cases, the procedure allows you to avoid abdominal surgery. During its implementation, polyps can be removed, and a biopsy of altered tissues can be performed for further examination.
Diseases that require a colonoscopy:
- Diverticular disease.
With diverticulosis, there is a protrusion of the intestinal wall. The diverticula themselves resemble “sacs”. Translated from Latin, this term means “road to the side.” Feces accumulate and stagnate in these bags, which leads to the development of inflammation. Over time, the intestinal wall becomes thinner and becomes damaged, which leads to bleeding and even perforation. At first, the disease occurs without obvious symptoms; more than 80% of patients are not even aware of its development. Ultrasound for diverticulosis does not provide the necessary information. Pathology can be detected using colonoscopy, CT or irrigoscopy.
- Polyps and polyposis.
Polyps are benign neoplasms that have the ability to degenerate. Such tumors must be removed and further studied. Polyps most often do not show themselves, although they may bleed. When they reach large sizes, a person experiences abdominal pain.
If a patient is diagnosed with familial polyposis, accompanied by the appearance of a large number of tumors, resection of part of the intestine may be required. Polyps can be visualized during an MRI or CT scan. However, only with the help of colonoscopy the doctor has the opportunity to remove them, or take part of the tumor for further histological examination.
- Ulcers.
Colonoscopy can detect even the smallest areas of damage to the intestinal mucosa.
- Colon cancer.
Colon cancer is the third leading cause of death among other cancers. The causes of tumors can be identified only in 1/4 of the patients. Patients with a hereditary predisposition are at risk. If the cancer has an advanced course and metastases to the liver, then no more than 0.1% of patients survive over the next 5 years. When a tumor is detected at stage 3 of development, no more than 1/4 of people reach the five-year survival threshold.
If a tumor is detected at an early stage of development, the prognosis is most often favorable. Thus, detecting first-degree cancer can save the lives of 93% of patients. Colonoscopy can detect adenocarcinomas and other cancers in the early stages of development, perform a biopsy, and even remove some of them. The procedure is performed using a loop electrode.
- Nonspecific ulcerative colitis.
With this disease, inflammation of the intestinal wall occurs. It becomes covered with ulcers that bleed and secrete pus. The mild course of the pathology is characterized by redness of the intestinal mucosa, erosion and isolated areas of ulceration are visible on it. The vascular pattern is poorly expressed.
The severe course of the pathology is characterized by the presence of a large number of ulcers and areas of necrosis. A lot of pus and mucus are found in the intestinal lumen, there are areas of hemorrhage, and pseudopolyps and abscesses can form. All pathological changes can be detected during colonoscopy.
- Crohn's disease.
The disease is characterized by abdominal pain, severe diarrhea, and the appearance of anal fissures. The intestinal wall is thickened, reminiscent of a “cobblestone” appearance. These areas alternate with areas of ulceration, scar tissue, and fistulas. Crohn's disease can be diagnosed using a colonoscopy.
- Intestinal tuberculosis.
Intestinal tuberculosis develops in 70% of patients with pulmonary tuberculosis. Mycobacteria enter the intestines from the respiratory system. Diagnosis comes down to laboratory tests with a test for tuberculosis, X-rays of the intestine and colonoscopy with a biopsy of its tissue.
- Intestinal obstruction.
Colonoscopy allows you to clarify the nature of developing intestinal obstruction. Using a colonoscope, foreign bodies can be removed from the organ.
- Chronic colitis.
In chronic colitis, inflammation of the inner lining of the large intestine occurs. It undergoes degenerative processes. If the disease is advanced, then the walls of the organ suffer from atrophy.
Patients complain of abdominal pain, stool upset, nausea and loss of appetite.
Colonoscopy can detect the following types of disease:
- Typhlitis is a lesion of the cecum.
- Sigmoiditis is a lesion of the sigmoid colon.
- Proctosigmoiditis is a lesion of the rectum and sigmoid colon.
- Transversitis is a lesion of the transverse colon.
- Total colitis is a global lesion of the colon.
- Ischemic intestinal disease.
Ischemia and necrosis of intestinal tissue can develop in various diseases. This includes atherosclerotic vascular lesions, vasculitis, and vascular pathologies. Colonoscopy can be performed only according to strict medical indications, when the acute stage of the disease has passed. During the procedure, the doctor will find purplish-red areas, ulcers, hemorrhages, and strictures on the intestinal wall.
- Amyloidosis.
With amyloidosis, amyloid accumulates in the intestinal walls. This is expressed by abdominal pain, intestinal obstruction, constipation, and bleeding may develop. If the distal parts of the organ are affected, a colonoscopy with a biopsy of the changed tissue is required. Amyloid will be found in them.
- Pseudomembranous colitis.
Pseudomembranous colitis develops during long-term treatment with antibiotics. In this case, convex plaques with a yellowish tint will be visible in the intestines. They are an accumulation of fibrin, leukocytes and dead epithelium.
- Diverticula.
Saccular formations can form in a person throughout life, or be present from birth due to weakness of the connective tissue. When sick, a person complains of abdominal pain, diarrhea and increased gas formation. Colonoscopy is performed only after the disease has passed the acute stage.
Diet before colonoscopy
An important part of preparing for a colonoscopy is proper diet in the preceding days and on the day of the examination. In general terms, the recommendations are as follows:
- A few days before the procedure, you need to switch to a low-fiber diet, reduce the consumption of fresh vegetables and fruits, dried fruits, nuts, and whole grains.
- 1–3 days before and on the day of the procedure, you need to give up solid food. Broths, clear fruit juices (for example, clarified juice from apples, white grapes), tea and coffee, and jelly are allowed. It is recommended to drink more fluid the day before.
