- Diagnostics
- Treatment and prognosis (outcome)
- Treatment of metastases of other tumors to the liver
- Combined treatment
The total number of patients with liver metastases is approximately one third of the total number of patients with malignant tumors.
In Russia, about 450 thousand new cancer patients are diagnosed annually.
A significant proportion of them already have liver metastases; in other patients, liver metastases can be detected at different times after the diagnosis of cancer.
The number of all patients with liver metastases in Russia is more than 100 thousand, which is tens of times greater than the number of all patients with primary tumors of the liver and intrahepatic bile ducts.
Metastases to the liver are most often observed in patients with primary tumors of the colon, lungs, stomach, pancreas, and breast. Cancers of the biliary tract, esophagus, ovaries, prostate, kidneys, and melanoma less commonly affect the liver.
Most often, metastases in the liver repeat the structure of primary tumors. However, in some cases, metastases differ from primary tumors in the degree of differentiation (maturation) of tumor cells, which makes it difficult to determine the identity of the primary tumor.
As a rule, metastatic liver tumors are rarely observed in patients with cirrhosis. This can be explained by poor conditions for fixation and proliferation of tumor cells in the scarred organ.
Metastatic liver cancer is usually characterized by rapid progression and the absence of specific laboratory and clinical signs.
Increasing weakness (36%), loss of appetite, weight loss (18%), mild pressing pain (72%) in the stomach, enlarged liver (22%), periodic rise in temperature (20%) - indicate significant liver damage, involvement into the process of both lobes of the organ.
All patients with liver metastases are divided into two groups, regardless of the sources of metastasis:
- patients with single liver metastases;
- patients with multiple liver metastases.
(More than three metastases are considered multiple).
In patients with single metastases, the symptoms of the disease resemble those of primary liver cancer (liver enlargement and dull pain in the right hypochondrium with small tumor sizes).
In patients with multiple metastases, local and general symptoms are more pronounced and are characterized by increasing liver failure and complications in the form of obstructive jaundice.
Some patients experience swelling of the lower extremities and dilation of the veins of the anterior abdominal wall as a result of compression of the inferior vena cava. 30% of patients already at the time of diagnosis have ascites (fluid accumulation in the abdomen) due to damage to the peritoneum.
Causes and risk factors
The exact causes of liver cancer have not yet been established. Most often, a malignant lesion occurs against the background of a long-term inflammatory process in the liver tissue. Most often, the first signs of liver cancer are detected against the background of cirrhosis. In regions where viral hepatitis is widespread, cases of liver cancer are detected much more often. Thus, approximately 25% of all patients with signs of liver cancer are diagnosed with viral hepatitis C, and approximately 40% are chronic carriers of the hepatitis B virus.
Other risk factors that increase the risk of developing liver cancer include:
- poor nutrition leading to obesity;
- drinking large amounts of alcohol;
- long-term use of drugs that have hepatotoxicity (including steroids, oral contraceptives);
- the influence of external factors - toxins that damage liver cells (vinyl chloride, aflatoxins);
- long history of diabetes mellitus;
- Budd-Chiari syndrome (these are episodes of thrombosis in the hepatic veins);
- hereditary pathologies - Wilson's disease, hemochromatosis, tyrosinemia, glycogenosis, alpha-trypsin deficiency, intestinal polyposis.
In some cases, the causes of liver cancer cannot be determined, and the cases are considered idiopathic.
Liver cancer symptoms
The first signs of liver cancer are not specific; they are also possible in many other pathologies of the organ (acute and chronic hepatitis, alveococcosis, cirrhosis, damage to the bile ducts or liver metastases). In the early stages, the pathology may not manifest itself in any way, since the organ has a high reserve. Therefore, liver cancer is often first detected by ultrasound, which is performed for various pathologies of internal organs located near the liver. If the tumor is significant in size, patients may experience the following complaints and manifestations:
- decreased or complete lack of appetite (anorexia);
- decrease in the amount of hemoglobin and red blood cells;
- discomfort, pain in the hypochondrium, closer to the right side or in the upper abdomen;
- nausea, vomiting with bile or food;
- an increase in the size of the abdomen due to the growth of a tumor formation that can be felt through the abdominal wall;
- ascites (growth of the abdomen due to the accumulation of fluid in it);
- weight loss, sometimes very significant (up to several kilograms in a couple of months);
- yellowing of the skin and whites of the eyes (development of jaundice);
- severe skin itching;
- nose bleed;
- stool disorders - alternating constipation or diarrhea;
- change in color of urine (dark) and stool (discoloration);
- expansion of small capillaries under the skin (formation of telangiectasia).
