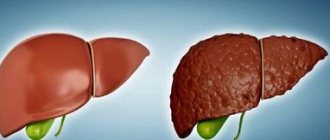
Many diseases are accompanied by an increase in the size and weight of the liver. Hepatomegaly (literally “large liver”) is an integral part of various pathologies, since the organ is involved in all biochemical processes of the body.
Liver hepatomegaly is not a disease, but a symptom of a primary or secondary lesion. It is identified by certain objective signs. Therefore, we immediately warn those who are interested in what this diagnosis means: you should not look for it in the classification of diseases as a separate nosology; it is taken into account in the “Symptoms and Syndromes” section.
Criteria for defining hepatomegaly
We are already so accustomed to the most objective assessment of the size of the liver based on the results of ultrasound or computed tomography that we forget that the first signs of hepatomegaly are determined by the attending physician using the ancient methods of palpation and percussion.
Normally, when examining an adult by percussion, the diameter of the organ along the right midclavicular line should not exceed 12 cm. The lower edge of the right lobe can be palpated in incomplete people; it is soft and slides along the doctor’s fingertips.
In relation to the right costal arch, a protrusion of 1–2 cm is allowed. This is typical for people of asthenic physique. The left lobe of the liver is not palpable. It is located in the upper part of the epigastrium behind the stomach. If a dense formation can be identified in this area, then hepatomegaly can be suspected.
To be sure that the liver is enlarged, the doctor needs to exclude prolapse of the organ in chronic bronchitis and severe pneumosclerosis. An unclear compaction due to a tumor of the kidney, intestines, or enlarged gallbladder may be mistaken for the right lobe of the liver.
In addition to the size, the doctor pays attention to the shape and density of the edge (sharp, rounded, “rocky,” “lumpy,” soft), and the presence of pain during palpation.
..
Prevention
The essence of prevention is to prevent diseases that lead to liver enlargement. To do this, it is important to follow the following recommendations:
- Eat right and do not abuse unhealthy foods, control your intake of carbohydrates and fats.
- Get rid of bad habits.
- Avoid uncontrolled use of medications, carrying out drug treatment only as prescribed by a doctor.
- Follow all hygiene rules to avoid parasitic or viral infection.
- Those who have suffered from liver disease should undergo regular preventive examinations with a doctor.
- Practice regular physical activity, but it should not be excessive.
What causes the pathology?
The causes of hepatomegaly are very diverse. They are associated both with diseases of the liver itself and with other pathologies. Most often, organ enlargement is caused by the following liver diseases:
- viral and non-viral hepatitis;
- hepatosis (fatty hepatosis is a common pathology in obese people), alcoholic and non-alcoholic fatty degeneration;
- tumors (adenoma, hemangioma, carcinoma, cancer metastases from other organs, focal hyperplasia);
- formed cysts;
- amyloidosis;
- liver enzymopathy (with lysosomal lipase deficiency, hepatomegaly appears in 87% of cases);
- Gaucher disease, which causes fat accumulation;
- cirrhosis with irreversible fibrotic disorders with necrosis of hepatocytes;
- thrombosis of the hepatic veins, blockage of the bile ducts due to inflammation of the bladder.
Hepatomegaly is caused by chronic infections and intoxications. The liver ensures the neutralization of toxic substances and poisons; some pathogens “settle” directly inside the organ: with malaria, echinococcosis, granulomatous hepatitis develops with tuberculosis, sarcoidosis, cytomegalovirus infection, mononucleosis, septic pericarditis.
With decompensation of cardiac activity in the liver, venous blood of the inferior vena cava system is retained, the organ swells, a long process causes compression of hepatocytes and their necrosis, followed by replacement with fibrous tissue, cardiac cirrhosis of the liver is formed
Since the liver suffers from pathology associated with metabolic disorders, hepatomegaly is found in hemochromatosis (iron deposition in cells), Wilson-Konovalov disease (copper particles are found in hepatocytes).
Decompensation of cardiac activity caused by right ventricular failure contributes to overflow and increased pressure in the inferior vena cava and its basin. A congestive type of hepatomegaly is observed:
- with the consequences of acute myocardial infarction;
- myocardial dystrophy;
- cardiomyopathies;
- heart defects.
