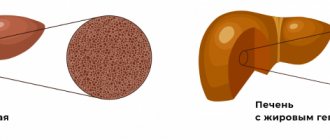
“Faty liver” is a disease that is characterized by excessive accumulation of fat in the liver cells.1 This disease has several names - fatty liver, steatosis, fatty degeneration, but each of them means only one thing - it is not to be trifled with, and its early diagnosis, as well as subsequent treatment, must be timely and comprehensive.
To begin with, it is worth remembering that fatty liver disease can be associated with alcoholic or non-alcoholic liver damage.2 Next we will talk about non-alcoholic damage. Recently, the number of patients with non-alcoholic fatty liver disease (NAFLD) has increased significantly. Thus, according to statistics, in 2007 NAFLD was detected in 27% of patients, while in 2014 this figure increased to 37%. Thus, NAFLD currently ranks first in frequency among chronic liver diseases.1
Causes of fatty hepatosis
There are three main reasons for the development of hepatic steatosis:
- Obesity. If the body mass index exceeds 30, the likelihood of dystrophy is about 40%.
- Drinking alcoholic beverages. Moreover, hepatosis can occur even in people who drink a little, but every day. There is a direct relationship between the duration of alcohol consumption and the severity of liver dystrophy and, as a consequence, the risk of developing cirrhosis.
- Long-term use of medications with hepatotoxic effects.
Less commonly, hepatosis develops against the background of diseases that occur with metabolic disorders; this category includes hyperlipidemia, hypercholesterolemia, diabetes mellitus, thyrotoxicosis, myxedema, Itsenko-Cushing syndrome, malignant neoplasms, chronic diseases of the gastrointestinal tract, in which the absorption process is disrupted, etc. .
Liver dystrophy can be caused not only by obesity, but also by poor nutrition - overeating, abuse of fatty foods and foods containing hydrogenated fats and simple carbohydrates.
The disease is sometimes diagnosed in people who have a deficiency of enzymes involved in lipid metabolism (hereditary disease).
Most often, more than one factor leads to the development of steatosis. In most cases, there is a multifactorial factor, for example, the consumption of alcohol by a person who is eating poorly or taking toxic medications.
Medications for detoxification
Medications with a detoxification effect effectively cleanse liver cells of toxic compounds, strengthening their structure and improving functioning. Most often, the following drugs are prescribed for fatty hepatosis:
- Polysorb
is an effective enterosorbent that fights toxic decay products, allergens, and toxic substances; - Antral
- used for the treatment and prevention of inflammatory liver lesions; - Kholosas
is a shiro made from rose hips, containing an increased concentration of ascorbic acid and cleansing hepatocytes of toxins.
Also common enterosorbents include Enterosgel - acts against metabolic products and toxic substances, Ovesol - cleanses the liver and fights bile stagnation, improving its outflow.
In the treatment of fatty liver, other enterosorbent drugs can be used - Atoxil, Polyphepan, sodium thiosulfate, activated carbon.
In order to accelerate the elimination of toxic substances and prevent the development of dysbiosis, detoxification solutions are prescribed for cleansing enemas. The most commonly used are Normaze or Duphalac.
Classification
Based on etiology, hepatosis is divided into non-alcoholic fatty liver disease and alcoholic steatosis. The first type of disease is diagnosed in only 7–10% of cases.
Hepatosis occurs:
- primary - caused by metabolic disorders, for example, obesity or hyperlipidemia;
- secondary – due to the impact on the body of external negative factors, which subsequently lead to metabolic disorders, for example, fasting, long-term use of corticosteroids, intestinal resection.
Doctors also take into account the characteristics of fat deposition, according to which hepatosis is divided into:
- diffuse;
- zonal;
- focal disseminated;
- pronounced disseminated.
Symptoms of fatty liver disease
There are no specific signs of fatty liver hepatosis, even when there are already significant morphological changes. This is the insidiousness of the disease and lies a serious danger.
At the initial stage, the following nonspecific symptoms of fatty hepatosis may occur:
- general fatigue, asthenia, decreased ability to work;
- heaviness in the abdomen, stool instability, discomfort in the right hypochondrium, nausea, flatulence, sometimes vomiting;
- weight gain;
- causeless increase in body temperature for a long period of time;
- slight enlargement of the liver;
- skin itching.
