Home > Articles > Liver restoration after poisoning
It is customary to treat poisoning until symptoms such as nausea, diarrhea and dizziness disappear. In rare cases, patients recall the subsequent normalization of water and electrolyte balance and cleansing of the liver, but it is the liver that receives the most damage, since it is the body’s filter, ensuring the neutralization of toxins and poisons that have entered it. Therefore, the biggest problem in the treatment of poisoning remains liver intoxication. Symptoms, treatment, and prevention of liver poisoning are not generally known, and patients often resort to folk remedies for cleansing, only worsening their condition.
Content:
- Etiology.
- Pathogenetic mechanisms of liver intoxication.
- Clinical picture of alcoholic liver intoxication: 3.1. Steatosis. 3.2. Alcoholic hepatitis. 3.3. Cirrhosis.
- Diagnostics.
- Principles of treatment: 5.1. Nutrition correction. 5.2. Drug treatment.
Alcoholic liver intoxication refers to the sequential development or combination of several diseases: steatosis (fatty degeneration), hepatitis and cirrhosis. In this case, the pathology can be asymptomatic (or with a “blurred”, non-specific clinical picture) until the development of irreversible changes. According to WHO, alcoholic liver poisoning is the most common disease in hepatology.
Effects of alcohol on the liver
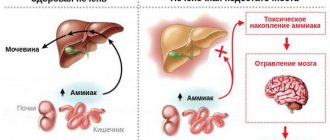
After entering the stomach, ethanol enters the bloodstream, then into the hepatobiliary system, where breakdown and neutralization occurs.
For processing, a lot of enzymes are synthesized that convert alcohol into simple compounds - water and carbon dioxide. The intermediate breakdown product is acetaldehyde, a toxic substance. The liver of a healthy person quickly removes metabolic products. The worn-out organ of a patient with alcoholism cannot cope with the systematic use of alcohol, slowing down the removal of metabolites and retaining some of the toxins in the tissues. The consequence is the onset of acetaldehyde intoxication, requiring the use of infusions of detoxifying drugs. Alcohol liver poisoning can occur not only in hardened alcoholics. Any person who drinks alcohol in large quantities is susceptible to toxic effects. The risk group includes:
- teenagers and young people under 21 years of age;
- women, their gland is most vulnerable to alcohol;
- having chronic cardiovascular pathologies, diseases of the thyroid gland, gastrointestinal tract, autoimmune diseases, hepatitis in the anamnesis;
- people with excess body weight, as well as those suffering from diabetes;
- patients taking medications according to indications - anti-inflammatory drugs, painkillers, hormones, antidiabetic drugs.
According to statistics, more than 40% of people suffer from intoxication after drinking alcohol. 78% of addicts develop cirrhosis, 14% develop hepatocellular carcinoma or liver cancer.
Etiology
The most obvious reason for the development is long-term abuse of alcoholic beverages. In this case, not only the amount of alcohol matters, but also the frequency of drinking episodes and the specific type of strong drinks. For most people, the critical dose of ethanol is 80–160 g per day over 10–20 years of regular drinking.
But in women, the disease develops when drinking much smaller doses of alcohol (20–40 g per day) and over a shorter period. This is explained by the smaller number of enzymes involved in the breakdown of ethanol. And if therapy is started too late, in 50% of women the pathology progresses to hepatocellular carcinoma, even if they get rid of addiction.
According to experts, one-time alcoholic excesses (even with significant alcohol abuse) are safer, since a rare intake of alcohol gives the liver the opportunity to “recover”, which cannot be said about daily drunkenness.
In addition, the risk of alcoholic liver toxicosis is increased if:
- genetic characteristics due to which the mechanisms for the production of enzymes that affect the metabolism of alcohol are disrupted;
- being overweight, which provokes the accumulation of visceral fat;
- concomitant viral and infectious liver diseases;
- taking hepatotropic medications (antifungals, antibiotics, immunosuppressants), antiulcer medications that reduce the activity of alcohol dehydrogenase;
- autoimmune diseases.
Restoring the liver after poisoning: basic recommendations
How to restore the liver after poisoning? One of the main methods is a special diet. The method is simple, effective and allows you to really cope with most of the consequences of poisoning. It is necessary to exclude from the menu during the recovery period of liver cells:
- excessively fatty foods;
- spicy foods and seasonings;
- pickles and marinades;
- smoked meats, especially those prepared using “liquid smoke”;
- canned food, even homemade;
- mayonnaise, mustard, ketchup;
- It is better to replace fried foods with baked or steamed ones.
In this case, you should include in your daily diet foods that are beneficial for the liver:
- rabbit meat, turkey;
- butter and vegetable oil (in moderation);
- dairy products;
- cereals;
- peas, lentils, beans, chickpeas;
- fruits vegetables;
- low-fat fish.
Among the tips on how to treat liver intoxication, if the risk of re-poisoning is high (workers in hazardous industries, residents of environmentally unfavorable areas, people with chronic liver diseases), there is an important point: daily consumption of milk and dairy products. Even following only this rule will reduce the risks of re-intoxication. It is also advisable to limit any other sources of toxic substances - stop smoking, alcohol, spend more time in the fresh air, even if this means traveling several blocks. You should avoid fast food, as well as a variety of semi-finished products.
