The article was prepared by a specialist for informational purposes only. We urge you not to self-medicate. When the first symptoms appear, consult a doctor.
The liver is the organ that does not make itself known for a long time in case of illness. Most often they are discovered during ultrasound diagnostics. And quite often in the extract you can find a small but frightening note - diffuse changes in the liver parenchyma. Don't panic, first you should try to understand what this phrase means. There is no such diagnosis as “diffuse changes in the liver parenchyma”. The recording can only mean that certain processes are occurring in the organ that caused such a condition. But why this happened needs to be determined with the help of various types of research.
Diffuse changes can be a symptom of the following diseases:
- cirrhosis
- any hepatitis
- sclerosing cholangitis
- autoimmune hepatitis
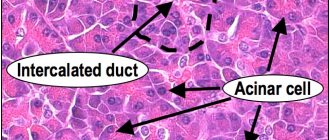
To understand what we are talking about, you should know that the parenchyma is not a shell, but a collection of the most important elements responsible for the functioning of the organ. The liver consists entirely of parenchymal tissue, which, in turn, is formed from certain cells - hepatocytes.
Therefore, when the doctor says that the parenchyma has diffuse changes, he means transformation of the liver tissue. Thus, minor deviations may be a consequence of a viral disease. But there are also severe lesions, so it is necessary to conduct additional studies that will reveal the full depth of liver damage. But in any case, diffuse changes in the liver parenchyma cannot be ignored, and identifying the causes that led to such a condition is the key to successful treatment.
What does “diffuse liver changes” mean?
Diffuse changes are not a separate disease, but a consequence of long-term pathological processes. The term is used when undergoing an ultrasound examination. During the examination, the diagnostician sees structural changes affecting the tissues of the organ.
With focal changes, a specific area suffers, and with diffuse changes, the entire organ at once.
According to the degree of manifestation, the violation is divided into 3 groups:
- moderate;
- minor;
- expressed.
Moderate diffuse changes occur with prolonged abuse of alcoholic beverages, large amounts of fatty foods in the diet and intoxication processes due to medications. Minor tissue changes are diagnosed in the early stages of diseases, with bacterial or viral inflammation.
The causes of pronounced changes are secondary or primary cancer tumors, cirrhosis, excess weight, diabetes mellitus or chronic hepatitis. The edematous organ increases in size several times, and functionality is impaired.
Changes in structure and structure are divided into 3 types:
- by type of fatty infiltration;
- by type of hepatosis;
- according to the type of steatosis.
The gland is involved in the process of nutrient metabolism. Under the influence of enzymes in the intestines, the breakdown of fats coming from food occurs. The liver converts them into triglycerides and cholesterol. With diffuse changes, they accumulate in the tissues of the organ, disrupting its activity.
A healthy gland is homogeneous, with a large number of bile ducts and blood vessels. With hepatic changes, excess fat accumulates inside the cells, leading to the gradual destruction of healthy hepatocytes.
With steatotic disorders, scattered fat accumulations appear in the liver. Because of this, healthy cells are destroyed, causing the formation of cysts. The result is pathological irreversible structural changes.
General information
Speaking about diffuse changes in the liver , you should first of all understand what this concept means. This condition is not a disease, but a symptom of diseases that manifest themselves as a result of decreased immunity , poor nutrition, alcohol abuse, taking toxic medications, etc. Due to negative effects, connections between molecules are disrupted.
The functions of hepatocytes also change, as a result of which the fatty and connective layer increases. In fact, this is one of the manifestations of liver pathologies, and the correct diagnosis can only be established after a comprehensive examination and consultation with a hepatologist.
This article will discuss how to diagnose this pathology and what needs to be done to improve the condition of the liver.
Reasons for the development of pathology
Diffuse changes can occur against the background of chronic diseases or under the influence of negative factors. In most cases, the process is irreversible, even if the patient begins treatment.
