But let's return to the characteristics and symptoms of the pathology.
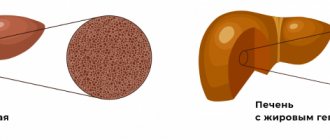
Steatosis is a disease caused by a disorder of phospholipid metabolism, in which both intracellular and extracellular deposition of fat droplets occurs in the liver parenchyma. Normally, the human liver contains 5-7% fat. If this percentage reaches 10 or higher (in the most severe cases, this percentage rises to 50 - that is, half of the liver parenchyma is fat), this is a good reason to diagnose fatty infiltration. In this article, we will discuss hepatic steatosis, symptoms and treatment of this disease.
Symptoms
In order to understand what hepatic steatosis is, it is necessary to know not only the pathogenesis, but also the symptoms of the disease. Steatosis of the liver and pancreas is more common in women. Usually the disease develops asymptomatically over a fairly long period, so it most often manifests itself in people over 40 years of age. Symptoms of the disease are in many ways similar to those of hepatitis:
- enlarged liver - its edges, protruding 3-4 centimeters from under the costal arch, can be felt during palpation;
- decreased performance, fatigue, irritability, apathy, poor sleep, absent-mindedness;
- nagging pain in the right hypochondrium, which is explained by an enlarged liver stretching the fibrous capsule;
- unstable stool, vomiting;
- slight icterus of the sclera of the eyes (the skin usually retains its normal color);
- unpleasant skin odor and bad breath;
- rashes, itching of the skin.
Establishing diagnosis
Diagnosis of pancreatic steatosis is carried out on the basis of patient complaints, examination and computer diagnostics - ultrasound, MRI or CT. In some cases, a biopsy is done.
If during the examination a person was diagnosed with steatosis, the condition of the liver is also checked, since this organ is most often affected during the development of this disease. And only after this the doctor assesses the general condition of the patient, the functioning of the gland and other organs, and also determines further treatment tactics.
Etiology
We have already received a general idea of what diffuse hepatic steatosis is, and now it’s time to move on to the details. The cause of disturbances in phospholipid metabolism and the resulting increase in the level of free fatty acids in the liver parenchyma is usually an incorrect lifestyle and diet in particular. The modern lifestyle of most clerks predisposes them to spend a lot of time sitting (both in front of the monitor and behind the wheel), eat poorly (fortunately, supermarkets have a large selection of all sorts of unhealthy goodies), and also periodically drink alcohol.
We can say that steatosis is a disease of lazy people.
Obesity greatly contributes to the accumulation of lipids in liver tissue. Add to this the bad environment, and we get a portrait of a typical patient with fatty liver: not too young, not too slim and predisposed to alcohol. The list of predisposing factors looks something like this:
drug addiction (morphine derivatives, methamphetamine, any potent psychotropic substances).- alcohol abuse;
- pharmacological drugs that have hepatotoxic side effects (anti-inflammatory, hormonal, painkillers, antibiotics and antidepressants);
- congenital metabolic disorder (malabsorption syndrome);
- impaired absorption of protein and vitamins due to previous operations (for example, resection of the small intestine);
- chronic diseases of the gastrointestinal tract, in which the absorption of nutrients worsens (most often colitis, pancreatitis);
- insufficient amount of protein in the diet (protein contributes to the normal absorption of fats);
- chronic foci of infection in the body, severe intestinal dysbiosis, accompanied by general intoxication of the body;
- diabetes;
- general obesity;
Particular attention should be paid to malnutrition associated with insufficient protein in the diet.
At first glance, the issue is not as acute as, for example, alcohol or drug abuse. However, this is precisely why nutritional issues are often not given enough attention, which provokes fatty liver degeneration. Vegetarians (and especially vegans - the most radical representatives of the movement) deprive themselves of animal protein, which helps the normal absorption of fat. The lack of animal protein food can somehow be compensated for by cottage cheese, milk and cheese, but vegans do not accept even such a diet, so they chronically do not receive enough amino acids. At the same time, as compensation, they often indulge in sweet dishes, which also has a bad effect on the condition of the liver.