In addition to proper nutrition, a course of hepatoprotectors is of great importance. These drugs, the task of which is to normalize the activity of the liver, may be different in their composition, origin, formula of the active substance, but they are all united by a beneficial effect on liver tissue. For example, Legalon is a hepatoprotector based on silymarin from the fruits of milk thistle, has an antioxidant effect, helps restore liver cells, and normalize the course of biochemical processes in them. The unique purification system for silymarin allows us to achieve maximum bioavailability of this substance, which distinguishes this drug from other plant hepatoprotectors. It can be taken by children from 12 years of age.
Pathogenetic mechanisms of liver intoxication
The main metabolite of ethyl alcohol, acetaldehyde itself has a damaging effect on hepatocytes. This connection calls:
- damage to cell membranes and, accordingly, their necrosis;
- increased synthesis of triglycerides and their deposition in hepatocytes;
- impaired synthesis of serum albumin (this protein determines the colloid osmotic pressure of the blood);
- violation of the filtration function of the liver;
- stimulation of lipid peroxidation processes.
In place of damaged hepatocytes, foci of connective tissue form. This leads to a deterioration in the blood supply to liver cells, progression of the inflammatory reaction, and activation of carcinogenesis processes. It has been established that one of the most dangerous forms of cancer, hepatocellular carcinoma, in the vast majority of cases develops against the background of progressive cirrhosis.
Common Consequences
Regular consumption of alcohol-containing drinks, regardless of strength, harms the entire body. The worst consequence is chronic poisoning. Common complications of alcohol consumption.
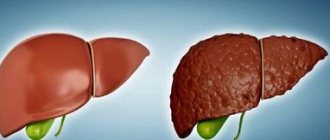
- Steatosis or fatty degeneration
is the first phase of the manifestation of structural changes, diagnosed in 90% of alcoholics. It is curable; if you abstain from alcohol, the functions of the organ are fully restored. - Hepatosis
is a consequence of constant exposure to ethanol leading to disruption of fat metabolism, which contributes to the occurrence of degenerative changes. This causes tissue degeneration - fat particles displace the nuclei of healthy cells, gradually replacing them with connective fibrous tissue. The disease is diagnosed in 95% of people prone to excessive drinking. - Alcoholic hepatitis develops against the background of hepatosis
- a combination of degenerative and inflammatory processes under the influence of large doses of alcohol. Diagnosed in every fifth case. Without timely medical intervention, the disease progresses to cirrhosis. - Cirrhosis - destruction of hepatocytes,
cessation of the detoxification process, toxins circulate freely through the blood, causing the development of hepatic encephalopathy, affecting brain cells. It occurs quickly; several years pass from the first symptoms of deficiency to the terminal stage. At the last stage, more than half of patients die within six months.
Clinical picture of alcoholic liver intoxication
Symptoms of the disease depend on its stage and specific form.
Steatosis
The most common (diagnosed in almost 90% of people who abuse alcohol) manifestation of the pathology. The signs of fatty degeneration are nonspecific, so most patients simply do not pay attention to them. Note:
- decreased appetite;
- discomfort (minor pain, heaviness) in the area of the right hypochondrium;
- flatulence;
- bowel disorders (mainly diarrhea);
- fatigue, general malaise;
- deterioration of health after overeating, eating fatty, fried foods.
Jaundice and other symptoms characteristic of liver damage appear extremely rarely (less than 10% of patients with diagnosed steatosis).
Alcoholic hepatitis
It can occur in acute or chronic form. Acute is the most severe type of alcoholic liver intoxication, usually develops after a prolonged alcoholic excess against the background of steatosis, compensated cirrhosis, fibrosis.
There are several types of acute alcoholic hepatitis:
- Icteric. Accompanied by nausea, lack of appetite, vomiting, severe digestive disorders. Characterized by a jaundiced coloration of the skin and whites of the eyes against the background of severe fever and arrhythmia. The somatic symptoms of alcoholism intensify (tremor, polyneuropathy, excessive excitement or, conversely, lethargy).
- Cholestatic. Severe jaundice with severe skin itching, fever, and a sharp decrease in body weight is typical. Due to spasm of the biliary tract, changes in the concentration of bilirubin, urine becomes dark brown, and feces become discolored.
- Fulminant. The most unfavorable option occurs with massive necrosis of hepatocytes. Manifests with fever, loss of appetite. The pathology progresses very quickly. Sometimes, even with timely medical care, hemorrhagic syndrome, encephalopathy, acute renal failure, cerebral edema and death cannot be ruled out.
The chronic form is characterized by a less pronounced clinical picture. Typical:
- various digestive disorders;
- moderate pain in the abdominal area;
- periodically occurring jaundice (one of the predictors of an unfavorable prognosis for the development of the disease);
- weakness, exercise intolerance, drowsiness.
