Reflux esophagitis is a chronic disease associated with inflammation of the esophageal mucosa due to the reflux of gastric contents into the esophagus (reflux). Reflux esophagitis is a manifestation of gastroesophageal reflux disease, which in turn most often develops against the background of a hiatal hernia.
Reflux esophagitis is perhaps the most common disease of the gastrointestinal tract. According to various studies, about 50% of the adult population of developed countries experience symptoms of reflux at one time or another, but only 9.5% are diagnosed. This is due to the fact that in mild cases people do not seek medical help.
Complaints with reflux esophagitis
The most common complaint with reflux esophagitis is heartburn. Most often it is perceived as a burning sensation in the chest, sometimes a sour taste in the mouth, and sometimes takes a debilitating form, significantly reducing the quality of life. It occurs when overeating, or eating certain foods, and is often worse when lying down or bending over. Heartburn can also occur on an empty stomach or during prolonged fasting. Heartburn worsens when lying down; in severe cases, it forces patients to sleep in a sitting position.
The second most common symptom of reflux esophagitis is chest pain. The pain is associated with inflammation in the wall of the esophagus. The pain intensifies while eating; patients literally feel the passage of a bolus of food through the esophagus. Analgesics do not relieve pain. Antacids and sometimes drinking cold water provide relief.
Also often with esophagitis, belching occurs, which is associated with a concomitant hiatal hernia.
Often, reflux esophagitis is accompanied by complaints characteristic of other diseases, the so-called extraesophageal manifestations of reflux esophagitis. A dry cough that gets worse after eating or lying down is common. When examining such patients, lung diseases are not detected, but sometimes chronic bronchitis or bronchial asthma are detected, which significantly complicates the diagnosis of reflux esophagitis.
Another common extra-esophageal manifestation of esophagitis is hoarseness and frequent pharyngitis, which are difficult to treat until medications are used to treat esophagitis. Also, with reflux esophagitis, heart rate arrhythmias and tooth decay are not uncommon.
Throat and voice problems
The main symptom of gastroesophageal reflux disease is heartburn, but not all people feel or report it. They may have other symptoms that are more difficult to diagnose. Doctors call these cases "silent reflux," or asymptomatic reflux. The patient may not have heartburn as classically described in textbooks, but they may have various other problems that occur outside the esophagus, such as hoarseness, voice changes, sore throat, or chronic cough. They feel as if there is a lump or hair in their throat and constantly have to clear their throat by coughing and clearing their throat.
Diagnosis of reflux esophagitis
Diagnosis of reflux esophagitis most often does not cause difficulties. For an experienced gastroenterologist, it is often enough to collect complaints and a medical history to suspect a diagnosis of reflux esophagitis.
The most important and informative diagnostic method is gastroscopy (FGDS) .
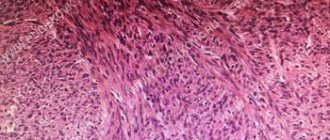
Reflux esophagitis, endoscopic picture
When examining the esophagus, inflammation in its mucous layer, erosion, and ulcers are revealed. According to gastroscopy, the degree of the disease is determined. Sometimes so-called endoscopically negative reflux esophagitis occurs, in which case the wall of the esophagus appears unchanged, although there are complaints.
X-ray of the esophagus with barium - used to diagnose a possible concomitant hiatal hernia; also during this study, it is possible to document the fact of reflux of gastric contents into the esophagus, its severity, and duration. The speed of passage of contrast through the esophagus is also assessed, which makes it possible to judge motility disorders and indirectly judge the presence of inflammation in its walls.
In difficult cases, daily pH measurements or daily impedance measurements are performed to clarify the diagnosis. These studies make it possible to measure acidity in the lumen of the esophagus and identify reflux of gastric contents, determine its nature and the time of contact of aggressive contents with the esophageal mucosa, this is of great importance for developing treatment tactics.
Sometimes, after several years of illness, heartburn either goes away completely or decreases significantly, without treatment, and this is a bad sign, most often indicating the development of complications.