Alcohol occupies a special niche among the factors contributing to the development of the disease. Most cases of fatty liver degeneration are precisely the result of abuse of ethanol derivatives. Alcoholic steatosis of the liver often ends in cirrhosis - irreversible changes in liver tissue.
That is why even a special abbreviation NAFLD arose - liver steatosis not caused by alcohol consumption (literally: Non-alcoholic Fatty Liver Disease).
Symptom complex
The disease can be asymptomatic for a long time, especially with focal damage to the organ. As for diffuse changes in the liver such as steatosis, they are characterized by the appearance of nonspecific signs:
- a person feels constant weakness, gets tired quickly during physical and mental stress;
- Nausea occurs mainly after eating. Vomiting is rare and may be mixed with bile;
- changes in the psycho-emotional state are manifested by irritability and apathy;
- Dyspeptic disorders include belching, bitterness in the mouth, heaviness in the stomach and intestinal dysfunction, which is caused by impaired digestion of food;
- liver pain. Its character and intensity can be different, ranging from bursting, aching and ending with severe colic. Note that the parenchyma does not have nerve endings, as a result of which it is not capable of causing pain. However, with inflammation and swelling, it increases in volume, thereby stretching the fibrous capsule of the organ. It is after irritation of its receptors that an unpleasant symptom appears. Pain can also spread to the epigastric (supragastric) zone, sometimes to the lower back and abdomen;
- Jaundice develops with cholestasis, that is, stagnation of bile. When its production and movement through the excretory ducts are disrupted, large quantities of bilirubin enter the bloodstream, which is accompanied by yellowness of the skin and mucous membranes. It is also possible that itching sensations and changes in the color of stool may occur;
- loss of appetite.
Against the background of liver steatosis, there is a decrease in the body’s immune defense, which makes a person more susceptible to infection. He often suffers from acute respiratory viral infections and suffers from exacerbations of chronic diseases.
A severe complication of the disease is cirrhosis. It develops due to the replacement of dead hepatocytes with connective fibers. Thus, the non-functioning area of the liver gradually increases, thereby aggravating the organ failure.
Pathogenesis
The accumulation of fat droplets in liver tissue can occur due to a violation of the natural oxidation of free fatty acids in liver mitochondria, as well as due to their increased formation and accelerated delivery to hepatocytes. Due to weakened production of lipoproteins, the removal of triglycerides from the liver worsens. The accumulation of fats in the liver parenchyma can provoke the development of inflammatory and even necrotic processes. A direct relationship between these two processes has not yet been accurately established, but it is generally accepted that the development of inflammation and tissue necrosis can be caused by the intake of hepatotoxic substances that promote the release of free radicals and the onset of oxidative processes. In addition, the production of endotoxins (toxic substances produced inside the body), which usually occurs when there is pathological growth of bacteria in the intestines or the presence of a focus of infection in other organs and tissues, can also become such an impetus.
The development of fatty infiltration can be both diffuse and focal in nature. Diffuse hepatic steatosis is characterized by uniform deposition of fats in the liver parenchyma. It is not difficult to guess that the focal form is characterized by focal deposits of fat.
Who is susceptible to the disease
In most cases, steatosis develops in the presence of a combination of the following two factors:
- improper lifestyle;
- development within the body of any of the above concomitant diseases.
Unfortunately, not only is steatosis itself a very difficult disease, it also provokes the very rapid development of a pathology such as cirrhosis of the liver. Together, these two pathologies can kill even an otherwise healthy person.
The age category most susceptible to the development of steatosis is represented by citizens of both sexes:
- women aged 60 and older;
- men aged 50 and older.