Hepatitis is dangerous due to complications, since due to a violation of the filtration function of the liver, general immunity is reduced, and accordingly, the risk of infection with tuberculosis, HIV, etc. increases. Cardiomyopathies, pancreatitis, and pyelonephritis are often diagnosed against the background of damage to the hepatobiliary system.
Cirrhosis
In terms of symptoms, the initial stage of cirrhosis differs little from chronic hepatitis. But the jaundice is already becoming permanent, the patient is exhausted due to anorexia and sudden weight loss. As the disease progresses, the following signs appear:
- characteristic vascular network on the skin of the nose;
- spider veins on the body;
- periodic episodes of fever, chills;
- recurrent nosebleeds.
Safety precautions: what not to do
When restoring the liver after poisoning, it is worth adhering to the principle of “do no harm,” especially when it comes to combining the methods of classical, traditional and oriental medicine. It is a well-known fact: many drugs, harmless in themselves, react with medications and form dangerous combinations. That is why, when treating at home, it is necessary to first talk with your doctor and clarify which folk remedies are safe and which are best avoided. If the doctor prescribes a detailed treatment regimen using both traditional and classical medicines, it is necessary to follow it very strictly, maintaining time intervals. Only then will restoration of the liver after poisoning by drugs, fungi or bacteria be successful.
Before you start taking choleretic preparations and herbal infusions for the liver, you need to remember that:
- Any deterioration in well-being cannot be ignored. Sudden dizziness, trembling in the hands or knees require consultation with a doctor;
- You cannot refuse hospitalization if emergency doctors insist. The risk of dying if you refuse increases many times over;
- You cannot drink alcohol while adhering to a strict diet;
- we must not forget about other chronic diseases, including those requiring a certain type of nutrition;
- You cannot combine several treatment methods on your own.
How, then, to treat liver intoxication at home? With maximum self-care. It is mandatory:
- sleep well;
- eat regularly;
- provide yourself with some physical activity;
- avoid stress;
- try to do things that bring you pleasure every day;
- take hepatoprotectors;
- visit your doctor periodically.
Since liver cells are able to effectively regenerate, providing conditions for the body to heal independently is a top priority. Good nutrition, healthy sleep, and hepatoprotective drugs stimulate natural processes, helping to restore the liver after serious poisoning.
Diagnostics
In addition to standard general clinical tests, the following are required:
- blood biochemistry;
- liver tests;
- coagulogram;
- analysis to determine the level of electrolytes in the blood;
- studies to identify the main markers of hepatotropic viruses, HIV;
- immunogram to assess immune function and possible concomitant autoimmune diseases;
- analysis to determine indicators of lipid and protein metabolism;
- test for blood glucose levels.
Also for liver intoxication:
- Ultrasound (usually reveals hepatomegaly, splenomegaly, characteristic changes in echostructure);
- Doppler ultrasound to assess blood flow in the portal and splenic veins;
- gastroscopy;
- elastography (non-invasive technique for diagnosing cirrhosis);
- CT or MRI;
- biopsy (if hepatocellular carcinoma is suspected).
Drug-induced liver damage: diagnosis, treatment
In recent years, the importance of drug-induced liver injury (DILI) has increased significantly; doctors of all specialties are faced with this problem. The difficulty of diagnosing DILI lies in the fact that clinical and laboratory manifestations and histological signs can “simulate” other liver diseases or overlap with existing viral and/or alcoholic liver damage. At the same time, DILI needs to be diagnosed at an earlier stage, since continued use of medications can greatly increase the severity of clinical manifestations and significantly affect the outcome of the disease as a whole. According to A.O. Bueverov [1], “the true prevalence of drug-induced liver damage remains and, apparently, will remain unknown, however, it can be stated that in clinical practice this diagnosis is formulated unreasonably rarely. This is due to several factors, among which the most important are: 1) the patient’s reluctance to report taking certain medications (antidepressants, antipsychotics, etc.); 2) reluctance of doctors to document iatrogenic diseases. General factors predisposing to the appearance of DILI are the following: 1) prescription of drugs in high doses; 2) dosing of the drug without taking into account the individual characteristics of the patient; 3) long-term treatment; 4) polypharmacy; 5) liver diseases of any etiology; 6) background systemic diseases (especially kidney diseases). Zimmerman in 1978 proposed classifying substances that cause liver damage into one of 2 groups: 1) obligate hepatotoxicants and 2) damaging the organ only in sensitive individuals (idiosyncratic) [2]. Obligate hepatotoxicants cause a predictable dose-dependent effect, usually reproducible in experiments on experimental animals. In a small proportion of people, medicinal substances that do not exhibit hepatotoxicant properties in experiments nevertheless cause liver damage. The phenomenon is based on genetically determined characteristics of the metabolism of xenobiotics and other reasons for the body’s increased susceptibility to the drug. This type of pathology is not reproduced experimentally and is not dose-dependent. The criteria for distinguishing between these forms are presented in Table 1. But in practice, it is not always possible to clearly distinguish between direct hepatotoxicity and idiosyncrasy. Moreover, in susceptible patients, some drug compounds that were previously classified as allergens appear to directly damage hepatocyte membranes through intermediate toxic metabolites.