As the tumor grows and disintegrates, general malaise, fever, and weakness may occur.
Signs of liver metastases
During the initial period of metastasis growth, with its small size, there are no manifestations. There are no pain receptors in the liver tissue, so pathological processes in it often go unnoticed by the patient. It becomes possible to suspect something only in the later stages, when there is a significant increase in the organ’s size, and then the baroreceptors in the liver capsule begin to send painful signals. Or the bile ducts become blocked and symptoms of jaundice appear.
Therefore, it is so important to carry out preventive examinations and monitoring of cancer patients, including after surgery to remove the primary tumor. The volume and frequency of examinations must be determined by the oncologist. Their timely implementation will help early diagnosis in case of awakening of “dormant”, inactive cancer cells scattered in the body.
As the disease progresses, nonspecific symptoms appear, and their severity gradually increases.
Malignant organ damage may be indicated by:
- indigestion (dyspepsia). There is bloating, flatulence, nausea, alternating constipation and diarrhea, abdominal discomfort;
- dull pain in the right side;
- liver enlargement;
- excessive weakness, fatigue;
- apathy, insomnia;
- decreased appetite;
- unexplained weight loss.
Later join:
- increase in abdominal volume due to the appearance of fluid (ascites);
- pathological elements on the skin - spider veins, dilated venous network, pigment spots, darkening of the skin (including pigmentation of the palms);
- vomit;
- change in appetite, aversion to certain foods;
- bleeding from the nose, esophagus, intestines;
- enlargement of the mammary glands in men.
If the tumor node is located along the path of bile outflow, then as it grows, manifestations of jaundice begin. The sclera (icteric sclera), skin, and oropharyngeal mucosa turn yellow.
The appearance of such symptoms does not necessarily mean liver cancer. The listed signs can also occur with cirrhosis, hepatitis, cholecystitis, pancreatitis, and with many other diseases of the digestive tract, when taking certain medications, or exposure to toxins. Therefore, it is important to immediately begin an examination and find out the cause.
The list of symptoms for liver metastases is long and among them there is not a single specific one that could accurately determine the diagnosis. Therefore, a lot of additional research and analysis is being carried out.
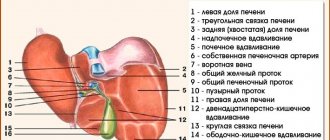
Types of primary liver cancer
There are several classification options for primary liver cancer. There are various types of tumors, which differ in course and prognosis. Experts identify several of the most typical types of primary liver cancer (the tumor is formed from the cells of the organ).
Hepatocellular cancer
is the most common tumor (carcinoma) that occurs in the liver area.
As the name suggests, these tumors form in hepatocytes, which form the basis of liver tissue. The course of hepatocellular cancer is possible in two clinical forms - diffuse
(when a large part of the liver is affected) or
nodular
(one focus is formed - a node or several areas).
A more favorable variant of this cancer is possible - fibrolamellar carcinoma
, with it there are possibilities for more active treatment.
Cholangiocarcinoma
is a malignant tumor that originates in the area of the bile ducts.
Cholangiohepatoma
is a mixed type of tumor in which cancer cells originate both in the area of hepatocytes and in the area of epithelial cells in the bile ducts.
Variants of tumors such as angiosarcomas, mesodermal formations
are lesions that grow from lymphatic capillaries, blood vessels or connective tissue cells.
Possible hepatoblastoma
cystadenocarcinoma
is also identified . It occurs as a result of the degeneration of a benign tumor.
The story of Marina from Chelyabinsk, a patient at the Ikhilov Cancer Center
When the doctor was doing my annual physical, she touched my sternum and it hurt a lot. When the results of the blood tests came back, it turned out that my bilirubin was elevated. Nevertheless, another month and a half probably passed before I was given a final diagnosis. Having learned that I have a malignant liver tumor (cholangiocarcinoma), I decided to undergo treatment in Israel, at the Ichilov Oncology Center.
Israeli doctors confirmed the diagnosis: I had stage 1 cancer. They performed a resection on me - removing part of the liver with the tumor. The treatment lasted 6 months, then remission began, which has been going on for 14 months. Doctors say that I have a good chance of a complete cure, because... the operation was carried out on time.
I was pleasantly surprised by the attitude of the staff towards patients. Everyone understood that I was scared and provided support and care. I knew that I was completely safe in this institution.