As the disease progresses, icteric staining of the mucous membranes and skin is possible. Blood pressure often decreases and fainting occurs. There is a tendency to hemorrhages (increased bleeding).
There are 3 degrees of fatty hepatosis depending on the lesion:
- up to 33% – I degree;
- 33–66% – II degree;
- more than 66% – III degree.
Dietary recommendations
There is no diet that suits everyone without exception. Patients with fatty hepatosis first of all need to reduce the calorie content of their daily diet. One of the recommendations may be advice on limiting the consumption of foods rich in saturated fatty acids and replacing them with foods containing monounsaturated or polyunsaturated fats (milk, olive oil, fish oil).
Nutritional balance
The main parts of food are proteins, fats, carbohydrates, water, minerals and vitamins, which must be strictly balanced. The ratio between proteins, fats and carbohydrates should be 1:1:4.
Animal proteins should make up about 60% of the total protein. Of the total fat, 20-25% should be vegetable oils as a source of polyunsaturated fatty acids.
The balance of carbohydrates is expressed in the ratio of starch, sugar, fiber and pectin. Sugars should be represented by fruits, berries, dairy products, and honey. It is extremely important to maintain a balance of vitamins and minerals, which must be supplied to the body daily in accordance with daily requirements.
Diet
This is the number of meals and the interval between them during the day. For healthy people 3-4 times a day at 4-5 hour intervals. For some concomitant diseases, such as obesity, it is necessary to eat 5-6 times a day.
Nutrition for liver diseases
The diet for fatty hepatosis should be gentle and create maximum liver rest. It is necessary to reduce the amount of fat and enrich the diet with foods that are sources of complete proteins and vitamins, reduce the sugar content and increase the amount of fluid. Meals should be frequent and in small portions. It is necessary to exclude fatty meats, smoked meats, spices, spicy, rich dough. Alcohol is absolutely prohibited.
To find a diet that is right for you, consult your doctor.
up
Diagnostics
Diagnosis of the disease is difficult. Firstly, steatosis has no specific symptoms. Secondly, biochemical tests do not show significant changes. Sometimes the activity of serum transaminases increases, but this indicator does not change in all patients with steatosis. In this regard, differential diagnosis with hepatitis, biliary tract obstruction, primary hemochromatosis, and hepatocerebral dystrophy is of primary importance.
The doctor makes the final diagnosis based on a comprehensive examination and a series of tests, including ultrasound and biopsy.
To find out the cause of fatty hepatosis, the level of insulin in the blood, serum glucose concentration, hormonal status, antibodies to cytomegalovirus and hepatitis viruses, markers of autoimmune hepatitis, etc. are determined.
Results of treatment of liver steatosis
Patient review:
» Dear Bella Leonidovna!
Dear Nelly Nikolaevna Tsurikova, Mushinskaya Kira Vladimirovna, girls at the reception, ultrasound diagnostic doctor, thank you all so much for organizing the treatment of my illness. You guys work wonders as a team! High-level professionals and people with a capital “P!” I am grateful to fate that I found your clinic, which really saved my life and changed it 180 degrees. Thanks to your efforts, qualifications and attention, I have become a completely healthy person. I lost 23.5 kg in 9 months, my liver has become a real factory that now works perfectly!
In general, I wish your team all the best. Do not stop! You really do a great job for people, help overcome serious illnesses.
On the eve of the New Year 2022, I would like to wish you health, family joys and love too! with best wishes, your patient from Kazan" >>> - Rustem 12/05/2018
Treatment of fatty hepatosis
Treatment of fatty hepatosis is usually complex, including diet therapy, drug therapy and physical therapy.
Diet plays an important and sometimes paramount role in the treatment of steatosis. Sometimes, to cure the first stage, it is enough to follow a diet. Thanks to a significant limitation of fat consumption, healthy cells, and there are more than 66% of them, independently remove the fat present in the liver. But even in the later stages, nutritional correction is a prerequisite. It is recommended to steam food, eat more greens, vegetables and low-fat dairy products, eggs, cereals, and vegetarian dishes.
The cause of its occurrence directly affects how fatty hepatosis is treated.