1.Structure of the esophagus
Esophagus
- a muscular tube connecting the throat (pharynx) to the stomach. The length of the esophagus is about 20 centimeters, and its inner surface is a pink mucous membrane. There is a part of the esophagus called the upper esophageal sphincter (UES). This is a group of muscles at the top of the esophagus that work during breathing, eating, belching and vomiting. A person can consciously control this muscle group. The upper esophageal sphincter muscle also holds food and secretions that may come from the windpipe.
The lower esophageal sphincter (LES) is a group of muscles at the lower end of the esophagus where it connects to the stomach. When the lower esophageal sphincter is closed, it prevents acid and stomach contents from moving back out of the stomach. The muscles of the LES are not subject to conscious control.
Diseases of the esophagus
, in fact, not so little. Some of them are quite serious, some do not require complex and long-term treatment. Depending on the severity of the disease, it may be treated by gastroenterologists or thoracic surgeons, who perform operations on the esophagus when necessary for treatment.
A must read! Help with treatment and hospitalization!
Classification of reflux esophagitis
The two most widespread classifications of esophagitis in the world are the Savary-Miller classification, adopted in 1977 and modified in 1997 at the 6th European Gastroenterological Conference, and the Los Angeles classification, also adopted in 1997. It is considered more complete and therefore more often used.
Savary-Miller classification
1st degree - one or more erosions occupying less than 10% of the circumference of the esophagus 2nd degree - merging erosions occupying more than 10, but less than 50% of the circumference of the esophagus 3rd degree - multiple erosions occupying the entire circumference of the lower third of the esophagus 4th degree - complications of reflux esophagitis: esophageal ulcer, stricture, Barrett's esophagus
Los Angeles classification of esophagitis
Grade A - damage to the wall no more than 5 cm long, within one fold of the mucosa Grade B - damage more than 5 cm long, but within one fold Grade C - damage more than 5 cm long, occupying up to 75% of the circumference of the esophagus Grade D - damage to the mucosa occupying 75% or more of the circumference of the esophagus
Complications of reflux esophagitis
With inadequate therapy, or its insufficient effectiveness, or in the absence of treatment, reflux esophagitis continuously progresses and can lead to quite serious complications. The most common complication is the development of Barrett's esophagus, in simple terms, this is a situation when the structure of the cells of the esophageal mucosa, under the influence of constant inflammation, begins to change its structure. This process is called dysplasia. Barrett's esophagus is considered a precancerous disease, as it significantly increases the risk of developing esophageal adenocarcinoma (cancer).
Also a frequent complication is the development of severe erosive ulcerative lesions of the esophageal mucosa, which in turn are complicated by either bleeding or stricture (narrowing) of the esophagus. Bleeding can be either chronic, invisible to the patient, or acute, quite profuse and life-threatening. With chronic bleeding from erosions and ulcers of the esophagus, the patient feels unmotivated weakness and, when taking a blood test, anemia is detected.
Stricture of the esophagus (narrowing of the lumen), as mentioned above, develops against the background of erosive esophagitis, or ulcerative lesions of the esophageal mucosa, in the absence of adequate treatment. Signs of a narrowing of the esophagus include difficulty swallowing and vomiting of food that has just been eaten. Esophageal stricture requires immediate treatment
3.Diagnosis of diseases
Of course, depending on the symptoms of which disease the doctor sees during the initial examination and consultation, methods for further diagnosing diseases of the esophagus will be selected individually. Let's talk about some of them:
- Upper endoscopy, FGDS (esophagogastroduodenoscopy)
. In this procedure, a flexible, thin tube with a camera on the end (endoscope) is inserted into the esophagus through the mouth. An endoscope allows you to examine the stomach and duodenum (small intestine). - pH monitoring of the esophagus
. A probe that monitors pH levels is inserted into the esophagus. This method is used to diagnose GERD and monitor the progress of GERD treatment. - X-ray examination
with preliminary administration of drugs containing barium. This method is usually used to determine the causes of difficulty swallowing. - Biopsy
. A method for diagnosing diseases of the esophagus, in which a sample of esophageal tissue is taken using endoscopy, which is then examined under a microscope. - Confocal laser endomicroscopy
. This is a new procedure in which a microscope is inserted into the patient's esophagus. Endomicroscopy can be a good alternative to biopsy.