The fact is that citizens who have lived to this age are usually no longer able to give up bad habits, for example, smoking or drinking, while their immunity has long been weakened and cannot resist incoming toxins. The same applies to junk food, the consumption of which at this age is as dangerous as smoking or drinking alcohol.
Steatosis in the International Classification of Diseases
According to the ICD-10 classification, hepatic steatosis does not have a single code. The digital values of the code change, since liver steatosis, the symptoms of which vary depending on the forms of the disease, can give a different clinical picture. The following code options are allowed:
- K 73.0 – chronic hepatitis;
- K 73.9 – chronic cryptogenic hepatitis (of unclear etiology);
- K 76.0 – fatty liver, not mentioned in other sections;
- Changes in the liver like cirrhosis.
As can be seen from the list, code 76.0 is closest to steatosis, but it does not always fully reflect the nature of the pathological changes occurring in the liver parenchyma, since fatty infiltration can be combined with both the proliferation of connective tissue and inflammatory and necrotic phenomena.
How to diagnose the disease
Like other dangerous diseases, steatosis cannot be diagnosed solely during an initial examination based on the patient’s testimony, since, unfortunately, they are not enough.
The main diagnostic activities will be carried out through the following categories of studies.
Table 1. Tests performed to diagnose steatosis
| Instrumental diagnostics | Laboratory research |
Instrumental diagnostics is a method that involves examining a patient using specialized medical equipment. So, they usually do:
| Further diagnostic methods are based on the study of biological fluids of the human body in a laboratory setting. So, for inspection they take:
The purpose of the examination is to determine the level of specific substances in the body, for example, alpha-amylase. |
Additionally, when diagnosing “steatosis”, the functioning of the liver is checked, since it is this organ that can be the first to be affected by the disease being sought, triggering the process of fatty infiltration of its cells.
Diagnostics
Due to the absence of clear symptoms, often accumulated fat in hepatocytes (liver cells) is detected by chance (for example, during a routine examination of a person or during diagnosis for another disease). When a patient contacts a specialist with complaints of dyspeptic disorders and chronic fatigue, the doctor first examines the anamnestic information, concomitant diseases, as well as the peculiarities of the appearance of clinical signs of steatohepatosis.
He focuses on alcoholism, the presence of metabolic diseases and endocrine pathology. During the physical examination, the skin, mucous membranes and palpation (palpation) of the abdomen are assessed.
For further examination, laboratory tests and instrumental methods are prescribed.
Laboratory diagnostics
To study the functional capacity of the liver and other internal organs, the doctor prescribes biochemistry. It includes many indicators, but more attention is paid to transaminases. They are intracellular enzymes that, after the destruction of hepatocytes, are released. The degree of their increase characterizes the severity of the pathological process in the liver.
We are talking about alanine aminotransferase and aspartate aminotransferase. In addition, the level of alkaline phosphatase, bilirubin and protein is examined. Changes in steatosis concern the prothrombin index, which gradually decreases, as well as cholesterol and lipoproteins, which increase their content in the blood.
The listed indicators refer to indirect markers of the disease. As for the more accurate ones, they provide information about the quantitative composition of fibrous fibers.
Several biomarkers have been developed for diagnostic purposes. Fibrotest includes:
- haptoglobin;
- alpha-2 macroglobulin;
- gamma-glutamyl transpeptidase;
- total bilirubin volume;
- apolipoprotein A1.
Unlike the marker described above, Actitest additionally includes ALT. The accuracy of the technique at the initial stage of fibrosis is about 70%, while with pronounced changes in the liver it reaches 96%.
The fibrometer provides information on the quantitative composition of platelets, gamma-GT, transaminases, urea, as well as prothrombin and alpha-2 macroglobulin. The accuracy of the technique is approximately 87%.
The complex of laboratory tests may include determining the level of the gland, searching for markers for viral hepatitis, as well as antibodies (antinuclear and anti-smooth muscle).