Stages of liver cancer
The basis of clinical classification is the TNM system. It is based on the pathological features of the tumor, and its prognosis depends on the stage of liver cancer. Each classification criterion will indicate the presence or absence of certain changes.
- T is the growth and spread of the tumor, the presence of several tumor nodes, the size of the largest of them, as well as the growth of the tumor focus into neighboring areas.
- N - reflects tumor metastasis to nearby (regional) or distant lymph nodes;
- M - indicator reflects metastasis of liver cancer to other organs.
In addition to these criteria, the course of the disease, the features of its treatment and the prognosis of liver cancer are influenced by the presence of fibrosis and the degree of differentiation of tumor cells. The lower the degree of differentiation, the more the cancer cells differ from healthy ones and the more aggressive the cancer. These indicators have an extremely negative impact on survival, regardless of TNM stage.
One of the classification options is based on blood parameters for liver cancer. They determine the functional activity of the liver and the severity of cirrhosis. The assessment is carried out based on the levels of total bilirubin, serum creatinine, and blood coagulation parameters.
Metastatic liver diseases: why do they appear so often?
The frequent appearance of cancer cells in hepatocytes (liver cells) is due to the characteristics of blood flow in the organ. The liver performs many important functions in the body; all blood passes through it every hour and more than once. In just a minute, 1.5 liters of blood flows through the liver vessels (about 30% of the total blood volume in the body). To filter and purify the blood, it must be slowed down and redistributed among small-diameter vessels (capillaries). This is what happens in the liver lobules. With a slow, repeated flow in narrow vessels, there is a high probability of cancer particles settling.
Most potential metastases (cells from a tumor node) are recognized by the body's immune system as foreign and are destroyed. When defense mechanisms fail, they continue to circulate in the blood and find places for further settlement. Cancer cells, which are particles of the primary (main) tumor, can remain in one of the hepatic capillaries and become the basis for the development of a metastatic cancer node in the liver. Secondary tumors are much more common here than primary cancers (ratio approximately 9/1). There are often cases when metastasis is detected by chance during examination for other diseases. In this case, the patient does not know about the presence of a primary tumor.
Primary liver cancer: diagnosis
All people who are at high risk for developing liver cancer are regularly screened. First of all, doctors look for ultrasound signs
Liver cancer in people suffering from chronic inflammatory processes of the organ have different degrees of cirrhosis. They are advised to perform an ultrasound examination every six months, even in the absence of complaints.
In addition, they are advised to perform laboratory blood tests to determine the tumor marker of primary liver cancer - AFP
(stands for alpha-fetoprotein). With this type of observation, it is possible to identify tumor lesions at an early stage (there are no symptoms or complaints yet), when the cancer can be radically cured. Changes in tests for liver cancer with an increase in AFP typically occur in up to 50-90% of patients. Levels greater than 400 ng/mL may occur in individuals with large tumors or rapidly growing tumors. But a temporary increase in the indicator is possible against the background of cirrhosis or inflammation of hepatocytes. However, high AFP in combination with ultrasound data and MRI of the liver confirms the diagnosis in almost 100% of patients.
Performing a CT
or
MRI with contrast
helps to identify a tumor and clarify its size and location, which is important for drawing up a treatment plan for liver oncology.
If all this data is not enough to make a diagnosis, a percutaneous biopsy
(puncture or aspiration) under ultrasound control. The risk of complications with such diagnostic methods is minimal.
Characteristics by stages
Stage 1. The most favorable for treatment: small tumor sizes, the area of segment damage is no more than ¼. The chances of recovery are high.
Stage 2. The neoplasm reaches sizes up to 5 centimeters. Adjacent liver segments are affected. The outer lining of the liver is destroyed. There is no metastasis. The survival prognosis is worse than at stage 1, but remains positive.
Stage 3. The tumor is up to 8 centimeters and has grown into neighboring tissues and organs. Secondary lesions appear. There is a decrease in immunity. Organs damaged by metastases malfunction.
Stage 4. The disease cannot be completely cured. The size of the tumor is over 8 centimeters. Metastases are spreading everywhere. The main systems of the body fail. If metastases penetrate the brain, life counts for months (3-4 months). If not, the patient can live up to 5 years.
Liver cancer treatment methods
If the diagnosis of liver cancer is confirmed, treatment must be started immediately. It will be long and includes several stages. In addition, depending on the type of tumor, its size and location, several methods are combined. The main method is surgical removal of cancer
– resection of part of the liver or its complete removal with transplantation of a donor organ.