Diseases
During an ultrasound of the liver, diffuse changes are displayed in a number of diseases. The list includes:
- parasitic infestation;
- diabetes;
- advanced obesity;
- viral inflammation;
- hepatitis;
- neoplasms;
- cirrhosis.
With obesity and diabetes, there is more iron, and tissue echogenicity increases significantly. Viruses trigger the process of tissue degeneration, but after treatment the process stops and spontaneous restoration to physiological norm occurs.
Predisposing factors
Violations lead to:
- Frequent stress and overload
. Due to psycho-emotional problems, the production of adrenaline increases in the adrenal glands. The hormone is broken down by the liver, and its excessive amount leads to damage to hepatocytes. - Unhealthy eating
. Fatty and heavy foods create additional stress on the organ, which leads to rapid “wear and tear”. - Ecological situation
. Various toxic substances are transported to the liver through the bloodstream. Due to frequent overloads, the neutralization process is disrupted and the organ is gradually poisoned. Even life near major highways is dangerous. - Alcoholism
. Liver enzymes process ethyl alcohol, and it breaks down into aldehydes. They lead to the destruction of healthy areas of tissue, which are replaced by fatty patches. - Drug therapy
. Some medications contain substances with hepatotoxic effects. Violation of the dosage or too long treatment “kills” the liver.
With timely detection of the pathological process on ultrasound, the negative effect can be reversible.
Treatment recommendations
The main directions of therapy are following a diet and taking medications. Dietary nutrition involves regularly eating healthy foods in small portions. Thanks to this, not only the pain syndrome is reduced, but the general condition is alleviated.
The diet should include foods that do not “load” hepatocytes, but, on the contrary, protect by normalizing metabolism and delivering vitamins and microelements.
Doctors recommend reducing the caloric content of the diet, reducing the amount of protein foods of animal origin, as well as salt and fatty foods. Diet No. 5, 5a is prescribed for the treatment of hepatitis and cirrhosis. It includes:
- daily calorie content not exceeding 3 thousand calories;
- meals should be taken every 2-3 hours;
- emphasis on boiled, steamed, baked dishes;
- exclusion of trans fats (margarine, fast food, canned foods);
- enriching the diet with fresh vegetables, fruits, and vegetable proteins;
- control over the drinking regime (up to two liters per day).
Of the foods allowed in diet No. 5, it is worth highlighting:
- low-fat dairy products;
- fish, lean meat;
- porridge (buckwheat, rice);
- vegetable soups;
- herbal teas, juices.
It is recommended to avoid:
fatty meats and fish;- pickles;
- canned food;
- spices;
- smoked meats;
- fatty broths;
- muffins;
- sweets;
- alcohol, carbonated drinks, coffee.
Drug therapy is tailored to the cause of the disease. Prescription of diet and drug treatment should be carried out by a doctor based on laboratory and instrumental diagnostic data.
Therapy may include the following groups of drugs:
- antivirals, necessary for the treatment of infectious hepatitis;
- detoxification (often in the form of solutions for infusion);
- hepatoprotectors;
- vitamin complexes;
- immunomodulators;
- drugs that affect the production and movement of bile.
Do not forget that the success of therapy depends on the continued influence of a negative factor (alcohol, viruses, hepatotoxic drugs).
Only after the stress factor has been completely eliminated can we hope for recovery.
Signs of diffuse changes
Symptoms of changes depend on the underlying disease.
Similar signs include:
- fragility of blood vessels;
- digestive problems;
- increased fatigue;
- constant weakness;
- changing the structure of the language;
- frequent mood swings;
- slight increase in temperature.
With liver problems, patients often complain of constant heartburn and nausea after eating. Feces change color, becoming whitish or almost black. Noticeable cracks appear on the surface of the tongue, and a white or yellowish dense coating is possible.
Sweating becomes more frequent, and an unpleasant, pungent odor appears, even soon after taking a shower. The condition of the skin worsens: it acquires a yellow tint, quickly dries and flakes. Acne and allergy symptoms are often observed. In the morning and after eating inappropriate foods, an unpleasant bitter taste remains in the mouth.