Weight loss is a necessary condition for obese patients. As a rule, this helps to get rid of insulin resistance, which leads to normalization of carbohydrate and lipid metabolism. But there is one important nuance here - you should not lose weight too quickly (up to 600 g per week is allowed), otherwise there is a risk of progression of fatty hepatosis.
For alcoholic fatty degeneration, successful treatment is only possible with complete abstinence from alcohol. Patients are recommended to consult a narcologist.
Lipotropic drugs for fatty hepatosis are prescribed to accelerate the removal of fat from the liver. This category includes drugs that normalize cholesterol and lipid metabolism, promote fat oxidation and its mobilization from the liver: lipoic acid, essential phospholipids, folic acid, B vitamins.
To prevent the destruction of cell membranes and stimulate the regeneration of hepatocytes, hepatoprotective drugs are prescribed for fatty liver hepatosis: betaine, taurine, ursodeoxycholic acid, glutargin, phosphatidylcholine,
Tablets containing ursodeoxycholic acid often prescribed for fatty hepatosis: Livodexa, Grinterol, Urdoxa, Ursodez, Ursoliv, Ursofalk, Exchol, Ekurochol.
Thiazolidinediones and biguanides are used to eliminate insulin resistance.
The utilization of fatty acids is improved by physical exercise, so it is recommended for all patients with this disease.
Why is NAFLD dangerous?
Fatty hepatosis, especially at the very beginning, can be practically asymptomatic, and the existing symptoms are not specific and, thus, make diagnosis difficult. However, you should not relax - diagnosing fatty hepatosis is important for any suspicion of the presence of this disease. Because this disease, developing gradually, practically without manifesting itself clearly, nevertheless increases the risk of cardiovascular death several times - in other words, it increases the risk of developing strokes and heart attacks.4 In addition, advanced fatty hepatosis can ultimately lead to ultimately, to the development of cirrhosis and liver failure. The likelihood of this event is low, however, if it occurs, the consequences can be fatal. The fact is that cirrhosis usually requires organ transplantation, which can be further complicated in the presence of cardio-metabolic disorders and diseases that often accompany fatty hepatosis.3
Stages of development of NAFLD
- 1
Stage of fatty hepatosis (steatosis)
The initial stage of the disease, often asymptomatic
- 2
Non-alcoholic steatohepatitis
Hepatosis with accompanying inflammation of liver cells
- 3
Fibrosis with further transition to cirrhosis
At this stage, liver tissue begins to be replaced by connective tissue, which leads to disruption of the structure and, ultimately, disruption of the organ.3
Fatty hepatosis of pregnant women
Separately, there is hepatic steatosis, which occurs without a significant cause in women bearing a child. Acute fatty hepatosis of pregnancy is diagnosed in one out of 13,000 women. 20–25% of cases end in death, according to foreign authors, and up to 60%, according to domestic sources.
The disease progresses quickly, over 2–3 weeks. Occurs mainly in late pregnancy - 32–36 weeks. The exact cause of this pathology has not yet been established.
Symptoms that may indicate acute fatty hepatosis in pregnant women: excessive vomiting, severe nervous disorders, general weakness, drowsiness.
The only treatment method is emergency delivery. Within 5 weeks after birth, the disease regresses.
Anti-obesity drugs
Weight loss is considered an important part of the treatment of fatty hepatosis in men and women. For this purpose, drugs are used that stimulate metabolism, accelerate lipid metabolism, and reduce hunger. Anti-obesity drugs inhibit the absorption of calories and their conversion into fat cells. To normalize weight, use:
- Meridia
- provides a long-lasting feeling of fullness even after small portions of food and can be used for type 2 diabetes; - Metformin
- used for obesity against the background of type 2 diabetes mellitus (contraindicated for insulin dependence); - Acomplia
— affects directly the points of the brain “responsible” for hunger and reduces the need for food; - Orlistat
- inhibits the enzyme lipase, inhibiting the absorption of fats; - Sibutramine
- reduces the feeling of hunger and delays the absorption of calories.
Weight loss medications are not always prescribed - only if dieting and exercise have not brought noticeable results. It is better not to take such medications on your own, as they can cause negative side reactions.
Anti-obesity drugs should not be taken without consulting a doctor, as they have many contraindications - glaucoma, arterial hypertension, prostate disease, neurological disorders and disorders of the thyroid gland.