- You should not eat or drink anything 2–4 hours before the procedure The procedure can only be carried out under medicated sleep conditions on an empty stomach.
In parallel with the diet, in the afternoon before, the intestines are prepared for the procedure using laxatives. Recommendations regarding types of drugs and dosage regimens may vary from doctor to doctor. [2,3]
How to prepare properly:
Knowing what you can eat before a colonoscopy can provide better information. As a rule, start a diet
required
three days before the procedure
. Its essence is to rid the body of intestinal contents (discussed by many: toxins and toxic substances, disposal of harmful gas-forming products, dietary fiber, feces) and coloring substances that can distort the color of the mucous membrane, the image. In addition, a slag-free diet helps normalize stool, preventing the development of constipation, diarrhea, bloating and the formation of large feces that make it difficult to pass through the endoscope.
This medical procedure may be accompanied by discomfort in the lower abdomen due to excessive “bloating” with air, which is introduced through the endoscope, if there is “excess content” in the lumen. But maintaining the recommended diet before a colonoscopy can reduce discomfort by improving preparation without obstructing the view of the camera and the endoscope. If you suffer from constipation, you will need to talk to your doctor, who may prescribe a course of daily laxatives.
Indications and contraindications
Indications for colonoscopy are:
- blood and mucus in the stool;
- presence of relatives with colon cancer;
- previous colon surgery;
- chronic abdominal pain of unknown etiology;
- suspicions of cancer, ulcerative colitis, Crohn's disease;
- elevated temperature for a long period of time, accompanied by anemia and weight loss.
Regular colonoscopy is also recommended for all people over 50 years of age for the early detection of tumors, polyps and other diseases of the colon.
Contraindications to the study are the active stage of Crohn's disease or ulcerative colitis.
Diagnostic colonoscopy
A diagnostic colonoscopy is performed to identify certain pathological formations in the intestines. There are two special types of this study:
- A screening colonoscopy is recommended for all people over 50, even if they have no symptoms. For some bowel diseases, screening may need to start at a younger age. This type of screening is used for early diagnosis of polyps that can develop into a malignant tumor and intestinal cancer.
- Control colonoscopies are periodically performed in people with a history of polyps, colon cancer, and inflammatory bowel diseases. [1.4-6]
Intestinal polyps discovered during colonoscopy
Having discovered a pathological neoplasm in the intestine, the doctor removes it using a special instrument inserted through the colonoscope and sends it to the laboratory for histological and cytological examination. This procedure is called a biopsy .
The Euroonko clinics in Moscow and St. Petersburg are running a promotion for “Gastro- and colonoscopy under intravenous sedation.” The cost of the complex service includes endoscopic examinations of the stomach and colon, light anesthesia (sedation, “medicated sleep”), a preliminary appointment with a specialist (candidate of medical sciences or doctor of medical sciences), a three-hour stay in a comfortable room. More details about the program.
Who is it suitable for?
Colonoscopy under anesthesia is definitely performed if:
- Inflammatory processes occur in the intestines. Ulcers, colitis, enteritis are accompanied by pain; if the probe inaccurately touches the intestinal walls, this will cause too much discomfort to be ignored.
- The patient is less than twelve years old. It is difficult for the child to relax the muscles enough for the examination to be effective and produce results, in addition, pain during the process can be delayed and create unpleasant associations with hospitals in general.
- There are adhesions in the intestines formed by connective tissue. When air enters the intestine, this also provokes severe pain, which cannot be written off.
- The patient has a psychiatric diagnosis that will not allow him to sufficiently prepare, relax, and in some cases even understand what is happening.
- The patient has a low pain threshold and knows that the examination will be too unpleasant for him.
In a private clinic, a colonoscopy under anesthesia can be done simply at will, without indications.
Therapeutic manipulations during colonoscopy
During an endoscopic examination of the colon, the doctor may perform some therapeutic procedures:
- Remove polyp.
- Stop intestinal bleeding, for example, using electrocoagulation or clipping.
- Eliminate stenosis (narrowing of the intestinal lumen) caused by a malignant tumor or other causes. A special balloon is inserted into the narrowed area and inflated to expand the lumen, and then a stent is installed - a tube with a mesh wall made of metal or plastic (this procedure is called stenting ). [7,8]
Removal of an intestinal polyp during colonoscopy
During the work of the endoscopy department at Euroonko, more than a hundred endoscopic stenting of the colon was performed under the guidance of an endoscopist, Doctor of Medical Sciences Mikhail Sergeevich Burdyukov. This minimally invasive procedure helps restore intestinal patency in inoperable cancer.
Often, a colonoscopy is initially performed as a diagnostic procedure and, if pathological changes are detected, it becomes a therapeutic procedure.
Colonoscopy in a state of medicated sleep
Endoscopic examination of the intestine is usually painless, but the patient may experience discomfort from a feeling of bloating (this goes away immediately after the procedure) and the advancement of the probe through the loops of the intestine. In Euroonco clinics it is possible to carry out the procedure in a state of medicated sleep. In this case, the patient is given a special sedative, under the influence of which he is plunged into deep sleep. After approximately 40 minutes, the effect of the drug ends, and within 5-10 minutes after waking up the patient can walk and talk, and after an hour he can go home.
Types of anesthesia
In the standard version of the procedure, the probe itself is lubricated with an anesthetic. When it comes into contact with the intestinal walls, the medicine reaches them, is absorbed and reduces pain. However, if indicated or simply desired by the patient, anesthesia is used. It comes in two varieties:
- Medication sleep.