About our clinic Chistye Prudy metro station Medintercom page!
Treatment of reflux esophagitis
Treatment of esophagitis is carried out both conservatively and surgically. Of course, the overwhelming majority of patients are treated conservatively by a gastroenterologist. The goal of treatment is to remove symptoms, prevent the development of complications, and improve quality of life. You need to understand that it is often impossible to cure reflux esophagitis with conservative methods once and for all, and either constant or periodic maintenance therapy is required. The only way to radically get rid of esophagitis is through surgery.
Lifestyle change
The first thing a competent gastroenterologist will recommend when treating reflux esophagitis is optimizing the patient’s lifestyle, and it must be said that this is the most difficult thing in treating this disease. If you are overweight, you should lose weight. Patients are recommended to eat frequent meals, at least five times. Last meal 4 hours before bedtime. It is recommended to sleep with the head end raised, and you should not put pillows on it, but raise the head end of the bed. Alcoholic drinks, coffee, tea, and sour foods are prohibited. Limiting physical activity associated with heavy lifting and working in an inclined position.
So let's summarize what you need to change in your life:
- after eating, avoid bending forward and not lying down;
- sleep with your head elevated;
- do not wear tight clothes and tight belts;
- avoid large meals;
- do not eat at night;
- limit the consumption of foods that cause a decrease in LES pressure and have an irritating effect (fats, alcohol, coffee, chocolate, citrus fruits);
- stop smoking;
- normalize body weight, if it is excess;
- Avoid taking medications that cause reflux (anticholinergics, sedatives and tranquilizers, calcium channel inhibitors, beta blockers, theophylline, prostaglandins, nitrates).
How often does laryngopharyngeal reflux occur?
Typical GERD has been on the rise in recent decades, especially in the United States and Western Europe. Its frequency is estimated at 10-20% of the general population.
Calculating the frequency of LPR is not so easy - the symptoms are usually masked and can be explained by many other diseases.
There is a large study looking at the incidence of laryngopharyngeal reflux among people with heartburn. The average frequency was 32.8%, and in people with erosive lesions of the esophagus the frequency was higher, up to 34.9%. With non-erosive GERD it is slightly less - 30.5%.
The actual incidence of laryngopharyngeal reflux without the typical manifestations of GERD is not known, although scientists suspect that it is much more common than we think.
Conservative therapy
For conservative therapy, the following groups of drugs are used:
- antacids and alginates
- proton pump inhibitors
- prokinetics
Antacids and alginates
Antacids and alginates, topical preparations most often containing aluminum and magnesium salts, these drugs act locally, are not absorbed into the blood and do not have a systemic effect. Their advantage is safety of use, but there is also a disadvantage, a short duration of action. Antacids are not used as an independent method of treatment, but are used as first aid for heartburn, and as an intensification of therapy for the speedy healing of erosions and ulcers of the esophagus. Preparations in the form of gels with alginic acid have proven themselves to be the best, which, when interacting with acid in the lumen of the stomach, form foam, thereby increasing the duration of action of the drug and its effectiveness. Antacids are most often prescribed 40 minutes after meals and at night, or on demand in case of heartburn.
Proton pump inhibitors (PPIs)
Today they are the main drugs in the treatment of reflux esophagitis, these include the well-known omeprazole, lansoprazole, rabeprazole, etc. These are systemic drugs, they block the transport of hydrogen molecules into the parietal cells of the stomach, responsible for the secretion of hydrochloric acid, and how do we We remember from the school chemistry course, this acid consists of a molecule of hydrogen and chlorine, no hydrogen, no acid. These drugs have revolutionized the treatment of reflux esophagitis, significantly improving the outcome and reducing the number of complications. Previously, H2 histamine receptor blockers were used, which were much less effective and had more side effects. It must be said that these drugs are sometimes used now in combination with PPIs to enhance the effect. The main disadvantage of proton pump inhibitors (PPIs) is their fairly rapid removal from the blood, which requires repeated use throughout the day, and even with double use, so-called acid breakthroughs are described, when, more often at night, the acidity of gastric juice sharply increases. Most often, PPIs are prescribed 20 mg twice a day 20 minutes before meals, morning and evening for 6 to 8 weeks. Then maintenance therapy is prescribed at 10 mg per day or 10 mg twice a day.