Hepatomegaly is most pronounced in malignant tumors of the lymphatic system (leukemia, leukemia). In this case, foci of additional extramarrow hematopoiesis are formed in the liver or the tissue is saturated with lymphoblastic cells. The liver reaches enormous sizes, occupies most of the abdominal cavity, and its weight reaches 20 kg.
Survival prognosis
To predict the life expectancy of a patient with cirrhosis aggravated by ascites, it is necessary to take into account the advanced stage of the disease.
With continued exposure to unfavorable factors on the organ, cirrhosis worsens, which negatively affects survival.
World statistics show that patients with compensated liver cirrhosis can live more than ten years. If we are talking about decompensated cirrhosis, then up to 40% of patients die within the first three years, three years from the moment the disease is diagnosed.
The Onco.Rehab integrative oncology clinic offers modern methods of treating diseases according to international protocols.
How does hepatomegaly syndrome manifest?
During examination, the doctor identifies signs of hepatomegaly and interprets them in favor of one or another diagnosis. For example,
- the “stony” consistency of the edge of the liver, the bumpiness of the surface indicate the likelihood of cirrhosis or a tumor (new cells grow faster, so bumps form);
- pain on palpation is more typical for hepatitis (inflammation), moderate sensitivity of the edge is observed with steatosis;
- rapid enlargement of the organ is typical for the development of cardiac decompensation, with the capsule stretching, which is accompanied by pain;
- The course of liver abscess and hydatid cyst is distinguished by severe pain.
Pain in the liver area
With a significant enlargement of the liver, the patient experiences the following symptoms of hepatomegaly:
- heaviness, constant bursting pain under the ribs on the right or in the epigastrium, radiating to the side, right side of the abdomen, intensifying with movements;
- an increase in abdominal volume due to the accumulation of fluid in the abdominal cavity (ascites);
- itchy skin rashes;
- yellowing of the sclera and skin;
- nausea, heartburn;
- bowel dysfunction (alternating diarrhea and constipation);
- small angiomas on the skin of the face, chest, abdomen in the form of “spiders” or spider veins.
Jaundice is one of the possible symptoms of pathology
Specific symptoms depend on the cause of hepatomegaly. With hepatitis, the patient's liver enlarges evenly, a thickening appears, which is felt along the lower edge. Palpation is painful. There is yellowness of the skin, signs of general intoxication and inflammation (fever, weakness, headaches, dizziness).
Treatment of hepatomegaly caused by viral hepatitis requires antiviral agents and immunostimulants. With good efficiency, the liver returns to normal size. Cirrhosis differs from hepatitis in the mechanism of destruction of liver tissue. Due to diffuse changes in the liver with areas of necrosis, working hepatocytes are replaced by scar tissue.
Impaired functions are accompanied by a tendency to bleeding, the skin takes on an earthy tint, and ascites grows due to portal hypertension. An expanded venous ring with outgoing vessels in the form of a “jellyfish head” appears around the navel.
In metabolic disorders characteristic of metabolic diseases, fermentopathy, along with hepatomegaly, the following is detected:
- damage to the kidneys and spleen (glycogenosis);
- copper deposits and a colored ring around the iris, hand tremors (Wilson-Konovalov disease);
- yellow-brown spots on the body and xanthelasmas on the eyelids, the connection of clinical manifestations with a period of fasting (pigmented hepatosis in Gilbert's syndrome);
- cough with hemoptysis (hemochromatosis).
In the patient, the signs of heart disease come first: shortness of breath, swelling in the legs, ascites, palpitations and arrhythmia, angina-type pain, cyanosis of the feet, hands, lips, and in children - the nasolabial triangle.
Stages
There are 4 stages of cirrhosis, the 3rd and 4th of which are usually burdened by ascites:
- Compensation stage. The tissue of the organ has undergone changes, fibrosis is localized mainly in the periphery, portal hypertension and ascites are absent.
- Subcompensation stage. Fibrosis spreads from the periphery to the center of the liver, and portal hypertension develops. Ascites is still insignificant, symptoms of the disease begin to appear.
- Stage of decompensation. The amount of fibrosis increases and reaches between half and two-thirds of the liver volume. Ascites is rapidly progressing.
- Terminal stage. New symptoms are added, the prognosis for survival is very low, the patient’s condition is serious, and the ascites is excessive.