A toxic substance can directly affect the structure of the hepatocyte (metabolite of paracetamol - N-acetyl-p-benzoquinone) and/or have an indirect effect on specific metabolic reactions (for example, inhibition of protein synthesis when using cytostatic antibiotics). Most direct hepatotoxicants cause dose-dependent liver necrosis, often in the presence of effects on other organs (kidneys). The classic drug with an obligate hepatotoxic effect is paracetamol. The basis of the toxic effect of drugs on the liver is damage to hepatocytes. The mechanisms underlying the hepatocytotoxic effect of drugs (Table 2) are closely interconnected and often aggravate each other’s effects in a “vicious circle” manner.
The spectrum of clinical manifestations of drug-induced liver disease can be extremely varied, but the most common are acute lesions of the hepatitis type (in approximately 80% of cases). Chronic DILI can be an independent disease (for example, with long-term use of methyldopa), but usually develops as the outcome of an acute pathological process (with long-term use of drugs or their combination). The severity of drug-induced liver diseases varies from an asymptomatic increase in transaminase levels to the development of fulminant liver failure (FLF). In addition to symptoms characteristic of liver diseases (jaundice, skin itching, “liver signs”, bleeding, liver enlargement and pain on palpation), general manifestations are often observed (nausea, abdominal discomfort, loss of appetite, general weakness, decreased ability to work). Although the development of acute liver failure is possible, in most cases drug reactions are transient and resolve spontaneously. The latent period when using hepatotoxic dose-dependent drugs is usually short (pathological manifestations develop within 48 hours from the start of administration). Depending on the degree of increase in the levels of alanine aminotransferase (ALT) and alkaline phosphatase (ALP), acute liver damage is classified as hepatocellular (cytolytic), cholestatic, or mixed, combining signs of cholestasis and cytolysis (Table 3).
More often, in 2/3 of cases, the hepatocellular type of damage occurs. An increase in ALT activity up to 5 times the upper limit of normal is considered moderate hyperenzymemia; 6–10 times – as moderate hyperenzymemia, more than 10 times – as high. In drug-induced liver diseases, elevated ALT levels are the most sensitive early diagnostic test. In mitochondrial hepatocytopathies, the activity of aspartate aminotransferase (AST) increases significantly. Depending on the underlying type of liver damage, clinical symptoms and changes in biochemical parameters can vary widely. Acute drug-induced hepatitis of varying severity
, is perhaps the most common drug-induced liver injury.
As a rule, it is caused by idiosyncratic reactions; the risk of developing drug-induced hepatitis increases with prolonged and repeated use of the drug. The clinical picture in the prodromal period is dominated by dyspeptic disorders, asthenic and allergic syndromes. With the development of the icteric period, darkening of the urine and lightening of the feces are noted, and enlargement and tenderness of the liver are detected. An increase in aminotransferase activity and alkaline phosphatase levels is directly dependent on cytolysis and the spread of liver necrosis. The level of γ-globulins in the serum increases. When the drug is discontinued, regression of clinical symptoms occurs quite quickly. In some cases, drug-induced hepatitis carries the risk of FPN, the mortality rate of which can reach 70%. Acute drug-induced hepatitis has been described with the prescription of antituberculosis agents (especially isoniazid), aminoglycosides (streptomycin, amikacin, rifampicin), antihypertensive drugs (methyldopa, atenolol, metoprolol, labetolol, acebutolol, enalapril, verapamil), antifungals (ketoconazole, fluconazole), antiandrogenic drugs drugs (flutamide), tacrine (a reversible cholinesterase inhibitor used for Alzheimer's disease), clonazepam (an anticonvulsant) [3, 4]. Steatohepatitis
.
Corticosteroids, tamoxifen, and estrogens may act as triggers for steatohepatitis in predisposed individuals, such as those with diabetes, central obesity, or hypertriglyceridemia. Drug-induced steatohepatitis usually develops during long-term pharmacotherapy (more than 6 months) and is apparently associated with the accumulation of drugs. Acute fatty liver changes can be caused by tetracyclines, NSAIDs, as well as corticosteroids, valproic acid and anticancer drugs. A feature of steatohepatitis caused by some drugs is its continued progression after discontinuation of the drug. Chronic drug-induced hepatitis
can also be caused by repeated prescriptions of nitrofurans for recurrent urinary infections, clometacin, fenofibrate (a lipid-lowering drug), isoniazid (a tuberculostatic), papaverine, minocycline (a tetracycline antibiotic) and dantrolene (a muscle relaxant, used to eliminate muscle spasms in cerebral palsy, multiple sclerosis and spinal cord injuries).