Prokinetics
Prokinetics are drugs that improve and normalize peristalsis of the gastrointestinal organs, including the esophagus. The most commonly prescribed drug is itopride, which is considered the most effective and safe drug. Motilium is also prescribed. The previously popular cerucal has recently been deprecated due to its central effect on the brain. Prokinetics are prescribed 1 tablet three times a day 20 minutes before meals. A course of 2 weeks is recommended.
Problems of conservative therapy
The vast majority of patients with reflux esophagitis are treated conservatively, achieving good functional results, but unfortunately, therapy is not always effective. As we wrote above. The cause of reflux esophagitis is the reflux of gastric contents into the esophagus. So the first problem with conservative therapy is that it does not eliminate the cause, but only relieves the symptoms. With conservative therapy, reflux remains, but is no longer acidic, and therefore patients do not feel any complaints. Although some researchers believe that due to the neutralization of acid, bile begins to flow into the esophagus, since it ceases to be inactivated in the stomach, and bile is an even more aggressive environment for the development of complications of esophagitis. Although it should be noted that this is still a theory that has not received sufficient confirmation. But at the same time, a number of scientists associate the growth of esophageal cancer with this hypothesis. Since, despite the widespread use of PPI drugs, the incidence of esophageal cancer is steadily increasing.
Taking medications in itself can cause complications. Evidence has been obtained that proton pump inhibitors increase the risk of stroke, osteoporosis and heart attack, and although the risk is not quite high, about 0.4 - 0.6% per year, it is still there.
Well, perhaps the main thing is that the effect of conservative therapy is temporary and is not always sufficiently effective. So, 6 months after stopping therapy, complaints return in 40-50% of patients, and after 12 months in 80-90%, that is, most patients are forced to take medications daily for many years. Considering the sufficient safety of the drugs, this may not be scary, although it certainly reduces the quality of life. But the problem lies in the fact that with long-term therapy, after three or five years, the effectiveness of the drugs decreases and in 20 - 30% of patients complaints reappear and complications of esophagitis develop, despite the constant use of the prescribed drugs.
Effective treatment of chronic cough in patients with gastroesophageal reflux disease
I.G. Danilyak, Yu.I. Nymann, A.D. Palman
Cough occurs as a result of irritation of cough C receptors located in the upper and lower respiratory tract, pleura, diaphragm, pericardium and esophagus. With the development of inflammatory and other pathological processes in them, these C-receptors are excited, since they are stimulated primarily by inflammatory mediators (prostaglandins, bradykinin, substance P, etc.).
In medical practice, recognition of the etiology of prolonged and chronic cough is of greatest importance. To establish its cause, it is recommended, in addition to a thorough analysis of clinical and laboratory data, to conduct a comprehensive instrumental examination, including an in-depth X-ray examination of the chest (X-rays in 3 projections, computed tomography), a study of the function of external respiration, and, if indicated, tracheobronchoscopy and daily gastroesophageal pH. measurements, consultation with an otolaryngologist [5, 7].
Here is an observation.
Patient B., 66 years old, was admitted to the hospital therapeutic clinic of the MMA named after. I.M. Sechenov with a diagnosis of chronic bronchitis in the phase of subsiding exacerbation, hypertension of the 1st degree.
Upon admission - complaints of cough, periodically paroxysmal, sometimes with the discharge of a small amount of thick light sputum, heartburn. Considers himself sick for a year. The onset of the disease is associated with an acute respiratory infection, which left a cough. Periodically, the cough, mostly nonproductive, intensified, often occurring in the form of an attack at night. She was examined on an outpatient basis. Persistent cough was regarded as a manifestation of chronic bronchitis, for which treatment was carried out with antitussive, expectorant and bronchodilator drugs, as well as periodically with antibacterial drugs. However, the therapy was ineffective.