The safest way. The patient falls into a half-asleep, hears the doctor perfectly, retains the ability to follow his instructions, but experiences discomfort to a much lesser extent or does not experience it at all. The drugs are as modern as possible, the load on the body is small. - General anesthesia.
It puts a strain on the cardiovascular system, so it is not recommended for people with cardiovascular diseases and those who have recently suffered a stroke or heart attack. It has a negative effect on the lungs, so it is also not recommended for asthmatics and other patients. During general anesthesia, the patient is unconscious, does not experience any discomfort, and does not respond to any requests. After waking up, needs observation for at least 24 hours.
Before you determine which type is right for you, you will need to talk to an anesthesiologist and get tested.
Methodology
A diagnostic colonoscopy lasts on average 30 minutes. If therapeutic manipulations are required, the procedure time increases.
In order for the patient to undergo the procedure without pain and discomfort, sedation is used - the patient is immersed in a state of “medicated sleep”.
The patient must be completely undressed from the waist down. He is placed on his left side, with his legs bent and knees brought to his stomach. The doctor lubricates the colonoscope with Vaseline, carefully inserts it through the anus and slowly advances it, examining the intestinal mucosa. In this case, the intestines are inflated with gas to provide a better view. At Euroonko, carbon dioxide is used for this, because it acts as an antispasmodic, is absorbed through the intestinal walls faster than oxygen and nitrogen and is excreted from the body.
The image from the colonoscope camera is transmitted to the device screen. Videos of the study are recorded and saved on a computer.
After the intestines are examined, the doctor carefully removes the colonoscope. The study is completed.
Recovery after colonoscopy
Hospitalization is not necessary, and colon endoscopy can be performed on an outpatient basis. The patient can leave the clinic as soon as he recovers from anesthesia. But you are not allowed to drive on your own on this day. You need to take one of your relatives to the clinic so that you can be escorted home.
Notes and recommendations regarding the recovery period after the procedure:
- When the effect of sedation wears off, a feeling of cramping and fullness of the intestines may appear. It will soon pass. To help the gas leave the intestines faster, it is recommended to walk.
- For 24 hours after the procedure, you should avoid drinking alcohol, driving vehicles, and doing work that requires concentration.
- Unless otherwise advised by your doctor, you can begin eating as usual immediately after the sedation ends. A special diet is prescribed after removal of polyps and other surgical procedures.
- It is recommended to rest for one day after the study, then you can do all your usual activities without restrictions, and go to work.
- If a biopsy was performed during the test, you may notice small amounts of blood in your stool for 1–2 days afterward.
- If you need to take blood clot preventative or other medications continuously, ask your doctor how long after your colonoscopy you can start taking them again.
- Since your bowels have been cleansed, another bowel movement may occur within a few days. It depends on your diet. If you do not have stool for a very long time after the procedure, consult your doctor.
You should immediately seek medical help if symptoms such as high fever, bleeding from the anus, or abdominal pain appear.
Day before the procedure
The patient’s proper morning during this period should begin with a light breakfast. It can be semolina porridge, yogurt, cottage cheese. You can first drink a glass of clean water, and 15 minutes after that you can start eating. After breakfast and until the completion of the study, it is forbidden to eat solid food; you must drink only clear liquids (teas, still water, juices).
Lunch must take place no later than 15:00. You can drink any broth (clear, strained). From 17:00 on the day before a colonoscopy, you can start taking a special drug to cleanse the intestines.
Possible complications
Colonoscopy is a safe test. The risk of complications during a diagnostic examination of the colon is minimal. The risks of surgical endoscopy of the colon are less than one percent, which allows us to speak with confidence about its safety. Complications during endoscopic examination of the colon are very rare, including:
- Allergic reactions to sedative medications.
- Bleeding after biopsy, polyp removal.
- Perforation (rupture of the wall) of the intestine.
Alternative diagnostic methods
Other tests can also be used for the early diagnosis of malignant tumors of the colon:
- Fecal occult blood test (annually). The accuracy of the study is 62–79%. Out of 10 people with colon cancer, only 6-8 will test positive. False-positive results are possible if the patient has recently eaten red meat, foods rich in vitamin C, or is taking drugs from the group of non-steroidal anti-inflammatory drugs. If the test shows a positive result, endoscopy is required to clarify the diagnosis.
- Flexible sigmoidoscopy (every 5 years) is an endoscopic examination of the rectum and lower third of the colon. It is performed in the same way as a colonoscopy, but during it, a smaller part of the intestine is examined. Helps identify 70–80% of polyps and malignant tumors in the rectum and lower colon.
- Fecal DNA testing combined with stool occult blood testing (every 3 years). Can detect up to 92% of malignant tumors and up to 42% of precancerous conditions.
- Virtual colonoscopy (CT colonography) (every 5 years) - multislice computed tomography (MSCT), during which the colon is filled with air. The detection rate of tumors larger than 1 cm using this study is 94%, polyps measuring 6–9 mm is 65%. Polyps smaller than 6 mm are not detected. If a polyp is found during CT colonography, endoscopy will still have to be performed to remove it. [9,10]
An image taken during CT colonography
Thus, colonoscopy is the most accurate and informative method of screening for colon cancer, while it makes it possible to immediately carry out a biopsy and some therapeutic manipulations.
Preparation with Flit
Fleet is a drug that appeared relatively recently, its popularity is rapidly growing, many patients have been convinced of the effectiveness of the drug from their own experience.
Rules for preparation using the drug Flit
- Take in two doses.
- 45 ml of the product is diluted in half a glass of water and consumed immediately after breakfast;
- the second dose (45 ml) - in the evening after a diet dinner.
- If the patient has time, you can take another dose in the morning on the day of the examination, no later than 8-00.