Chronic drug-induced hepatitis often develops in people who chronically drink alcohol. Acute cholestasis
has been described with the use of drugs of various pharmacological groups, including estrogens, anabolic steroids, tamoxifen, neuroleptics (chlorpromazine), statins, antibiotics (erythromycin, oxypenicillins, fluoroquinolones, amoxicillin/clavulanate), antiplatelet agents (ticlopidine), antihistamines (terfenadine ) and antifungal agents (terbinafine), NSAIDs (nimesulide, ibuprofen), antihypertensive (irbersartan) and antiarrhythmic drugs (propafenone), etc. Isolated hepatocellular cholestasis is more often observed with the use of sex hormones and anabolic steroids. Drug-induced cholangiopathy (cholestasis in small or interlobar ducts) can be acute and self-resolving after drug withdrawal or, on the contrary, take a protracted course, leading to ductopenia and sometimes biliary cirrhosis.
Diagnosis of drug-induced liver damage
Early diagnosis of DILI is of particular importance due to the high risk of disease progression without drug discontinuation. The possibility of lesions of this kind is taken into account when liver function is impaired in patients taking various drugs and alternative medicine. Due to the large number of asymptomatic drug-associated liver diseases in patients receiving hepatotoxic drugs and with polypharmacy, it is advisable to regularly (at least 1 time/2 weeks, and with long-term therapy - 1 time/month) determine the activity of aminotransferases , ALP and serum bilirubin levels. If transaminase activity is increased more than 3 times, the drug is discontinued. An alternative to discontinuing the drug, as well as if it is necessary to continue treatment with a hepatotoxic drug, is to reduce the dose of the hepatotoxicant and take an oral hepatoprotector. The drug of choice in this situation is drugs based on silymarin (Legalon). Indications for immediate discontinuation of the drug are the appearance of fever, rash or itching in the patient. The basis for diagnosing DILI is a carefully collected history of the medications used, assessing the duration and dose of the drugs received, and determining the possibility of taking them in the past. It is imperative to clarify your immediate medical history and find out whether you have taken biologically active food additives. They are not formally drugs, but are usually positioned as treatments for a wide range of diseases, including liver diseases, while the substances included in such drugs often have pronounced hepatotoxic properties (Table 4).
The diagnosis of drug-associated liver injury is in most cases a diagnosis of exclusion. A variant of the diagnostic algorithm is presented in Table 5.
With the help of biochemical and immunological studies, ultrasonography (and in some cases, other radiation diagnostic methods), liver diseases of a different etiology are established. But it should be remembered that DILI can overlap with “classical” liver disease and change its course. An attempt to re-expose the drug is unacceptable for ethical reasons. The diagnosis is confirmed if clinical symptoms, changes in biochemical parameters and histological signs of liver damage disappear or decrease after stopping the medication. Liver biopsy may be indicated if preexisting liver pathology is suspected or if biochemical parameters do not normalize after discontinuation of the drug. There are no specific histological changes for DILI. Granulomas, a significant admixture of eosinophils in the inflammatory infiltrate, and a clear zone of demarcation between the area of necrosis and unaffected parenchyma are often found. When making clinical and morphological comparisons, attention is drawn to the discrepancy between the severity and volume of morphological changes with the general relatively satisfactory condition of the patient and moderate changes in liver test parameters.
Treatment of drug-induced liver damage
The first step in the treatment of drug-associated liver disease should be discontinuation of the drug. In most cases, the drug quickly leads to a significant improvement in clinical and laboratory data. But in practical work, this is sometimes a very difficult task for a doctor, for example, when conducting chemotherapy in cancer patients, complex anti-tuberculosis treatment or treatment of neuropsychiatric diseases, diseases of the joints, heart, etc. In addition, multicomponent therapy, which is a complex potentially hepatotoxic substances, often does not allow us to specify the substance that caused the pathological reaction. If a doctor prescribes a drug with a known hepatotoxic effect (paracetamol, chemotherapeutic agents) or re-prescribes a course of drug treatment in which negative biochemical changes in liver tests were previously noted, hepatoprotective agents (milk thistle flavonoids) are included in the therapy from the first day of treatment (Table 6 ). In some cases, DILI can be prevented by adjusting the doses of medications used. For example, in people who chronically drink alcohol, the dose of paracetamol should not exceed 2 g/day. In case of hypersensitivity reactions, drugs that can cause cross-allergic reactions should be avoided, i.e. representatives of the same chemical group, for example, phenothiazines, tricyclic antidepressants, halogenated anesthetics, etc. The results of numerous experimental and clinical studies demonstrate a therapeutic effect in drug-associated liver diseases of some drugs from the group of hepatoprotectors. The very concept of “hepatoprotectors” is, by definition, not strict and is interpreted quite arbitrarily by different specialists. In the most common understanding, this is a class of drugs that, regardless of the mechanism of action, increase