Can hepatomegaly develop in only one lobe of the liver?
The liver consists of two lobes, each with its own innervation, blood supply, and bile ducts (central artery, vein, bile duct). Isolated hepatomegaly of the right lobe of the liver is observed more often than the left. Functionally, the right lobe is loaded more, performing 60% of the organ’s work, so any violations primarily affect it.
The left lobe is rarely affected; it is located closer to the pancreas; therefore, pancreatic disorders can cause an increase in the lobe
The examination usually reveals damage to the gallbladder and ducts, and the spleen.
With uneven enlargement of the organ, they speak of partial hepatomegaly. The lower edge of the liver rarely changes, so ultrasound is necessary for detection. A characteristic echo sign is a change in the homogeneity of the tissue structure. Usually found in tumors, cysts, and abscesses.
How is an enlarged liver and spleen combined?
An enlarged spleen (splenomegaly) may accompany hepatomegaly. It has been noticed that these two signs of pathology support each other. A simultaneous increase is expressed in hepatolienal syndrome. It is more typical for children, since it is aggravated by the anatomy and physiology of the growing organism.
It is provoked by hereditary diseases, infections, congenital anomalies. The syndrome is observed:
- for vascular diseases of the arteries and veins of the liver, spleen (vasculitis, thrombosis);
- chronic focal and diffuse liver pathology;
- hemochromatosis;
- liver amyloidosis;
- Gaucher's disease;
- hepatocerebral dystrophy.
Chronic parasitic and infectious diseases always, in addition to the liver, affect the spleen (intestinal tuberculosis, alveococcosis, malaria, infectious mononucleosis). Both organs are significantly enlarged with pathology of lymphoid tissue and blood (leukemia, lymphogranulomatosis, hemolytic anemia). Heart disease is less likely to promote spleen growth.
The main task of diagnosis is to identify the common cause that caused hepatomegaly and splenomegaly.
Organs have a pronounced functional connection
How does hepatomegaly occur in pregnant women?
Doctors note that liver problems during pregnancy occur in the third trimester. An enlarged uterus displaces the liver upward to the right. The movements of the diaphragm are limited, which makes it difficult to remove bile and fills the liver with blood.
Hormones influence the functioning of the liver, which is manifested by yellowish spots on a woman’s face and “stars” on the skin. An increase in fatty acids, cholesterol, and triglycerides is detected in the blood of a pregnant woman.
Pathological hepatomegaly can be caused by:
- toxicosis with prolonged vomiting, observed in 2% of pregnant women from the fourth to the tenth week, stops by the twentieth week, due to vomiting, dehydration, electrolyte disturbances can occur, and the woman’s weight decreases;
- intrahepatic stagnation of bile, found in every fifth pregnant woman, the cause is associated with hereditary predisposition.
Hepatomegaly can occur during pregnancy due to exacerbation of existing chronic diseases (heart decompensation, fatty hepatosis, diabetes mellitus, neoplasms, leukemia, hepatitis)
Treatment
It is possible to restore the normal size of the liver in a moderate form of the disease through diet therapy and taking hepatoprotective medications aimed at protecting the liver, as well as vitamin complexes and enzymes.
It is recommended to strictly follow the diet.
The following should be excluded from the diet:
- alcohol;
– fried, spicy, fatty, salty and spicy dishes;
– canned food and marinades;
– carbonated sweet drinks;
– dairy products with a high fat content – butter, cream, sour cream over 20%, ice cream, cheese.
You need to eat small portions 5 times a day. The main menu should include boiled vegetables and fruits, water porridge, lean meats and fish.
When does hepatomegaly occur in children?
Hepatomegaly in the fetus is manifested by an enlarged abdomen, which is detected on ultrasound during pregnancy. Already at this stage, doctors are trying to determine the cause; the course of pregnancy and the health of the unborn baby depend on it.
The most common are:
- intrauterine infection with viruses and bacteria (Toxoplasma, cytomegalovirus, Coxsackie, pathogens of chickenpox, rubella, syphilis, HIV), small hyperechoic inclusions are detected in the enlarged fetal liver;
- Rh conflict, when the mother’s blood is Rh negative, and the fetus accepts the father’s Rh;
- various tumor-like formations (hemangioma, hepatoblastoma, adenoma are detected in the fetus);
- increased hemolysis of red blood cells;
- heart defect with insufficiency;
- genetic manifestations of impaired metabolism;
- congenital anomalies.