Important! If the liver parenchyma increases, nearby organs suffer. Due to pressure, pain occurs in the pancreas, spleen or gallbladder. There are no nerve endings in the liver itself and it rarely hurts, which is why patients seek help too late.
Pathogenesis
The pathogenetic process of fatty hepatosis has not been sufficiently studied. Clinically, it is generally accepted that fatty hepatosis directly precedes the development of non-alcoholic fatty liver disease. The development of the disease, the actual accumulation of lipids, may be a consequence of:
- Increased intake of free fatty acids into the liver tissue.
- A sharp decrease in the rate of b-oxidation of acids in hepatic mitochondria.
- Increased synthesis of fatty acids in hepatomitochondria.
At the same time, the process of removing fat from the liver is hampered due to reduced synthesis of lipoproteins and the elimination of triglycerides in their composition.
Next, steatohepatitis is formed, accompanied by inflammatory-necrotic liver changes. This is the conditional “first push”. The role of the “second push” is associated with the use of certain groups of medications, which are a source of radicals that stimulate oxidative stress and the production of inflammatory mediators. As a result, microcirculation and metabolic processes are disrupted, liver ducts become clogged, and degenerative tissue changes develop.
Diagnostics
The main diagnostic method is ultrasound examination, which reveals echographic signs of changes.
If necessary, additional research methods are prescribed.
| Type of study | Goals | What will show |
| Blood for hepatitis | Determines the presence of hepatitis, the level of pathogen activity, and the type of disease. | The presence or absence of specific antibodies to the virus. |
| Radionuclide scanning | Displaying the presence of echo signs of changes. | Based on the nature of the distribution of the contrast agent, specialists evaluate the echostructure of the liver tissue. It is also possible to identify post-traumatic changes or metastases. |
| Blood biochemistry | Assessment of the functional activity of hepatocytes. | Bilirubin and ALT increase, albumin levels become lower. |
| CT | Shows small tumors, helps determine the presence of parenchymal bleeding. | |
| Fine needle biopsy | Histological examination. | Carried out to confirm cancer. |
A healthy liver on ultrasound is homogeneous, with fine granularity, weakly intense echogenicity, and further decreases in the area where the vessels are located. With fatty hepatosis, an increase in the echo signal occurs over the entire area of the gland. The organ has rounded edges, hepatomegaly (increase in size) is noticeable.
The main sign of cirrhosis is a lumpy liver. False lobules appear due to connective tissue. The surface of the organ is heterogeneous and uneven, the tissues are compacted. Hepatocytes are uneven: one part atrophies, the other compensatory increases. The vascular pattern of the liver is enhanced.
Diagnostic measures
To make a correct diagnosis you need:
- collection of anamnestic information. Attention should be focused on previous use of hepatotoxic medications, alcohol abuse, dietary errors, as well as past infectious diseases;
- complaint survey;
- conducting a physical examination, during which the doctor palpates the abdomen, determines the size and consistency of the liver, and assesses the severity of pain;
- laboratory diagnostics. To determine liver dysfunction, a biochemical analysis is required (of interest is the level of transaminases, alkaline phosphatase, total protein, bilirubin), a coagulogram (to assess the functioning of the coagulation system), a clinical blood test, and urine;
- instrumental diagnostics (ultrasound, tomographic examination).
If liver compaction cannot be diagnosed non-invasively, fine-needle puncture or laparoscopic examination may be performed.
Treatment
Therapy of diffuse changes requires an integrated approach, including:
- drug treatment;
- vitamin therapy;
- diet;
- rejection of bad habits.
The patient will have to regularly visit the doctor, take tests and undergo ultrasound examinations to monitor the results of treatment and the current condition of the organ.
Medicines
Medicines are selected individually, depending on the underlying disease, the patient’s age and the condition of the liver.
Therapy may include:
- Immunostimulants and antivirals (Cycloferon, Ribavirin). Increases the body's resistance and reduces the activity of hepatitis viruses.