For hypertension, the patient has been treated with enalapril for the past several months. I've never smoked. No professional (she worked as a design engineer before retiring) and household hazards that could lead to pathology of the respiratory system, as well as a hereditary predisposition to them, have not been identified. There is no allergic history.
On examination: the condition is satisfactory, the physique is normosthenic. Peripheral lymph nodes are not palpable. There is no swelling. Both halves of the chest are evenly involved in the act of breathing. Percussion sound is pulmonary, in the lower parts - with a boxy tint. The lower border of the lungs percussion is within normal limits. On auscultation, breathing is harsh, wheezing is not heard. Respiratory rate at rest is 16 per minute. The boundaries of cardiac dullness are within normal limits. Heart sounds are rhythmic, there are no murmurs. Heart rate - 78 per minute. Blood pressure - 145/90 mm Hg. Art. The abdomen is soft and painless. The liver and spleen are not palpable and are not enlarged by percussion. The stool is regular, urination is not impaired.
General blood and urine analysis: no pathology. IgE level is within normal limits.
General analysis of sputum: mucous membrane, leukocytes - 5-10 per field of view, no eosinophils found, significant admixture of saliva.
X-ray examination: the chest is cylindrical, the diaphragm is raised by one intercostal space, mobile, deformed by adhesions on the left; sinuses are free. Pulmonary emphysema, infiltrative changes are not determined. The heart is horizontal, the left ventricle is slightly enlarged; the aorta is dilated and thickened.
Computed tomography of the chest did not reveal any space-occupying formations or areas of pathological density in the lung parenchyma. The walls of the bronchi are moderately compacted. The trachea and large bronchi are freely passable and not deformed. The mediastinal lymph nodes are not enlarged. The aorta, pulmonary trunk and their branches are not dilated.
Indicators of pulmonary ventilation function and the structure of lung volumes are within normal limits. General bronchial resistance is not increased. After inhalation of Berotec, FEV1 increased by 7%.
Tracheobronchoscopy revealed signs of minor catarrhal bronchitis, but no other pathology was detected.
Echocardiography: the aortic root and its ascending section are of normal size, the aortic walls are moderately compacted, the bases of the aortic valve leaflets and the fibrous ring of the mitral valve are compacted.
Consultation with an otolaryngologist: free nasal breathing. There is no swelling of the nasal mucosa. No foci of chronic infection were identified. Indirect laryngoscopy did not reveal any pathology.
The patient was assumed to have chronic obstructive bronchitis. However, the absence of the main risk factors for the development of this pathology (never smoked, no burdened professional history), as well as the effect of outpatient treatment and the therapy we prescribed with inhalations of Atrovent and Lasolvan, together with inconclusive data from X-ray examination and tracheobronchoscopy, did not allow us to settle on this diagnosis. The paroxysmal nature of the cough, its occurrence, including at night, could indicate a cough variant of bronchial asthma, but an uncomplicated allergic history and the results of the studies denied this possibility.
Taking into account data on the frequent occurrence of cough as a side effect during treatment with angiotensin-converting enzyme inhibitors (the patient had been taking enalapril for a long time), this drug was discontinued, but the cough did not disappear and her health did not improve.
Since cough is often associated with gastroesophageal reflux (GER) and the patient complained of heartburn, further diagnostic search was aimed at excluding gastroesophageal reflux disease (GERD), and therefore esophagogastroduodenoscopy (EGDS) was performed. The esophagus is freely passable. Starting from its upper third, the mucous membrane is covered with fibrinous plaque; in the lower third, linear erosions are detected on all walls. The cardia does not close; a hiatal hernia is detected. In the stomach cavity there is a small amount of clear liquid without pathological impurities. Peristalsis can be traced along all walls. The folds of the gastric mucosa are medium in size. In the prepyloric part of the antrum there are multiple confluent erosions, some of them are covered with fibrin mixed with hematin. There were no red blood streams during the study. The mucous membrane of the duodenal bulb is without inflammatory changes, the postbulbar region is not changed. Conclusion: fibrinous-erosive esophagitis of the II degree. Hiatal hernia. Erosive gastritis with signs of bleeding. Given the latter finding, 24-hour gastroesophageal pH monitoring was not performed. The characteristic pathological picture obtained from endoscopy allowed us to conclude that the patient had GERD.