Prevention
Preventive measures include:
- proper nutrition, in particular limiting fatty, spicy, fried and smoked foods;
- moderation in the consumption of alcoholic beverages;
- taking medications correctly;
- regular physical activity.
Fat accumulation is often caused by excess weight due to a sedentary lifestyle. Scientists have proven that if you eat only fast food for 4 weeks, this disease will almost certainly occur. Student volunteers took part in the experiment. Moreover, the first signs appeared after 1 week of such nutrition. Therefore, nutrition and weight control are of great importance.
For prevention, hepatoprotectors should be used, especially during periods of increased load on the liver, for example, with prolonged alcohol consumption, antibiotic treatment, and following a diet aimed at weight loss.
Alcoholic hepatitis and liver cirrhosis
Alcoholic hepatitis, according to the International Classification of Diseases of the Liver Organ, is divided into acute and chronic. The disease is one of the main variants, along with alcoholic fibrosis, which transforms into cirrhosis
.
Acute alcoholic hepatitis - episodes of acute toxic necrosis (acute liver failure of alcoholics) are extremely difficult and often pose a threat to the patient’s life. This form of hepatitis develops in 30% of patients who abuse alcohol for at least 3-5 years, and malnutrition, parental alcoholism, decreased activity of acetal and alcohol dehydrogenase, and decreased HLA B40 antigen play a role.
The relationship between the lack of histocompatibility antigen HLA B40 and the development of chronic active hepatitis with subsequent transition to cirrhosis
.
This form of hepatitis (acute necrosis) can develop against the background of fatty liver
, acute hepatitis, fibrosis or cirrhosis.
In cirrhosis,
the development of acute hepatitis (necrosis) very often leads to decay (parenchymal) and shunt (portocaval) hepatic encephalopathy, which most often ends in death.
Histologically, perivenular damage to hepatocytes, balloon degeneration, their necrosis, alcoholic hyaline (Mallory bodies), leukocyte infiltration, pericellular fibrosis, etc. are observed. Necrosis of hepatocytes in the center of the hepatic hexagonal lobules.
Acute hepatitis often develops in young and middle-aged people after binge drinking with previous long-term alcohol consumption. An acute onset of pain and dyspeptic syndromes is typical, but in some patients the disease can develop gradually.
The most common icteric variant: severe weakness, lack of appetite, nausea, vomiting, jaundice, diarrhea, and sudden loss of body weight. The pain is localized in the right hypochondrium, epigastric region. There may be a fever.
Examination reveals jaundice, hepatomegaly, and fever. The area where the organ is located is painful on palpation and smooth. In some patients, the spleen enlarges, palmar roofing material (erythema), skin spider veins, hand tremors (asterixis), which is a sign of hepatic encephalopathy, mental disorders (lethargy, agitation, hallucinations), ascites resistant to diuretics. Concomitant infections are noted: pneumonia, pyelonephritis, active tuberculosis. The cholestatic variant with skin itching, light-colored feces, and dark urine are rare. The blood is characterized by severe hyperbilirubinemia, hypercholesterolemia, increased activity of alkaline phosphatase, gammaglutamyl transpeptidase, and a slight increase in AST and ALT.
There are fulminant (fulminant) acute alcoholic hepatitis, which is severe, often with an unfavorable prognosis, and a latent variant with an asymptomatic course. Leukocytosis with a shift to the left and a sharp increase in ESR are always observed.
Prognostically unfavorable symptoms are hepatic encephalopathy, hepatorenal syndrome, prolongation of prothrombin time by more than 50%, relapses of acute hepatitis at the stage of established cirrhosis. The prognosis is most favorable for the latent form of acute hepatitis.
Recovery is possible with complete abstinence from alcohol, but this does not always guarantee the absence of subsequent cirrhosis
.
Chronic hepatitis is divided into persistent and active mild, moderate, severe, most often representing stages of progression of acute hepatitis.
Chronic persistent hepatitis is histomorphologically manifested by pericellular and subsinusoidal fibrosis, Mallory bodies, balloon degeneration of hepatocytes. A similar picture without progression of fibrosis can persist for 5-10 years, even with moderate alcohol consumption.