- Breakfast and dinner should include only 1 glass of water.
- Lunch should be dietary and include no more than 750 ml of water.
- Each dose of Flit should be washed down with 1-3 glasses of cold water; after taking the drug, the liquid can be consumed in unlimited quantities.
- Fleet begins to act approximately 30 minutes after administration.
Colonoscopy results
Further tactics depend on whether certain pathological neoplasms have been detected.
No pathological changes were found
In such cases, no additional diagnostic procedures are required. The doctor will recommend repeating the procedure in 5–10 years. If the intestines were poorly prepared and feces remain in it, which prevented a full examination of the mucous membrane, repeat endoscopy will be recommended after a year.
If 1-2 polyps measuring less than 1 cm are found with a low risk of malignancy
The doctor will recommend repeating the test in 5 years.
If “dangerous” polyps are detected
Your doctor may recommend a repeat colonoscopy sooner than five years later in the following cases:
- more than two polyps were found in the colon;
- polyp size more than 1 cm;
- polyps were found, while there are fecal masses in the intestine, which complicate its full examination;
- according to the results of the biopsy, the removed polyps belong to histological types that have a high tendency to malignant degeneration;
- Cancer cells were found in the polyp.
If polyps are identified that could not be removed endoscopically
Such patients should consult a doctor. Perhaps the question of abdominal surgery will arise.
If cancer is detected
An examination is prescribed that helps assess the stage and other characteristics of the malignant tumor. The patient is referred to the oncology clinic, treatment begins in accordance with the protocols. If the doctor was unable to guide the colonoscope to the end of the colon
X-ray with barium enema or CT colonography may be prescribed.
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- S. V. Kashin, E. L. Nikonov, N. V. Nekhaikova, D. V. Lileev. Standards for quality colonoscopy (a manual for doctors). Russian Research Medical University named after. N.I. Pirogova. Moscow, 2022.
- Subbotin A.M. Is ideal preparation for a colonoscopy a reality or a goal on the horizon? Stages of improving its quality. Regular issues of "RMZh" No. 28 dated December 10, 2010.
- Shulpekova Yu. O. High-quality preparation for colonoscopy is the key to accurate diagnosis // MS. 2022. No. 15.
- Ivashkin V.T., Shelygin Yu.A., Khalif I.L., Belousova E.A. and others. Clinical recommendations of the Russian Gastroenterological Association and the Association of Coloproctologists of Russia for the diagnosis and treatment of ulcerative colitis. Coloproctology, 2022, No. 1 (59).
- All-Russian Union of Public Associations, Association of Oncologists of Russia. Clinical guidelines for the diagnosis and treatment of patients with colon cancer. Moscow, 2014.
- Nikiforov P.A. , Blokhin A.F. , Vakhlakov A.N. , Vinogradova N.N. , Gribunov Yu.P. , Danko A.I. , Nikitina S.A. 20 years of experience in the use of colonoscopy in the diagnosis of colon tumors. Regular issues of "RMZh" No. 28 dated December 28, 2003.
- K. A. Forde. Therapeutic colonoscopy. World J Surg. Nov-Dec 1992;16(6):1048-53. doi: 10.1007/BF02067060.
- Krushelnitsky V. S., Korochanskaya N. V., Durleshter V. M., Gabriel S. A., Guchetl A. Ya. Colonoscopy in the diagnosis and treatment of polypoid formations of the colon // EiKG. 2013. No. 6.
- V. N. Volkov, V. A. Ovchinnikov Pros and cons of virtual colonoscopy // Bulletin of the Smolensk State Medical Academy. 2012. No. 1.
- Zholdybay Zh.Zh., Amankulov Zh.M., Abdrasilova Zh.S., Karimbaeva A.M., Sadibekova A.K. Virtual colonoscopy // Bulletin of KazNMU. 2018. No. 3.
New schemes for bowel preparation for colonoscopy
The effectiveness of colonoscopy and the detection of intestinal pathology during its implementation largely depend on the quality of intestinal cleansing. Inadequate preparation of the intestine for examination may cause the endoscopist to miss any pathological focus. This, in turn, can cause untimely diagnosis of many serious diseases, including colon cancer, and, as a result, the cost of additional funds for re-preparing the patient for the study and the actual repeat colonoscopy itself. Despite the understanding of the importance of adequate bowel preparation by all stakeholders - gastroenterologists referring patients for examination, medical staff of departments, patients, in daily clinical practice endoscopists regularly encounter poor visualization during colonoscopy. Currently, on the domestic pharmaceutical market there is a fairly large number of different products, the use of which can qualitatively cleanse the intestines for carrying out a full-fledged endoscopic or any other instrumental examination or surgical intervention. Adequate bowel preparation should be properly motivated by doctors in front of patients, in order for them to comply with the diet and regimen of taking a cleanser, chosen for each patient personally.