The identified pathology of the esophagus and stomach served as the basis for starting adequate therapy: diet (exclusion of rough, spicy foods, small meals), omeprazole, Venter, Motilium, amoxicillin, metronidazole and dicinone were prescribed. After a few days, the condition improved - the cough decreased and the night attacks stopped, and the heartburn disappeared. By the end of the 3rd week of treatment, the cough had completely stopped.
Upon discharge, it is recommended to follow a diet, limit spicy foods, eat small meals, sleep with the head elevated, continue taking omeprazole, Motilium, Venter. During the control endoscopy (after a 6-week course of therapy), a complete disappearance of erosions in the stomach and a significant decrease in the symptoms of esophagitis were noted. Maintenance anti-relapse therapy was prescribed (single dose of famotidine at night). Observation by a gastroenterologist is recommended.
Thus, the identification of GERD in the patient and the exclusion of other possible causes made it possible to associate the occurrence of cough with a pathological process in the esophagus (grade II reflux esophagitis); The treatment prescribed for this occasion led to the disappearance of the cough.
GERD (reflux esophagitis) is a pathology of the esophagus, characterized by the occurrence of inflammation, erosive and ulcerative changes and (or) functional disorders as a result of the reflux of aggressive gastric or intestinal contents into the esophagus. Based on the severity of the endoscopic picture of the esophageal mucosa, 5 degrees of reflux esophagitis are distinguished, but even in the absence of visible morphological changes, histological examination reveals signs of an inflammatory process. Among the complaints (heartburn, belching, burning behind the sternum, etc.), patients also indicate cough [4].
A study of the etiology of cough has shown that GER, along with bronchial asthma and postnasal drip, is the most common cause of its occurrence [7, 10, 13]. During GER, the pH in the esophagus decreases, a sour taste appears in the mouth, and a cough occurs, which can appear without microaspiration, only due to a reflex mechanism. In the latter case, the typical symptoms of GERD (burning behind the sternum, sour taste in the mouth, regurgitation) are not typical. Special studies have shown that more than 50% of patients do not have typical symptoms of reflux, and in the rest they occur only after a coughing attack. It is indicated that in some patients cough may be the only manifestation of GERD [11, 12].
There is no doubt about the role of GER in the formation of bronchial obstruction; a chronological relationship between episodes of GER and the occurrence of the latter has been proven. Therapeutic elimination of reflux leads to a significant reduction or complete disappearance of broncho-obstructive disorders [6].
The pathogenesis of cough and broncho-obstructive syndrome due to GER involves vagal-mediated reflexes from the distal esophagus to the muscles of the trachea and bronchi through stimulation of acid-sensitive receptors of the esophagus. The influence of tachykinins released from sensory neurons on the formation of acid-provoked bronchoconstriction has been shown, as well as the important role of bradykinin in this process [14].
The influence of GER on bronchial reactivity has been demonstrated. In patients with bronchial asthma combined with GERD, a correlation was found between provocative doses of methacholine, which caused a decrease in expiratory volume by 20%, and the initial number of reflux episodes [15]. There is evidence indicating the influence of GER on the course of bronchial asthma, as well as the possibility of its occurrence due to GERD [2, 6, 9].
Reflexively occurring cough and broncho-obstructive syndrome are the most common pulmonary complications of GERD; respiratory pathology caused by repeated microaspirations (inflammatory diseases of the upper respiratory tract, tracheitis, bronchitis) is less common. It is indicated that patients with GERD may develop such serious complications as a result of macroaspiration, such as aspiration pneumonia, chronic obstructive bronchitis, and pulmonary fibrosis [1, 6, 9, 10].