Instrumental methods
The diagnostic complex also includes instrumental methods necessary for visualization and examination of the liver:
- Ultrasound is an accessible and informative way to examine internal organs. It allows you to evaluate the volume, structure, boundaries and blood flow, as well as detect additional formations. At the same time, ultrasound does not make it possible to examine the density and elasticity of tissue, which requires more accurate diagnosis;
fibroscanning is considered a direct method, during which low-frequency pulses are generated, which allows for targeted examination of the structure of the liver. Diagnosis is carried out once every 3-6 months (with 1-2 degrees of steatosis), and also every 4-8 weeks - with pronounced changes;- biopsy is an invasive test and therefore cannot be repeated frequently. Under anesthesia, the doctor collects material (a piece of liver tissue), and then sends it for histological analysis. The quality of diagnosis depends on the qualifications of the specialist and the area of the organ that was removed. If the liver structure changes unevenly, material may be taken from a less affected area, which will lead to incorrect determination of the stage of steatosis.
The first degree of the disease is characterized by the accumulation of fat in hepatocytes without changing their structure. Already in the second case, dystrophy and the formation of multiple cystic formations are observed, around which cell compaction occurs. The third degree is manifested by areas of connective tissue that completely disrupt the structure of the liver, which leads to its dysfunction.
3. Symptoms of pancreatic steatosis and diagnosis
Signs of the onset of the steatopancreatic process can be very blurred and be expressed by irregular disorders of the digestive process. At some point, for no apparent reason, a person experiences previously unobserved phenomena:
- heartburn;
- nausea;
- flatulence;
- allergic reactions;
- diarrhea;
- pain in the left hypochondrium after eating.
Studies already at this stage make it possible to identify signs of tissue changes and functional insufficiency of the pancreas: the presence of fatty layers, metabolic syndrome, hyperamylasemia, decreased densitometric parameters.
Diagnosis of suspected steatopancreatitis begins with collecting an anamnesis. The patient must describe his complaints in detail, preferably indicating the frequency, regularity and severity of certain clinical manifestations of the disease. It is advisable to describe the nature of the pain, the consistency of the stool, whether vomiting brings relief in the presence of nausea, how the symptoms are related to periods of eating and fasting. Laboratory tests can clarify the suspected diagnosis. These may include:
- examination of stool for the presence of enzymes;
- urine and serum analysis;
- study of the composition of pancreatic juice.
Instrumental diagnostic methods (ultrasound of the pancreas, laparoscopy and biopsy) reveal structural changes in tissue, the volume and location of accumulated fat.
About our clinic Chistye Prudy metro station Medintercom page!
Treatment of steatosis
It is necessary to treat the disease after diagnosis and taking into account the patient’s concomitant pathology. To date, there are no specific treatment regimens for steatosis. The treatment process often includes several areas:
- dietary nutrition according to table No. 5;
- weight correction. Given the presence of obesity in patients with hepatic steatosis, gradual weight loss is required by following the recommendations of a nutritionist. Complete refusal of food or self-limitation can lead to a sharp deterioration in the patient’s general condition;
- correction of hyperglycemia, -lipidemia and -cholesterolemia using diet and medications;
- giving up alcohol;
- discontinuation of hepatotoxic medications.
Among the effective drugs it is worth highlighting:
- Ursosan is based on ursodeoxycholic acid, which is a component of bile. It has a protective effect on hepatocytes, reduces cholesterol production and reduces its absorption in the intestine. The medicine also prevents stagnation, normalizing bile flow. It increases the activity of pancreatic enzymes and slightly reduces blood glucose;
- Heptral - has amino acids. It has antidepressant, detoxification and hepatoprotective effects;
- Phosphogliv is a medicine with essential phospholipids that are embedded in the cell membrane and prevent the destruction of hepatocytes;
- Hepa-Merz is a protective and detoxifying agent that contains amino acids (aspartate, ornithine);
- Metformin is an antidiabetic medication that improves glucose absorption. It belongs to the group of biguanides. Taking the medicine is accompanied by a decrease in thyroid-stimulating hormone and cholesterol, which is necessary to prevent vascular damage. Its main effect is to block glucose synthesis in the liver and increase the sensitivity of insulin receptors;
- Atorvastatin is prescribed to lower cholesterol.