the functional ability of liver cells to synthesize, detoxify and excrete various biological products, and support the resistance of hepatocytes to various pathogenic influences [5]. The goals of prescribing hepatoprotectors for drug-induced liver diseases are to restore and/or maintain liver cell homeostasis. In clinical practice in previous years, a variety of drugs were used as hepatoprotectors, many of which turned out to be ineffective and fell out of use. Currently, for drug-associated liver diseases, the drugs presented in Table 6 are predominantly used. The main requirements for an “ideal” hepatoprotector were formulated by R. Preisig: – fairly complete absorption; – the presence of a first-pass effect through the liver; – pronounced ability to bind or prevent the formation of highly active damaging compounds; – the ability to reduce excessive inflammation; – suppression of fibrogenesis; – stimulation of liver regeneration; – natural metabolism in liver pathology; – extensive enterohepatic circulation; – lack of toxicity. In the practice of a therapist who often deals with manifestations of moderate hepatotoxicity of medications, it is advisable to use not infusion, but oral forms of hepatoprotectors, which do not require patients to stay even in a day hospital. This condition is best met by the original preparation based on milk thistle, containing the maximum amount of silymarin. Silymarin is the common name for chemically related flavonolignan isomers from milk thistle fruit. The main bioflavonoids in silymarin are: silibinin, silydianin, silicristin, isosilibinin, among which silibinin has the greatest biological activity. The full range of actions of silymarin, using the example of the original drug Legalon, is reflected in Table 8. Numerous studies have proven that silibinin contributes to a significant increase in the content of reduced glutathione in the liver, thereby increasing the organ’s protection from oxidative stress, maintaining normal detoxification function of the liver. The hepatoprotective properties of silymarin (silibinin) are associated not only with the restoration of the liver’s own antioxidant systems. Silymarin itself is an antioxidant due to the presence of a phenolic structure in the molecule. Silibinin binds free radicals in hepatocytes and converts them into less aggressive compounds. Thus, the process of lipid peroxidation (LPO) is interrupted and further destruction of cellular structures does not occur. At the same time, it inhibits both the formation of malondialdehyde, a marker of oxidative stress, and prevents the effect of TNF-α on the activation of reactive oxygen species, which also leads to the interruption of the LPO process. The antioxidant effect of silymarin and inhibition of lipid peroxidation reactions have been clearly demonstrated in vitro. Milk thistle flavonoids exhibit 10 times higher antioxidant activity than tocopherol. The mechanism of the anti-inflammatory effect of silibinin is associated with its ability to inhibit the lipoxygenase pathway of arachidonic acid metabolism with suppression of the synthesis of active inflammatory mediators, especially leukotrienes B-4 in Kupffer cells. A large number of experiments have demonstrated the ability of silymarin to suppress the activation of NF-kB in cell cultures. NF-kB is a key regulator of inflammatory and immune responses, which binds to DNA and induces gene expression. An important aspect of the metabolic action of milk thistle flavonoids is the ability to activate the synthesis of proteins and phospholipids and support the process of hepatocyte regeneration. Silibinin stimulates the activity of nuclear RNA polymerase A in hepatocytes, accelerates transcription and the rate of RNA synthesis, which, in turn, leads to an increase in the number of ribosomes and activation of the biosynthesis of structural and functional proteins. Comparative characteristics of silymarin-containing drugs are presented in Table 7. Hepatoprotector Legalon, obtained from milk thistle fruits, includes the maximum amount of silymarin and silibinin thanks to a patented production technology that increases the concentration of silibinin in the medicinal substrate. This makes it possible to achieve higher bioavailability compared to similar drugs, i.e., it satisfies most of the requirements for hepatoprotectors. When taken orally, the drug Legalon quickly dissolves and enters the intestines. After absorption in the intestine through the portal vein system, 85% of silibinin enters the liver after 45 minutes and is selectively distributed in hepatocytes. In the liver, silymarin is metabolized by conjugation and does not form active metabolites. 80% of the active substance during the first passage through the liver is excreted in the bile in combination with glucuronides and sulfates. Due to deconjugation in the intestine, up to 40% of silymarin excreted in the bile is reabsorbed and enters the enterohepatic circulation. The maximum concentration in bile is 100 times higher than in plasma. The concentration of silibinin stabilizes after repeated doses, and the drug does not accumulate in the body. The regenerative mechanism of action of Legalon is due to the possibility of forming a complex with steroid cytoplasmic receptors and is transported into the cell nucleus, where it activates RNA polymerase A. At the same time, silibinin does not affect the rate of reduplication and transcription in altered cells with a maximum level of DNA synthesis, which excludes the possibility of its proliferative actions. FDA1 and EMEA2 experts approved the use of the drug Legalon as a hepatoprotective agent with a proven ability to restore the detoxification function of the liver (Table 8).