If resection is not possible and there are no suitable donors for transplantation, doctors can use non-resection therapy
- percutaneous ethanol injections, radiofrequency ablation therapy, arterial embolization or chemoembolization of tumor vessels. Traditional treatment of primary liver cancer is also possible - chemotherapy, the use of radiotherapy, targeted drugs or a combination of several techniques.
In the initial stage of liver cancer, surgery will be the main method of treatment. The tumor is resected within healthy tissue. One-stage resection and two-stage surgery with preliminary ligation or embolization of the portal vein are possible.
Contraindications to such an intervention include damage to distant lymph nodes and cancer metastasis. However, if the remaining portion of the liver is not enough for its full functioning, if the functions of the organ are significantly impaired, there are signs of liver failure, the tumor has grown into the hepatic vein, or affects the portal system, doctors resort to alternative methods of therapy.
If the tumor develops against the background of cirrhosis, the only radical treatment method is organ transplantation
. However, the criteria for transplantation are very strict, so such an operation is performed infrequently.
Chemotherapy
for liver cancer it is used infrequently due to its low activity against cancer cells. It is carried out using cytostatic drugs, but the effectiveness does not exceed 20%. When chemotherapy is combined with immunotherapy for liver cancer, toxic side effects may develop (decreased platelet and leukocyte levels). But the tumor can be reduced to a size where it can be removed. Research into the use of new immunotherapy drugs is still ongoing, but they have shown some success.
Radiation therapy
for liver cancer, it is used to a limited extent, since the development of radiation hepatitis and organ failure is possible. It is used for inoperable tumors in the area of the portal vein and the porta hepatis. Modern equipment is used to minimize damage to surrounding healthy tissue.
One of the promising areas is targeted therapy
in oncology for liver cancer. This is a targeted effect on cancer cells without affecting healthy tissue. It is used in stages when surgery is dangerous or impossible; the drugs help reduce the size of the formation.
How to increase life expectancy?
There are not many methods that can increase life expectancy and improve its quality. After a complete examination, the doctor determines the stage of the oncological process, which determines the treatment tactics.
Treatment
Today, there are several approaches to the treatment of liver carcinoma:
- surgical intervention;
- chemotherapy;
- irradiation.
The extent of the operation depends on the extent of the malignant process. This can be either resection of the affected organ or liver transplantation.
Chemotherapy has three directions, namely:
- embolization Its essence is to inject the drug into the blood vessel feeding the tumor. The drug is used in the form of microcapsules or an oil solution. It is considered the most effective method, as it makes it possible to block the delivery of blood to the tumor site and slow down the progression of the malignant process;
- infusion, when a chemotherapy drug in liquid form is injected into a vessel. The disadvantage of this method is that the drugs act not only on the tumor site, but also on healthy tissue. Among the adverse reactions, it is worth highlighting decreased immunity, hair loss, stomatitis and intestinal dysfunction;
- ablation The main goal of the method is to destroy the tumor by injecting the drug directly into its tissue.
As for radiation therapy, its effectiveness for liver carcinoma is minimal. In this regard, this technique is not used today.
Diet
Proper nutrition plays an important role in treatment. It should be light, but at the same time fully cover the body’s needs, thereby preventing weight loss. The diet includes:
- fractional meals. The interval between meals should not exceed two hours;
- drinking plenty of fluids, which makes it possible to prevent dehydration;
- liquid and puree dishes;
- methods of preparing food - steaming, baking, boiling or stewing;
- warm dishes (neither cold nor hot);
- the emphasis should be on pureed soups, vegetables, fruits, low-fat milk and cereals (buckwheat, wheat, rice, oatmeal);
- Pork, lard, rich broths, fatty fish, chocolate, coffee, offal, sweets with cream, fresh baked goods, canned food, sausages, onions, garlic, spicy seasonings and pickles are prohibited.
After treatment, it is important to undergo regular examinations, which is necessary to control the oncological process. In addition, it is necessary to monitor the functioning of internal organs, the level of hemoglobin, red blood cells, platelets and leukocytes, especially during chemotherapy.
Prevention of liver cancer
Among the main preventive measures are avoidance of alcohol consumption, vaccination against viral hepatitis B, as well as protection against infection with other types of infection. In addition, timely recognition and treatment of liver pathologies, treatment of fatty hepatosis and cirrhosis are important.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.