How to eat properly?
Diet for pancreatic steatosis is the main component of treatment. The diet should be low in calories, contain the physiological norm of protein with a sharp limitation of fats and carbohydrates. It is also necessary to take into account the fact that meals should be fractional - you need to eat 5-6 times a day, but in small portions. When following a diet, the patient should eat boiled or steamed food. The consumption of fried, fatty, salty, smoked and spicy foods is strictly prohibited. Sour and canned foods are also prohibited. It is necessary to stop drinking alcohol and smoking.
It is necessary to remove sweets and baked goods from the diet. It is not recommended to consume dairy products with high fat content. Preference should be given to light soups with cereals and vegetables. To prepare porridges, it is better to use rice, rolled oats and buckwheat. Vegetables you can eat: potatoes, zucchini, eggplant, pumpkin, radish, cucumbers, cauliflower, tomatoes. A specially designed nutritional system must be followed at all times. Strict adherence to a therapeutic diet will help prevent complications and progression of the disease.
Why is fatty liver disease dangerous?
Without treatment, liver steatosis threatens to develop severe complications. They are presented:
- fibrosis. As the cells die, they are gradually replaced by connective fibers, which is accompanied by scarring of the organ. Against this background, the functioning of the liver rapidly deteriorates;
- disruption of the production and movement of bile through the excretory ducts, as a result of which cholestasis develops and the digestion process is disrupted;
- steatohepatitis, which is characterized by inflammation of the liver tissue against the background of its fatty degeneration.
Separately, we should highlight cirrhosis, which is dangerous due to its manifestations. Against the background of protein deficiency, there is a deficiency of coagulation factors, which is fraught with massive bleeding. In addition, esophageal veins undergo varicose changes. They become crimped and their walls become thinner. The patient begins to experience severe swelling of the extremities. Fluid accumulates not only in tissues, but also in cavities (pleural, abdominal), which is accompanied by symptoms characteristic of pleurisy and ascites.
Provided proper treatment and compliance with all medical recommendations, it is possible to slow down the progression of the disease and significantly improve a person’s general condition.
Let's sum it up
A disease such as steatosis, although not considered fatal, is still very dangerous, since as a result of its development, the human body loses a significant part of the “power” of each organ. In other words, when beneficial cells are replaced by adipose tissue, the organ ceases to be able to fully carry out the functions assigned to it and provide the body with everything necessary.
To avoid the development of steatosis, it is best to follow preventive measures such as:
- proper nutrition;
- regular physical activity;
- healthy lifestyle.
Doctors agree that lipomatosis is an “eternal” disease, since it is impossible to talk about complete recovery. Dead cells cannot be regenerated. Therefore, treatment is aimed at trying to stop further replacement. This will be facilitated by proper nutrition and an active lifestyle.
Chronic alcoholic hepatitis: signs, symptoms, diagnosis, treatment
Chronic alcoholic hepatitis is accompanied by more pronounced clinical and biochemical manifestations than steatosis and liver fibrosis. The pathological process occurs with the development of small focal necrosis of hepatocytes and is accompanied by a fibrosing and inflammatory reaction. The inflammatory infiltrate consists predominantly of polymorphonuclear leukocytes. The clinical picture of chronic alcoholic hepatitis is characterized by pain in the right hypochondrium and dyspeptic disorders. Changes in laboratory parameters are more pronounced. The activity of aminotransferases increases, the level of gamma-glutamyl transpeptidase increases 3 or more times, and the content of immunoglobulin A in the blood increases. Differential diagnostic criteria for chronic alcoholic active hepatitis and hepatitis of other etiologies are anamnesis data, the absence of markers of a current viral infection in the blood (hepatitis A, B, C, D, F), and the detection of alcoholic hyaline in biopsies. With continued alcohol intake, chronic alcoholic hepatitis over 3–5 years leads to the development of alcoholic cirrhosis of the liver.