Chronic persistent hepatitis is accompanied by moderate abdominal pain, bloating, anorexia, unstable stools, belching, and heartburn. The liver organ is slightly enlarged and compacted. Diffuse compaction, increase confirmed by ultrasound data. The activity of gammaglutamyl transpeptidase, serum transaminases, and sometimes the thymol test increases moderately.
Chronic active hepatitis has the above-described histomorphological picture of alcoholic hepatitis with the presence of more or less pronounced active fibrosis, sclerosing hyaline necrosis. Abstinence from alcohol for 3-6 months. leads to an improvement in the morphological picture of the type of chronic non-alcoholic hepatitis. Chronic active hepatitis in the presence of autoimmune destruction of the parenchyma is characterized by progression of the process with the transition to cirrhosis
.
Clinical manifestations are more striking than with persistent hepatitis. Jaundice and splenomegaly are more often observed (when transitioning to cirrhosis, the organ can sharply shrink). Bilirubin, gammaglutamyl transpeptidase, immunoglobulin A, moderate thymol test, and blood transaminase activity increase significantly.
There are no direct morphological markers of the alcoholic etiology of diseases of the liver organ, but there are changes that are quite characteristic of the effects of ethanol. This is alcoholic hyaline (Mallory bodies), characteristic ultrastructural changes in hepatocytes, stellate reticuloepitheliocytes. Hyalin is a protein substance synthesized by hepatocytes. In light-optical examination, it has the appearance of eosinophilic masses of various shapes (ribbon-like, reticular, globular, irregular), which are usually localized near the nucleus of the cytoplasm of hepatocytes. After the death of the hepatocyte, it can be located extracellularly. With Mallory's tricolor stain, hyaline accumulations are colored pink.
In electron microscopic examination of biopsies taken from patients with chronic alcoholism, alcoholic hyaline is detected as fibrillar or granular material. Hyaline fibrils are shorter and thicker than normal tonofilaments. The formation of Mallory bodies in hepatocytes has been described in a number of diseases of non-alcoholic etiology: diabetes mellitus, Indian childhood cirrhosis, Wilson-Konovalov disease, primary biliary cirrhosis, liver cancer, after intestinal anastomosis for obesity.
Characteristic ultrastructural changes in hepatocytes and stellate reticuloendotheliocytes reflect the toxic effects of ethanol on the body.
Changes in hepatocytes are represented by hyperplasia, vacuolization of elements of the smooth cytoplasmic reticulum, and the formation of giant mitochondria with an irregular shape. Changes in stellate reticuloepitheliocytes indicate the failure of their phagocytic function: their cytolemma does not form outgrowths, single lysosomes with electron-light content.
Constantly occurring morphological markers of the effects of ethanol on the liver are:
- fatty degeneration of hepatocytes;
- foci of liquefaction necrosis affecting the central parts of the lobules;
- inflammatory infiltrate containing, along with lymphocytes and macrophages, a large number of neutrophilic leukocytes;
- restructuring of the liver organ with the formation of false lobules of a predominantly monolobular type separated by narrow fibrous septa.
An important diagnostic value for chronic hepatitis (alcoholic, like any other etiology) is an ultrasound of the abdominal organs (liver, spleen and other organs), as well as to identify ascites and the size of the portal vein. Doppler ultrasound should be performed to exclude or establish the severity of portal hypertension. Traditionally, radionuclide hepatosplenoscintigraphy continues to be used for diagnostic purposes.
Frequently asked questions about fatty liver disease
Which doctor should I contact?
A hepatologist specializes in liver diseases.
How to determine fatty hepatosis?
Unfortunately, the disease has no specific symptoms. A comprehensive examination allows you to identify deviations.
Can hepatic steatosis be cured?
With proper and timely therapy, changes in the liver are reversible. The main thing is to strictly follow all the doctor’s instructions, stick to your diet, and give up alcohol and “harmful” foods.
Causes of liver steatosis
What is the cause of liver steatosis , why, according to statistics from the European Association of Hepatologists, is this disease widespread as an epidemic? The most common opinion is poor nutrition and a sedentary lifestyle. And this is a big mistake. The cause of steatosis is not an unhealthy lifestyle, but hormonal and metabolic changes; this is a disease that, in addition to lifestyle correction, nutrition and physical activity, also requires observation by a hepatologist and endocrinologist!