In the genesis of aspiration pneumonia in patients with GERD, a certain role is played by impaired motility of the esophagus [1], especially dysfunction of its sphincters. The lower sphincter performs a protective function in relation to gastroesophageal reflux, and the upper one determines the degree of possible aspiration of gastric contents from the esophagus into the bronchi during GERD, which is associated with a decrease in the tone of the esophageal sphincters [3]. Inhalation of acidic gastric contents causes the destruction of surfactant, instability of the alveoli, the appearance of atelectasis, increased permeability of the pulmonary vessels, and alveolar edema [6]. Ingress of aspirated material into the respiratory tract leads to damage to the bronchial mucosa and thinning of the alveolar septa. Some researchers view airway aspiration as a “triple threat”: mechanical obstruction, chemical pneumonitis, and bacterial pneumonia [8].
As for the prevention and treatment of reflexively occurring pulmonary complications (cough, bronchial obstruction) in patients with GERD, its effective therapy is usually sufficient. For respiratory pathology that develops as a result of repeated microaspirations or as a result of macroaspiration (bronchitis, aspiration pneumonia, etc.), in addition to rational therapy for GERD, special treatment is necessary taking into account the characteristics and nature of the emerging pathological process.
It should be emphasized that in all cases of unspecified etiology of chronic uncorrectable cough, even in the absence of dyspeptic complaints, the possibility of its connection with GER should be kept in mind.
Literature
1. Avdeev S. N. Aspiration pneumonia // Russian. honey. magazine - 2001. - No. 21. - P.934-939.
2. Beytuganova I. M., Chuchalin A. G. Reflux-induced bronchial asthma. // Russian. honey. magazine - 1998. - No. 6. - P.1102-1108.
3. Geller L.I., Glinskaya T.P., Petrenko V.F. Tone of the esophageal sphincters in patients with bronchial asthma. // Wedge. honey. - 1985. - No. 12. — P.39-41.
4. Grigoriev P. Ya. Recommendations (protocols) for diagnosis and treatment of patients with diseases of the digestive system. // Practicing doctor. - 2002. - No. 1. - P.3-5.
5. Danilyak I. G. Cough: etiology, pathophysiology, diagnosis, treatment. // Pulmonology. - 2000. - No. 3. - P.33-38.
6. Fedoseev G. B. Mechanisms of bronchial obstruction. — St. Petersburg: Med. information agency, 1995. - P. 216.
7. Chuchalin A. G., Abrosimov V. N. Cough. - Ryazan, 2000. - 102 p.
8. Bartlett JG, Gorbach SL The triple threat of aspiration pneumonia. // Chest. - 1975. - Vol.68. — P.560-566.
9. Harding SM Gastroesophageal reflux and asthma: insight into the association. // J. Allergy Clin. Immunol. - 1999. - Vol.104. — P.251-259.
10. Irwin RS, Boulet LP., Cloutier MM et al. Managing cough as a defense mechanism and as a symptom. A consensus panel report of the American College of Honorable Physicians. // Chest. - 1998. - Vol.114, Suppl.2. — P.133-181.
11. Irwin RS, Zawacki JK, Curley FJ et al. Chronic cough as the sole presenting manifestation of gastroesophageal reflux. //Am. Rev. Respira. Dis. - 1989. - Vol.140. — P.294-300.
12. Mansfield LE, Hameister HH, Spaulding HS et al. The role of the vagus nerve in airway narrowing caused by intraesophageal hydrochloric acid provocation and esophageal distention. //Ann. Allergy. - 1981. - Vol. 47. - P.431-434.
13. Mello C. J., Irwin R. S., Curley F. J. Predictive values of the character, timing, and complications of chronic cough in diagnosing its cause. //Arch. Intern. Med. - 1996. - Vol. 156, No. 9 - P. 997-1003.
14. Ricciardolo FLM, Rado V., Fabbri LM et al. Bronchoconstriction induced by citric acid inhalation in guinea pigs. //Am. J. Respira. Crit. Care Med. - 1999. - Vol.159. — P.557-562.
15. Vincent D., Cohen-Jonathan AM, Leport J. et al. Gastro-esophageal reflux prevalence and relationship with bronchial reactivity in asthma. //Eur. Respira. J. - 1997. - Vol.10. — P.2255-2259.