- Plant hepatoprotectors (Silymarin, Gepabene, Karsil). Prescribed for toxic lesions, cholecystitis, cirrhosis. They protect the liver from harmful effects, stimulate the regeneration process, and stop the destruction of cell membranes.
- Amino acids (Heptor, Heptral). Accelerate the recovery of hepatocytes, have antioxidant and desontification effects.
- Preparations based on beef liver hydrolysates (Sirepar, Gepatosan). Protect the organ, cleanse the blood.
- Choleretic (Ursofalk, Odeston, Holemaks). Restores normal bile flow and relieves spasms.
- Phospholipids (Essliver, Essentiale Forte, Phosphogliv). Normalize metabolism in liver tissues.
The dosage and duration of the course are determined by the attending physician. Additionally, vitamin-mineral complexes and preparations are selected to restore the microflora of the gastrointestinal tract. During pregnancy, many of the drugs are contraindicated; therapy is carried out on an individual basis.
How to treat with folk remedies?
Traditional medicine recipes are used as aids. First make sure there are no contraindications for the ingredients used.
Olive oil
The oil helps cleanse the liver of toxins; it should be drunk in its pure form.
During the first 14 days, 0.5 tsp is enough. once a day. Afterwards the quantity increases to 1 tbsp. l. The maximum duration of the course is a month.
Drink with oats
Oats cleanse the blood, birch buds restore metabolism and correct high cholesterol levels. Lingonberries (both berries and leaves) relieve inflammation.
You will need:
- 3 cups dry oats;
- 3 tbsp. l. birch buds;
- 3 tbsp. l. lingonberry leaves.
Grind all the ingredients, pour in 3 liters of cold drinking water, leave in a dark, warm place for 24 hours. After the time has passed, place everything in an enamel bowl and place on low heat. When the broth boils, remove and cool the liquid. Drink 150 ml before meals for a month.
Decoction with honey
Natural honey helps renew tissues and increases glycogen in the liver. Cinnamon normalizes digestion, has a positive effect on the body's condition in diabetes, and helps cleanse the body of toxins and waste. Wormwood is used to combat pathological microorganisms.
The recipe includes:
- 1 tsp. chopped cinnamon;
- 1 tsp. wormwood;
- 200 ml water;
- 300 g honey.
Pour water over wormwood and cinnamon and bring to a boil over low heat. Add natural honey, cook until the mixture becomes thick. Drink 1 tsp. during meals 3 times a day. The course lasts 3-4 weeks. Store the finished product in the refrigerator.
Corn silk tea
Corn “hairs” help control blood sugar, neutralize toxins, restore metabolism, and improve liver and pancreas function.
For tea you will need:
- 300 g corn silk;
- 3 liters of hot water.
Pour boiling water over the hairs and leave for a day. It is recommended to store the liquid in a thermos. Drink 150-200 ml in the morning and evening. The duration of use is not limited.
Rose hip decoction
Due to its vitamin composition, rosehip supports the immune system. Phytoncides and mineral components have choleretic and diuretic effects, due to which they help alleviate the condition of pathologies of the kidneys, gall bladder and liver.
Prepare for the decoction:
- 200 g rose hips;
- 1 liter of hot water.
Grind the fruits with a blender and add hot water. Boil the mixture over low heat for 10 minutes. Pour the finished broth into a thermos and let it brew for 12-15 hours. You need to drink the entire amount within 5 days; store the leftovers in the refrigerator. Take a decoction of 150 ml per 30 minutes. before meals, no more than 4 times a day. The duration of the course is 10 days.
Diet
{banner_banstat9}
If liver activity is impaired, “heavy” foods that create extra stress are excluded from the diet. Steam, boil or bake food. Frying (especially using oil or animal fat) is removed.
The following products will have to be removed from the menu:
- canned food;
- mushrooms;
- fatty fish;
- smoked meats;
- pickles;
- sausages;
- salo;
- fatty meats;
- legumes
It is strictly forbidden to drink alcohol in any quantity. It is also recommended to give up strong tea and coffee, and carbonated drinks.