The number of diagnostic and therapeutic endoscopic examinations of the colon has increased significantly in recent years. At the same time, the capabilities of colonoscopy itself have increased significantly. The quality of endoscopes is improving, and it has become possible to examine the mucous membrane in high-definition (HD) conditions, using narrow-spectrum lighting and magnifying (ZOOM) endoscopy [1]. Currently, colonoscopy is the leading research method in the diagnosis and differential diagnosis of inflammatory bowel diseases, identifying polyps of the large and small intestine, and diverticulosis. Colonoscopy is an indispensable diagnostic method when conducting national screening programs for the early detection of colorectal cancer. The technical capabilities of endoscopy, and even more so the combination of colonoscopy with confocal microscopy, currently make it possible to determine areas of mucosal dysplasia in developing adenomas literally at the cellular level, accurately localizing the lesion with an error of just a few microns. However, such possibilities of endoscopic examination can only be realized in the presence of a clean intestinal mucosa, freed from various organic deposits and foamy contents [2, 3]. Adequate bowel cleansing is especially important when examining the right parts of the colon, where it is technically more difficult to diagnose early forms of malignant neoplasms and (or) flat, serrated neoplasms [4–7]. In addition, insufficient quality of bowel cleansing often leads to forced interruption of an already started colonoscopy, which in turn leads to additional costs for re-preparing the patient for colonoscopy and the actual endoscopic examination itself [1–3]. Re-referring a patient for a colonoscopy, additional time spent on bowel preparation, and performing a repeat colonoscopy itself may carry an unjustified risk and, as a result, late diagnosis of the pathological process.
Despite the obvious importance of high-quality bowel preparation for colonoscopy, in daily practice, unfortunately, it does not always meet the requirements. Insufficient bowel cleansing can cause tumors to “miss.” Thus, according to P. A. Nikiforov, 28 out of 377 patients a year after colonoscopy were diagnosed with stage II or III cancer, and in 34 - stage I cancer, which indirectly indicates that this pathology was missed during the initial examination due to inadequate preparation [8]. Almost the same results are reported by Lebwohl et al. based on an analysis of the work of the endoscopy department of a large multifunctional clinic, where out of 12,787 colonoscopies, bowel preparation was insufficient in 24% of patients [9]. Of note is the fact that only 17% of patients with initial inadequate bowel preparation underwent repeat endoscopy in the next 3 years. Of the 198 adenomas identified in this study, 42% were detected only at repeat colonoscopy.
The challenge in ensuring good bowel preparation is multifactorial. Only by taking into account all the components of this process can the proper quality of the intestinal condition and effective endoscopic examination be achieved.
One of the main components of solving this problem is, strange as it may sound, the patients themselves who are about to undergo a colonoscopy. In addition, the patient factor consists of two parts - subjective, which directly depends on the patient’s behavior, and objective, independent of the behavioral and psycho-emotional state of patients. Before the study, patients do not always adhere to the recommended diet and use of bowel cleansing agents. Even if the most effective existing means of bowel cleansing is used in patients who have violated their diet to one degree or another during the period of preparation for colonoscopy, the result of bowel cleansing may be negative. It is extremely important to convey to the patient, through the mouth of the doctor, medical personnel, or with the help of visual aids and materials, information about the need for strict adherence to diet and dietary restrictions, which are (usually) not so critical for lifestyle, but are extremely important for the quality of bowel preparation. But even if patients fully understand the need to comply with dietary restrictions, their observance cannot be guaranteed in all cases. In addition, the quality of bowel preparation in patients can be influenced not only by various errors in food, but also by objective factors. The overall result of the quality of bowel preparation can be influenced by multiple, at first glance insignificant, factors, for example, a sedentary lifestyle, sedentary work, difficult access to the toilet or limited fluid intake; even multi-bed rooms in clinics and hospitals can affect the psychological state patients and influence the quality of bowel preparation.
Another important component when cleansing the intestines is the correct choice of a drug that directly affects the contents of the intestine and evacuates it from the body. Each drug used in a given situation must meet certain requirements on the part of both research doctors and patients using it.
For endoscopists, it is important that the drug for bowel cleansing, when used, provides a clean mucous membrane without any residue of solid or liquid contents in the intestinal lumen, is well tolerated by patients and does not require additional monitoring of the health status of the subject.
On the other hand, the ideal drug for colon cleansing should not only meet the requirements of doctors, but also fully comply with the wishes of the patients taking this drug. It should have pleasant organoleptic properties with no adverse drug reactions (pain, nausea, vomiting) when taking it. In this case, preference is given to drugs that require less liquid to take, with minimal dietary restrictions and to a lesser extent change the normal rhythm and quality of life.
Currently, there are several groups of drugs on the pharmaceutical market intended for oral administration to prepare the intestines for instrumental studies. Each of these groups differs in the mechanism of action and, therefore, the effectiveness of the preparation. Unfortunately, none of the existing drugs is ideal in all respects, as evidenced by numerous clinical studies [9, 10]. Between different groups of drugs, even those that are similar in composition, there are noticeable differences in the quality of bowel preparation in terms of tolerability by patients [12].
The UK National Patient Safety Agency (NPSA) has issued guidelines for the safe use of oral bowel cleanses [13]. These guidelines make clear the possible clinical risks of using various oral colon cleanses. The recommendations, in particular, note that the decision to use a particular product should be made as responsibly as the decision to conduct an instrumental study itself, and all patients should fill out a written informed consent form to prevent possible risks when using oral cleansers . This guideline, as well as other recent meta-analyses, now focuses specifically on the safety of oral cleanses, provides guidelines for bowel preparation, absolute and relative contraindications for the use of various oral cleanses, and provides recommendations for the selection and use of these drugs in patients with various risk groups [14–17].