Legalon should be accompanied by drug therapy from the first days of treatment, because, according to numerous studies, an earlier start of hepatoprotective protection significantly reduces the risk of chronic disease. The drug is advisable to use in patients with DILI with clinical and biochemical signs of activity in preventive courses if long-term use of hepatotoxic drugs (for example, cytostatics, NSAIDs, antiarrhythmic drugs, antidepressants, contraceptives, etc.) is necessary, with forced polypharmacy (a special risk group is women after 40 years). Drug therapy for patients with a history of diffuse liver diseases of any etiology or suffering from alcohol and nicotine addiction should also be carried out in combination with taking Legalon. Prophylactic use of the drug is recommended for workers in hazardous chemical industries. Directions for use: 1. For DILI with moderately severe cytolytic syndrome: 70 mg 3 times a day for 3–4 months. 2. For severe DILI: 140 mg 3 times a day for 3–4 weeks, with a transition to maintenance doses of 70 mg 3 times a day for 3–4 months. 3. For chronic liver intoxication (drugs, industrial, household hepatotoxic compounds): 70 mg 3 times a day in courses of 3–4 months. 2–3 rubles/year. 4. If drug therapy is necessary for patients with diffuse liver diseases of any etiology: 140 mg 3 times during treatment and then 70 mg for 3–4 months. 5. For the prevention of DILI for workers in hazardous industries: 70 mg for a long time. Treatment of DILI remains a traditionally difficult problem for practitioners. Discontinuation of a hepatotoxic drug is often impossible without creating an immediate or delayed threat to the patient's life, or without significantly deteriorating the patient's quality of life. At the same time, widely known data on the ability of liver tissue to regenerate allow us to fairly optimistically assess the prospects and potential possibilities of pathogenetic therapy of drug-induced liver damage with hepatoprotectors.
Conclusion
The liver metabolizes most drugs. In case of liver diseases of any etiology, with long-term use of drugs, polypharmacy, its ability to metabolize drugs is impaired, therefore, when they are prescribed in normal dosages, unexpected toxic reactions may occur. The possibility of toxic effects of drugs should always be taken into account in the differential diagnosis of liver failure, jaundice, and increased transaminase levels. An isolated increase in cytolysis markers while taking medications should be treated with great caution, since this may indicate the development of drug-induced liver pathology. Detection of drug-induced hepatitis remains one of the most difficult challenges in medicine. The diagnosis is rarely made and, as a rule, at the stage of jaundice or hepatomegaly. The range of clinical manifestations of liver diseases caused by medicinal substances is extremely diverse, these manifestations often have similarities with the “classical” forms of liver diseases. The basis of diagnosis is a carefully collected anamnesis of the medications used. It should be borne in mind (due to the large number of oligosymptomatic DILI) that in patients receiving potentially hepatotoxic drugs, it is advisable to regularly determine the activity of aminotransferases, alkaline phosphatase and the level of bilirubin in the blood serum. Hepatoprotective agents are used to accelerate the restoration of liver structure and function. For outpatient clinics, it is advisable to use oral forms of medications based on silymarin from the first day of drug therapy. The drug of choice among silymarin-containing hepatoprotectors is the original hepatoprotector Legalon.
1
The Food and Drug Administration is a government agency subordinate to the US Department of Health. 2 European Medicines Agency (EMEA, European Medicines Agency) is an agency that evaluates medicinal products for their compliance with the requirements set out in the European Pharmacopoeia.
Principles of treatment
Treatment of alcoholic liver intoxication is impossible without complete abstinence from alcohol. Therefore, the main attention is paid to detoxification of the body, coding (medicines are used with caution, preference is given to hardware coding, hypnotherapy), and psychotherapy.
Nutrition correction
The diet should be balanced, high-calorie (up to 35 kcal/kg per day), contain a sufficient amount of protein (1 g/kg, but with the development of hepatic encephalopathy, the daily intake of protein foods is reduced to 20 g with simultaneous intravenous administration of amino acid solutions), unsaturated fatty acids, vitamins, macroelements. Naturally, fatty, fried foods, pickles, smoked meats, sausages, confectionery, etc. are completely excluded from the diet.
Drug treatment
To accelerate the regeneration of hepatocytes, reduce the activity of lipid peroxidation reactions, and eliminate the manifestations of cholestasis and fibrosis, the following is prescribed:
- corticosteroids (used with caution for concomitant viral, bacterial and fungal infections) for 7–14 days, followed by a gradual reduction in dose;
- herbal and combined hepatoprotectors, preparations containing essential phospholipids (these are one of the structural components of liver cell membranes);
- vitamins (thiamine, pyridoxine, cobalamin, nicotinic, ascorbic, folic acid, tocophelol, retinol);
- microelements (necessarily medications containing potassium, phosphorus, magnesium, zinc);
- antioxidants;
- pancreatic enzymes;
- diuretics;
- probiotics;
- selective immunosuppressants (if concomitant autoimmune disorders are detected);
- specific antiviral drugs (if hepatitis C has been diagnosed), etc.
The duration of treatment for alcoholic liver poisoning, as well as the need for hospitalization, is determined individually. When contacting a specialist and abstaining from alcohol in the early stages of the disease, a positive result can be achieved in 90% of patients. But as pathological changes in the liver progress, the chances of healing rapidly decrease.
Caution - danger!
The main enemies of the liver are considered to be alcohol and drugs, but they receive the palm rather for the number of victims than for the strength of the impact. Toxins contained in some poisonous mushrooms are considered to be much more powerful toxic substances that can completely destroy the liver, and lovers of “quiet hunting” risk much more than alcohol lovers. The fact is that microdoses of fungal toxin are sufficient to completely disable the liver, and not all toxic compounds are destroyed during heat treatment. Moreover, even mild mushroom poisoning weakens the body forever, and subsequent liver intoxication can be fatal. No less dangerous are the bites of certain snakes, insects, and the consumption of poisonous plants and berries.