It is allowed to eat a small amount of white bread, but it will have to be dried first. The basis of the diet should be cereals, lean meat, lean vegetable soups, fruits and vegetables. Kefir, milk, cheeses and sour cream - only with a low percentage of fat content.
Surgical intervention
{banner_banstat10}
If conservative treatment methods do not bring results, surgical intervention is recommended. It consists of partial or complete removal of the liver and other affected internal organs.
The operation is necessary when:
- advanced hepatitis;
- severe cirrhosis;
- cysts;
- large neoplasms;
- portal hypertension;
- cancer metastases.
In case of complete removal, the patient needs a liver transplant.
Alternative medicine
Experts recommend using traditional medicine recipes in combination with basic therapy. However, this must be done strictly after consultation with your doctor. At home, you can easily make your own healing decoctions, as well as infusions based on the following ingredients:
- Mint.
- Oats.
- Propolis.
- Corn silk.
- Chamomile.
- Fennel.
- Yarrow.
- Birch buds.
- Pumpkin seeds.
- Rose hip.
- Calendula.
- Lingonberry leaves.
- Apricot kernels.
Possible consequences and complications
Even minor diffuse changes can lead to the formation of chronic pathologies.
These include:
- infertility;
- encephalopathy;
- malabsorption syndrome;
- ascites;
- liver failure;
- extensive internal hemorrhages.
With timely initiation of treatment, the prognosis is quite favorable and the functioning of the organ can be restored in full.
List of sources
- Diseases of the liver and biliary tract: A guide for doctors / Ed. V.T. Ivashkina. M.: M-Vesti, 2002. 416 p.
- Ivashkin V.T., Yushchuk N.D. Diagnosis and treatment of diffuse liver diseases. Method, manual for doctors. M.: 2003. - 49 p.
- Mizandari M., Mtvardze A., Urushadze O. et al. Complex radiodiagnosis of diffuse liver pathology // Med. visualization. - 2002. - No. 1. - P. 60-68.
- Panfilov S.A., Panfilova E.V. Diagnosis of liver and biliary tract diseases with a course of pathological anatomy. - M.: Binom. Knowledge Laboratory, 2003. 211 p.
- Stepanyan I.A., Kobinets Yu.V., Izranov V.A., Ovchinnikov O.I. Diffuse liver changes: assessment of diagnostic efficiency using standardized arfi-elastometry. Radiation diagnostics and therapy. 2018;(1):30-35.
Prevention
A healthy lifestyle, proper nutrition and avoidance of alcoholic beverages will help you avoid liver problems. To minimize the risk of hepatitis B, vaccination is necessary. At the first suspicion of organ pathology, seek help from a doctor. Doctors also recommend regularly (at least once a year) diagnostic ultrasound of the abdominal organs: this will allow timely detection of developing disorders.
The liver is a large and hardy organ. With local dystrophic changes, a compensatory process is triggered: the gland increases in size to help the body survive. The appearance of alarming symptoms indicates serious problems that require specialist intervention.
Clinical symptoms
The disease at the initial stage is asymptomatic. The first signs appear only after the pathological process has transitioned to pronounced fibrosis. At this stage, symptoms such as:
- significant discomfort in the right hypochondrium;
- yellowness of the skin and sclera;
- enlarged liver and spleen;
- spider veins, a symptom of “liver” palms;
- gastrointestinal dysfunction: regular nausea, episodes of vomiting and diarrhea, flatulence;
- intolerance to spicy and fatty foods;
- asthenovegetative syndrome: causeless fatigue, emotional instability, sleep disturbances, etc.
When diffuse organ damage develops, severe severe manifestations join the general symptoms:
- diffuse hemorrhages;
- stable fever;
- hypotension;
- periodic loss of consciousness;
- visual impairment;
- ascites.
If such symptoms develop, emergency hospitalization is indicated.
specialist
Our doctors will answer any questions you may have
Tumasova Anna Valerievna Gastroenterologist