With any oral drug, no matter how effective, all bowel preparation efforts can be nullified if the patient does not follow a specific diet before starting preparation. For high-quality preparation, it is necessary to prescribe patients a slag-free diet for 2-3 days before starting bowel cleansing, so that there is as little dense undigested food residues in the intestinal lumen as possible. This provides the basis for subsequent effective lavage. In particular, foods that should be excluded from patients' diets include: vegetables (carrots, beets, cabbage, turnips, radishes, onions, garlic); herbs (sorrel or spinach); porridge, but not all (oatmeal, millet, pearl barley); legumes (peas, beans, lentils, beans); fruits (peach, apple, pear, bananas, tangerines, grapes, dried fruits); nuts of all varieties; any berries; rye bread, any products made from rye flour; dairy products (except fermented milk); fried, smoked meat, smoked sausages. These dietary restrictions are not critical for most patients, since dietary restrictions are recommended only for a short period of time, and besides, there remains a fairly large range of food products allowed for use: broths, eggs, semolina porridge, boiled meat and boiled sausage , cheese, butter, fermented milk products (but not cottage cheese), fish. On the day of the examination, you can only consume liquid food: tea, broth, mineral or boiled water, clear juices. In addition to the dietary restrictions that each patient must adhere to, depending on the type of cleansing drug used, there are absolute and relative contraindications for performing oral bowel preparation for colonoscopy. Thus, absolute contraindications include: suspicion of intestinal obstruction or perforation, obstruction of the gastrointestinal tract at any level, severe acute inflammatory bowel disease or toxic megacolon, impaired consciousness, hypersensitivity or allergic reaction to the components of the drug, difficulty swallowing and the inability to swallow without aspiration (in some cases, bowel cleansing can be done through a nasogastric (nasoduodenal) tube or other tube placed at the level of the duodenum). In this case, the preparation should be carried out in a hospital setting under the supervision of a doctor.
Relative contraindications for oral administration of bowel cleansing drugs are in patients undergoing hemodialysis or peritoneal dialysis, after a kidney transplant, suffering from chronic heart failure, cirrhosis of the liver and (or) having ascites. In these cases, you need to be very careful when choosing a cleanser and give preference to products based on polyethylene glycols.
Thus, drugs containing sodium sulfate and sodium phosphates, magnesium salts should be used with caution in patients with renal failure, liver cirrhosis, chronic heart failure, as there is a risk of developing water and electrolyte disorders.
Research to optimize bowel preparation processes continues to this day [18–21]. In healthy individuals, sodium phosphate-based preparations are currently recommended for use only in cases of individual intolerance to polyethylene glycol (PEG). In other cases, the drugs of choice currently remain those based on polyethylene glycols. But even in this case, there is quite a lot of freedom of choice among representatives of this series. Macrogol cleansers are currently available with molecular weights of 4000 and 3350. The differences in the molecular weight of the product component may seem minor, but these differences can have a significant impact on the quality of bowel preparation and the quality of life of patients.
For a long time, most experts gave preference to drugs based on macrogol 4000. Compared to drugs based on magnesium or sodium salts, these drugs are safe in relation to the state of the body’s water and electrolyte balance. They do not come into contact with the mucous membrane. Once in the lumen of the colon, macrogols form a gel-like substance that accumulates fluid located in the lumen of the intestine. In this case, the mechanoreceptors of the intestinal wall are irritated, peristalsis is activated and active cleansing of the intestine occurs. A significant disadvantage of Macrogol 4000 is the need for strong dilution of the drug and the intake of a significant volume of liquid when preparing for colonoscopy. On average, the volume of the cleansing agent is calculated from the ratio: 1 liter of macrogol 4000 solution per 20 kg of patient’s body weight. So, with an average weight of 70–75 kg, it is necessary to drink 4 liters of solution for adequate bowel preparation. In addition, the composition of the so-called first generation drugs, along with PEG, also includes some salts - in particular, potassium chloride, sodium chloride and sodium bicarbonate, designed to compensate for possible electrolyte losses. The presence of sodium sulfate in the composition of the drug (in various modifications up to 5.0 or 5.7 g) gives the solution a bitter-salty taste, which significantly reduces the organoleptic properties of the solution and can cause mild nausea and discomfort in some patients, especially when taking a large volume liquids.
At the Moscow Scientific Research Center we carried out research work on the use of a PEG solution with a lower molecular weight - macrogol 3350 (Endofalk). The drug is supplied in powder for preparing a solution. The isoosmotic solution of the drug consists of macrogol 3350, a mixture of electrolytes potassium and sodium chloride and sodium bicarbonate, which prevent the absorption of fluid in the lumen of the gastrointestinal tract. Silicon dioxide, also included in the mixture, has an antifoaming effect and prevents the development of flatulence. The use of PEG with a lower molecular weight made it possible to reduce the amount of stabilizing electrolytes, which improved the organoleptic properties of the drug. We observed 68 patients who underwent bowel preparation before colonoscopy. All patients were divided by blind randomization into two groups, the first included 29 people, the second 39 people. Both groups did not differ from each other in terms of gender and age. In order to determine the effectiveness of using PEG with a molecular weight of 3350, the first group of patients received a 3-liter Endofalk solution as preparation for colonoscopy, the second control group of patients received a 4-liter PEG solution with a molecular weight of 4000. Two days before the study, all patients followed a slag-free diet. The drug was taken before the study in two stages. Patients took the first portion of the drug in the evening before the study (starting at 18:00), the second portion - in the morning on the day of the study, 4 hours before the colonoscopy.
When taking the drug, the organoleptic properties and subjective sensations of patients were assessed in the form of a survey. The quality of bowel cleansing was assessed during colonoscopy using the international classification of bowel cleansing quality. Moreover, the study for endoscopists was blind, since they did not know which patient was prepared with which drug, and assessed the quality of bowel preparation only on the basis of objective criteria according to the Chicago Bowel Preparation Scale [22]. According to this classification, the large intestine is divided into three sections - left, middle and right. Each of the segments is assessed using a twelve-point system, to which is added a four-point gradation for assessing the amount of fluid in the intestinal lumen that is already present before the start of the study (Tables 1, 2).
Research results
Based on the results of colonoscopy performed by endoscopists, we did not note a significant significant difference in the quality of bowel preparation using Endofalk or macrogol 4000 solution.