The second deadly enemy of the liver is hepatitis viruses, including hepatitis A, which also leave a mark forever and weaken the liver even if treatment is started in a timely manner. Diabetes, enzyme deficiency, bacterial infections and parasites also require adequate treatment, because they gradually destroy the liver, poisoning hepatocytes with substances that are unsuitable for processing and excretion.
However, treatment can also be a risk factor: many antipyretics, painkillers and non-steroidal anti-inflammatory drugs, as well as some other drugs or excessive intake of seemingly harmless vitamin A can provoke necrosis of hepatocytes. And, despite the ability of cells to regenerate, intoxication of the liver with drugs can make a person disabled or even kill.
Working with poisons, in harmful and dangerous industries, being in areas of industrial accidents and pollution, living near landfills, smoking and alcoholism are factors in the gradual poisoning of the liver, leading to chronic intoxication. The presence of any of the risk factors means that you need to closely monitor your health and consult a doctor as soon as any symptom of liver poisoning is noticed.
Literature:
- M.A. Livzan, Doctor of Medical Sciences, Professor, E.A. Lyalukova, Ph.D. Alcoholic liver disease: modern aspects of diagnosis and treatment. Omsk State Medical Academy of the Ministry of Health of Russia, 2014.
- E.Yu. Eremina. Alcoholic liver disease. Parts 1, 2. Federal State Budgetary Educational Institution of Higher Professional Education Mordovian State University named after. N.P. Ogareva, Department of Propaedeutics of Internal Diseases, 2012
- Diseases of the liver and biliary tract. Ed. V.T. Ivashkina. Guide for doctors, 2nd ed., rev. and additional M.: Publishing house. House M-Vesti, 2005. 536 p.
- Moiseev V.S. Alcoholic liver disease. Clinical hepatology, 2006. No. 1. pp. 3-8.
- A.A. Antonyan, E.I. Kashkina, R.V. Lyakisheva. Modern ideas about alcoholic liver disease. Saratov Medical Scientific Journal, 2010, volume 6, No. 2, p. 317-322.
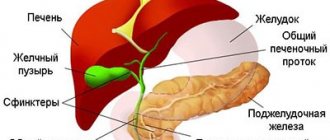
The role of the liver in the human body
The role of the liver in the metabolism of chemicals entering the human body is extremely large. The liver is a multifunctional organ that performs a variety of functions.
- One of the most important is the detoxification function - the neutralization of toxic substances of endogenous and exogenous origin, the formation and elimination of non-toxic substances.
- The liver is involved in protein, carbohydrate, fat, vitamin and mineral metabolism, hormone synthesis, and hematopoiesis.
- The liver performs a function related to the formation of bile, which is involved in digestion.
- The liver is one of the most important organs in the human body.
What to do if there are signs of intoxication?
If you are constantly in a bad mood, it is difficult for you to wake up in the morning with adequate sleep time (7-9 hours), and you want to sleep during the day, this is a reason to check your health. Perhaps it's not the liver, but a deficiency of vitamins and minerals. But the liver can also give such unobvious SOS signals. Moreover, at the initial stage of almost all liver diseases, these strange symptoms appear. Therefore, at the first signs of intoxication, it is better to do an ultrasound of the abdominal organs and take a blood test for ALT/AST enzymes.
Next, based on the examination results, the doctor will suggest a treatment strategy. If there is liver disease, you must first eliminate its cause, and then restore the functioning of the organ with the help of diet, moderate physical activity and hepatoprotectors. When the liver returns to normal, the detoxification process will restore itself. During therapy, enterosorbents, clean drinking water and herbal decoctions will help with the removal of toxins.
It is important to understand that both processes - removing toxins and healing the liver - must take place in parallel with each other. If you do not treat the disease that led to intoxication, it will never end. And the disease, in turn, will progress.
How does mild intoxication feel?
Chronic intoxication, which is characteristic of liver diseases, is called toxic hepatitis. It is characterized by the following manifestations:
- heaviness and pain in the right side
- increase in liver size
- poor appetite
- nausea and bitterness in the mouth
- increased gas formation
- diarrhea, skin itching, rashes
- low-grade fever (body temperature up to 37–37.5 °C)
- increased fatigue
- poor tolerance to usual stress
- drowsiness, apathy, bad mood
The more severe the liver disease, the worse it neutralizes toxins. Accordingly, with advanced viral hepatitis, steatohepatitis, liver cirrhosis and liver failure, the signs of intoxication are very pronounced. With NAFLD and ALD, the symptoms may be less significant, but they still exist.
– A mild degree of permanent intoxication occurs with diseases of the intestines and liver. Excess bacteria in the intestines release a lot of endotoxins and lipopolysaccharides. The liver may not be able to detoxify toxins. Then you need to remove intoxication and heal the intestines, writes hepatologist Sergei Vyalov on his Instagram.