Isolated fetal hepatomegaly rarely develops; more often it is accompanied by an enlarged spleen and other defects. The most successful period for detection is the II–III trimesters. Through a full examination, it is necessary to exclude Down syndrome.
In newborns and infants up to one year, a slight enlargement of the liver is considered normal. If, upon palpation, the lower edge protrudes from the hypochondrium by more than 2 cm, the condition is pathological and needs to be clarified.
Hepatomegaly syndrome can be accompanied by poor diet, complicate vaccination, and indicate autoimmune processes in the child’s body
The most common pathological causes are:
- infectious diseases, any viral infections;
- heart defects with right ventricular failure - pay attention to the baby’s heavy breathing, cyanosis of the face and limbs, tachycardia;
- diseases of the respiratory system - the child has severe shortness of breath, wheezing in the lungs;
- bile duct cysts with blockage of the bile ducts, inflammation - accompanied by high temperature, pain on palpation in the hypochondrium on the right;
- Debre's syndrome, Gierke's disease - accumulation of glycogen in the liver tissue contributes to the early development of fatty hepatosis, accompanied by convulsions, increased lactic acid content in the blood, acetoacetic acid is released in the urine;
- impaired lipid metabolism - expressed by constant diarrhea, vomiting, yellow spots on the skin;
- Mauriac's syndrome - complicates the course of diabetes, fat accumulates in the child's liver;
- tumors (hepatoblastoma, hemangioma) benign and malignant are rare.
A small child with hepatomegaly exhibits all the classic symptoms. They are difficult to tolerate. As the abdomen enlarges, the umbilical ring does not heal, and a hernial orifice is formed, through which the navel and intestinal loops protrude. Jaundice persists.
HIV-infected newborns sometimes differ from healthy children only in hepatomegaly. From an early age, frequent viral infections of the respiratory tract, mumps, dermatitis occur, lymph nodes become enlarged, and fungi affect the oral cavity. Any infection can lead to sepsis, meningitis, and anemia.
Echinococcosis affects older children. The main reason is contact with dogs. At 5–7 years of age, a moderate enlargement of the liver is observed, which is considered a physiological phenomenon and does not require intervention.
In older groups, the cause may be hepatitis (viral, toxic, drug), complications after congenital infection with herpes viruses, rubella, parasitic diseases, impaired bile outflow, biliary cirrhosis.
There may be metabolic changes in diabetes mellitus, Wilson-Konovalov disease, porphyria, liver damage caused by hemolysis, lymphoma, leukemia, tumors such as hemangioma, carcinoma with metastases.
In the presence of respiratory diseases, false hepatomegaly should be distinguished; it appears due to the pushing of the liver from under the ribs by increased airiness of the lungs
How is diagnosis carried out?
The above reasons for the increase in liver size indicate the difficulty of finding the underlying disease and the importance of differential diagnosis. This means that, in addition to identifying hepatomegaly, all possible types of research are used: blood and urine tests, general tests, bilirubin, sugar, protein, liver function testing using biochemical tests for basic enzymes.
Monitoring of the blood coagulation system and enzyme immunoassay are prescribed for viral and bacterial infections. The doctor determines the estimated growth of the organ using percussion and palpation methods.
Hardware methods are much more accurate and objective: ultrasound, computed tomography and magnetic resonance imaging, radiography is less informative, scanning with preliminary administration of hepatotropic radioactive substances gives a complete picture of cell damage, and the proportion of remaining undamaged tissue can be calculated.
Modern equipment makes it possible to detect not only changes in size, but also to accurately contrast the boundaries, tissue structure, and the nature of the changes (focal, diffuse). Morphological changes can be definitively judged by examining a biopsy.
The most accessible method for the population is ultrasound; it is based on the principle of recording the reflection of a wave from a dense organ.
Ultrasound allows you to compare the structure of the liver in all zones, identify denser foci and the size of the lobes. Echoscopic observation can be thought of as a visual examination on a screen without recording. It is more important when monitoring a contracting organ (heart). The liver is examined using echographic criteria, and images are printed in different projections.