Thus, in 87.4% of patients receiving Endofalk and 85.8% receiving Macrogol 4000, the degree of intestinal cleansing was 36 points; in 9.4% of patients in the first group and 7.6% in the second, the score corresponded to 32–34 points; in 3.2% of the first group of patients and 5.6% of the second group, the degree of intestinal cleansing was assessed within 28–31 points. In both groups, the amount of residual fluid was assessed as 0–1 point.
We noted the difference when taking different bowel preparation regimens during a survey of patients who assessed the taste of the solutions, the quality of night sleep, the number of bowel movements, the appearance of nausea, weakness, vomiting, thirst, dizziness, as well as during an objective and laboratory examination of patients in both groups for changes blood pressure, changes in basic indicators of acid-base balance.
As can be seen from table. 3, patients liked the taste of Endofalk more, which, according to some patients, has a pleasant taste of orange and passion fruit, compared to the bitter-salty taste of macrogol 4000, which is given to it by sodium sulfate in the solution (p < 0.05). The number of bowel movements during preparation with both drugs, as well as the quality of night sleep in both groups, was approximately the same, and we did not note a significant difference.
When assessing subjective feelings, the majority of patients in the first group liked Endofalk and rated it as “good” (96.5%), while less than half of the patients in the second group (43.6%) liked Macrogol 4000 (p < 0. 05). 41% of patients in the same group rated Macrogol 4000 “satisfactory” and 15.4% did not like it at all. Nausea while taking drugs was experienced by 14 people from the second group and 2 from the first; weakness while taking the drugs developed only in one patient when taking Endofalk and in 12 people taking Macrogol 4000. Also, only patients in this group experienced vomiting (1 patient). Thirst after taking the drugs was experienced by 4 patients of the second group and 1 patient while taking Endofalk.
When analyzing data from instrumental and laboratory studies, we noted only a slight increase in blood pressure values in 5 patients taking macrogol 4000, which did not affect the general condition of the patients. There were no changes in the acid-base status in any of the patients under our supervision.
The results of the study showed almost the same efficiency of intestinal cleansing when using traditional drugs based on macrogol 4000 and a new drug for Russia based on macrogol 3350 (Endofalk). However, Endofalk showed better organoleptic properties, and the smaller volume of liquid required when taking this drug allowed us to achieve better subjective sensations for patients compared to taking solutions of macrogol 4000. The results of our studies coincided with similar studies conducted in other countries [23, 24 ].
In addition to a comparative study of traditional bowel preparation, a small pilot study was conducted in a limited group of patients (12 people) on bowel preparation using low volumes of Endofalka (2 liters) in combination with bisacodyl, an irritant laxative that increases intestinal motility and increased mucus production. Three days before the study, patients were prescribed a slag-free diet. On the eve of the colonoscopy, solid food was excluded from the morning until 2 p.m. It was allowed to take only clear liquids (broth, tea, juice without pulp, mineral water), at 14:00 bisacodyl was prescribed - 4 tablets of 5 mg each, and at 18:00 patients were asked to drink 1 liter of Endofalk solution. In the morning, on the day of the study, 3 hours before the colonoscopy, the patients drank another liter of Endofalk solution. At the same time, if desired, when taking Endofalk, it was allowed to additionally take a clear liquid. The results of this training scheme in our study coincided with the work of German colleagues [25]. Good quality of preparation was achieved in more than 90% of patients, which was comparable to the results of preparation according to the traditional regimen using Macrogol 4000 or Endofalk in full. However, when Endofalk was combined with bisacodyl, all patients gave positive subjective assessments.
Conclusion
Preparing the bowel for a colonoscopy is a complex process. During preparation, patients must adhere to a restrictive diet and take special laxatives and additional fluids, which lead to profuse diarrhea. Thus, the intestines are cleared of contents. Often, preparing the intestine for instrumental studies may be accompanied by nausea and bloating. In some cases, the laxative may have an unpleasant taste. Bowel preparation processes, as a rule, disrupt the usual rhythm of life of patients. All these negative factors can influence patients' refusal to undergo colonoscopy.
However, given the recent increase in intestinal diseases, endoscopists and gastroenterologists need to motivate patients to undergo this study and, accordingly, the need for bowel preparation. Motivation should be built on three main pillars: firstly, it is necessary to explain the importance of performing a colonoscopy itself and identifying intestinal pathology at an early stage, secondly, it is necessary to explain to the patient the mechanism of intestinal cleansing when using various schemes, explain the importance of following a diet and rules of administration drugs, and thirdly, an individual approach to each patient is necessary for the optimal choice of drug for him.
Although none of the drugs available in clinical practice show significant superiority in cleansing efficiency, there are significant differences in their tolerability among patients, which, ultimately, should be at the forefront when choosing a particular method of bowel preparation.
When considering the issues of pharmacoeconomics and the cost of various bowel preparation regimens, it should be borne in mind that if the preparation is inadequate, it is necessary to repeat the study and then the cost of a colonoscopy can at least double.
Thus, in the arsenal of modern gastroenterologists and endoscopists there are currently many highly effective oral agents that allow achieving high quality bowel preparation while maintaining a favorable attitude towards the preparation and conduct of colonoscopy itself in patients. In this case, the most important rule must be observed - strictly follow the rules and preparation schemes when using any drug in order to get the best result, otherwise even the best existing drug can be discredited in the eyes of the patient.
Literature
- Hendry PO, Jenkins JT, Diament RH The impact of poor bowel preparation on colonoscopy: a prospective single center study of 10571 colonoscopies. Colorectal Dis. 2007; 9:745–748.