Acute alcoholic hepatitis: signs, symptoms, diagnosis, treatment
Acute alcoholic hepatitis occurs against the background of intense and prolonged drinking bouts and is accompanied by widespread necrotic lesions of the liver parenchyma with a pronounced inflammatory and significant fibrosing reaction. Necrosis is localized in the center of the lobules and can extend to the portal tracts (bridging necrosis) or affect the entire parenchyma of several adjacent lobules (multilobular necrosis). Acute alcoholic hepatitis is usually superimposed on previous steatosis, liver fibrosis or chronic alcoholic hepatitis. Leads to a pronounced deterioration of the clinical picture and significantly accelerates the formation of liver cirrhosis. Sometimes acute alcoholic hepatitis occurs with cholestasis. The disease resembles extrahepatic obstruction of the biliary system (abdominal pain, cholestasis, characteristic clinical and laboratory signs are noted). Patients are often admitted to surgical hospitals, where they sometimes undergo unnecessary surgery. It can be severe, with jaundice, signs of portal hypertension, signs of hepatic cellular failure and even death. Most often, a moderate form is observed, in some cases without jaundice and severe symptoms. Moderate forms of acute alcoholic hepatitis occur against the background of recent intense binge drinking, when anorexia, increasing weakness, nausea, vomiting, pain in the upper abdomen, diarrhea, rapid weight loss, moderate jaundice, and fever (hyperthermia) of subfebrile or febrile type appear. Palpation reveals an enlarged, dense, painful liver. The activity of aminotransferases is noticeably increased, the activity of gamma-glutamyl transpeptidase exceeds the upper limits of normal by 40 - 50 times, the activity of alkaline phosphatase is increased by more than 2 - 3 times. In a general blood test, neutrophilic leukocytosis can be observed up to 10 - 25 x 10 to 9 degrees / l with a band shift (up to 20 - 30), an increase in erythrocyte sedimentation rate (ESR) up to 30 - 50 mm/h.
Alcoholic cirrhosis of the liver: signs, symptoms, diagnosis, treatment
Alcoholic cirrhosis of the liver has a direct relationship with the amount of alcohol consumed daily (more than 80 grams per day) or the duration of alcoholism (more than 4–6 years). It develops in 10–30% of patients with chronic alcoholism. Genetic predisposition and poor nutrition are contributing factors. In women, alcoholic cirrhosis develops with less daily alcohol intake and duration of alcoholism.
What are the symptoms of liver cirrhosis? The following clinical signs (symptoms) of alcoholic cirrhosis of the liver . 1. Hepatomegaly (liver enlargement) with or without jaundice.
2. Splenomegaly (enlarged spleen).
3. Portal hypertension with dilated veins of the esophagus and often ascites.
4. Anorexia.
5. Enlargement of the parotid salivary glands.
6. Testicular atrophy in men.
7. Erectile dysfunction (impotence), erectile dysfunction.
8. Decreased libido (decreased sex drive).
9. Gynecomastia (enlargement of mammary and mammary glands in men).
10. Dupuytren's contracture.
11. Myopathy (muscle pain, atrophy, weakness).
12. Polyneuropathy.
13. Trembling of hands, eyelids, tongue.
14. Palmar erythema (redness of the palms).
15. Spider veins.
16. Puffy face with swollen eyelids and reddened skin.
17. Abdominal pain (stomach pain).
18. Erosion and peptic ulcers of the stomach and duodenum.
19. Gallstones.
20. Chronic pancreatitis.
Azotemia, hyperuricemia, signs of anemia, thrombocythemia, leukopenia (decreased number of white blood cells), coagulopathy are often detected. The prognosis is determined by the cessation or continuation of alcoholism.