- Froehlich F., Wietlisbach V., Gonvers JJ et al. Impact of colonic cleansing on quality and diagnostic yield of colonoscopy: the European Panel of Appropriateness of Gastrointestinal Endoscopy European multicenter study // Gastrointest Endosc. 2005; 61:378–384.
- Spiegel BMR, Talley J, Shekelle P et al. Development and validation of a novel patient educational booklet to enhance colonoscopy preparation // Am J Gastroenterol. 2011; 106:875–883.
- Hetzel JT, Huang CS, Coukos JA et al. Variation in the detection of serrated polyps in an average risk colorectal cancer screening cohort // Am J Gastroenterol. 2010; 105:2656–2664.
- Kahi CJ, Hewett DG, Norton DL et al. Prevalence and variable detection of proximal colon serrated polyps during screening colonoscopy // Clin Gastroenterol Hepatol. 2011; 9:42–46.
- Brenner H., Chang-Claude J., Seiler CM et al. Interval cancers after negative colonoscopy: population-based case-control study // Gut. 2012; 61:1576–1582.
- Singh H, Nugent A, Demers AA et al. The reduction in colorectal cancer mortality after colonoscopy varies by site of the cancer // Gastroenterology. 2010; 139:1128–1137.
- Nikiforov P. A., Golubeva S. V., Bazarova M. A., Grankov S. S. Use of the drug fortrans in preparation for colofibroscopy and endoscopic polypectomy // Ross. magazine gastroenterol., hepatol., coloproctol. 1999. No. 5. pp. 1–4.
- Lebwohl B., Kastrinos F., Glick M. et al. The impact of suboptimal preparation on adenoma miss rates and the factors associated with early repeat colonoscopy // Gastrointest Endosc. 2011; 73:1207–1214.
- Connor A., Tolan D., Hughes S. et al. Consensus guideline for the prescription and administration of oral bowel cleansing agents. 2009. https://www.rcr.ac.uk (accessed 28 Jun 2012).
- Connor A., Tolan D., Hughes S. et al. Consensus guidelines for the safe prescription and administration of oral bowel cleansing agents // Gut. 2012; 61:1525–1532.
- British National Formulary. London: BMJ Publishing Group Ltd, RCPCH Publications Ltd and the Royal Pharmaceutical Society of Great Britain, No. 63, March 2012.
- National Patient Safety Agency. Rapid Response Alert. Reducing risk of harm from oral bowel cleansing solutions. https://www.npsa.nhs.uk/nrls/alerts-and-directives/rapidrr/reducing-risk-of-harm-from-oral-bowelcleansing-solutions (accessed 25 Jun 2012).
- Turner D., Benchimol E.I., Dunn H. et al. Pico-Salax versus polyethylene glycol for bowel cleanout before colonoscopy in children: a randomized controlled trial // Endoscopy. 2009; 41: 1038–1045.
- Siddiqui AA, Yang K, Spechler SJ et al. Duration of the interval between the completion of bowel preparation and the start of colonoscopy predicts bowel-preparation quality // Gastrointest Endoscopy. 2009; 69: 700–706.
- Cohen LB Split dosing of bowel preparations for colonoscopy: an analysis of its efficacy, safety and tolerability // Gastrointest Endosc. 2010; 72:406–412.
- Unger RZ, Amstutz SP, Seo DH et al. Willingness to undergo split-dose bowel preparation for colonoscopy and compliance with split-dose instructions // Dig Dis Sci. 2010; 55:2030–2034.
- Seo EH, Kim TO, Park MJ et al. Optimal preparation-to-colonoscopy interval in split-dose PEG bowel preparation determines satisfactory bowel preparation quality: an observational prospective study // Gastrointest Endoscopy. 2012; 75:583–590.
- Van Dongen M. Enhancing bowel preparation for colonoscopy: an integrative review // Gastroenterol Nursing. 2012; 35: 36–44.
- Lebwohl B., Wang T.C., Neugut AI Socioeconomic and other predictors of colonoscopy preparation quality // Dig Dis Sci. 2010; 55: 2014–2020.
- Rosenfeld G., Krygier D., Enns RA et al. The impact of patient education on the quality of inpatient bowel preparation for colonoscopy // Can J Gastroenterology. 2010; 24:543–546.
- Gerard DP Validation of a New Bowel Preparation Scale for Measuring Colon Cleansing for Colonoscopy // The Chicago Bowel Preparation Scale Clinical and Translational Gastroenterology. 2013, 4, 1–11.
- Wexner SDL, Beck DE, Baron TH et al. A consensus document on bowel preparation before colonoscopy: prepared by a task force from the American Society of Colon and Rectal Surgeons (ASCRS), the American Society for Gastrointestinal Endoscopy (ASGE), and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) / / Gastrointest Endosc. July 2006; 64(1):154.
- Zakharash Y., Khohklova V., Radchenko L., Greinwald R., Pröls M., Zakharash M. Single-blind, randomized, monocentric, comparative study of the efficacy and tolerability of two different dosages of polyethylene glycol vs. polyethylene glycol + electrolytes in bowel preparation for colonoscopy // Endoscopy. 38 (Suppl II): A231.
- Preis J. et al. Open observational study to assess efficacy and sajavascript: void (0)fety of combined use of Endofalk and bisacodyl tablets for colon cleansing prior to colonoscopy. Falk Symposium 161.
P. L. Shcherbakov1, Doctor of Medical Sciences, Professor A. I. Parfenov, Doctor of Medical Sciences, Professor E. V. Albulova, Candidate of Medical Sciences
GBUZ MKNPTs DZM, Moscow
1 Contact information