Back to list Previous article Next article
18.06.2012
Tags:
Klebsiella, microflora
5/5 — (7 votes)
In the summer, diseases caused by infectious agents become relevant.
Microorganisms of the enterobacteria family are especially active - gram-negative, rod-shaped, with flagella for movement and attachment, facultative anaerobes: Escherichia coli, salmonella, klebsiella, etc. Thus, Klebsiella - klebsiella , can exist in soil, water, remaining viable for months, persists on food and dust.
Klebsiella can enter the body through the gastrointestinal tract, from poorly washed hands, vegetables and fruits, from water, from soil. However, this microorganism belongs to the group of opportunistic microflora and is detected in absolutely healthy children and adults; it is considered one of the elements of normal intestinal flora .
At the same time, Klebsiella is one of the most common nosocomial infections , because it is resistant to environmental factors and high temperatures. Although, in a few minutes it dies from disinfectants, and at very high temperatures in 1-1.5 hours. If proper hygiene rules and sanitary standards in the premises are not observed, there are cases of infection of newborns with Klebsiella in maternity hospitals. The baby constantly cries and cannot fall asleep, he is bothered by colic and frequent diarrhea. And the reason is Klebsiella - a bacterium resistant to the harmful effects of the external environment, covered with a dense capsule.
Basic information about the bacterium
Klebsiella
Klebsiella is a bacteria from the Enterobacteriaceae family that can cause numerous diseases. The microorganisms are named after the pioneering scientist Edwin Klebs, who studied pathogenic microorganisms in the 19th century.
These are small gram-negative bacteria with a polysaccharide capsule. The main danger of Klebsiella is associated with their resistance to many antimicrobial medications.
Different types of Klebsiella are found everywhere. The diversity of habitats is associated with the wide adaptation capabilities of the microorganism. Depending on the niche they occupy, bacteria rearrange their own biochemical reactions, which allows them to survive even in an unfavorable environment.
Most species of the organism can be found in water, soil, on the surface of plants, insects and other animals, including humans.
Klebsiella are prominent representatives of facultative anaerobes. All major biochemical reactions of the body occur in the absence of oxygen, but the bacterium can survive with access to atmospheric air.
In addition, these gram-negative organisms do not have specific growth requirements, unlike other members of the Enterobacteriaceae family. In the human body, Klebsiella lives in the nose, mouth and intestines. Bacteria can also penetrate the membranes of the brain and urogenital tract.
Pneumonia
Klebsiella is a pathogenic microorganism
Pneumonia is the most common form of infection caused by Klebsiella infestation. This is an inflammation of the lung tissue, accompanied by the appearance of exudate and pus in the organ.
The disease is accompanied by cough with sputum, fever, chills, shortness of breath and other symptoms. People who are being treated in a hospital are at greatest risk of this form of pneumonia.
Thus, Klebsiella can cause hospital-acquired pneumonia that is resistant to a number of antibiotics.
Possible symptoms of the disease:
- Chest pain when breathing or coughing.
- Dizziness and disturbances of consciousness (especially in older people).
- Sputum production during coughing.
- Increased body temperature.
- Sweating and shaking.
- Change in skin tone.
- Decreased body temperature (in older people and in patients with weak immunity).
- Nausea, vomiting and diarrhea.
- Hesitant breathing.
Long-term pneumonia can be fatal. Less dangerous complications of pathology include:
- Spread of bacteria in the bloodstream (bacteremia). This is how the infection spreads widely to other organs.
- Respiratory failure. In severe pneumonia or existing lung diseases, respiratory failure may develop, accompanied by a drop in oxygen concentration in the blood. The complication requires hospitalization and artificial maintenance of gas exchange.
- Fluid accumulation around the lungs (pleural effusion). Pneumonia often stimulates the release of exudate into the pleural cavity. This condition is accompanied by breathing problems.
- Lung abscess is the formation of purulent cavities in the organ. This often requires surgery.
If dangerous symptoms appear, including fever, cyanosis and respiratory failure, you should immediately consult a doctor.
How to treat
Newborns and children with severe intoxication are treated in a hospital.
The general treatment regimen is aimed at:
- Prescription of intestinal antiseptics (Uroxolin, Furazolidone).
- Prescription of probiotics (Bifiform, Lactovit).
- The use of enzymes (Festal, Pancreatin).
- Use of bacteriophages (Bacteriophage Klebsiella).
Approximate treatment regimen for systemic infection.
| A drug | Dosage |
| Ampicillin | 45 mg/kg; 7 - 10 days. |
| Neomycin | 10 mg/kg; 7 days. |
| Bacteriophage Klebsiella | From 1 month up to 6 months – 5 ml; From 6 to 1 year – 10ml; 14 days. |
| Bifiform | 1 package / 3 times a day; 5 – 10 days. |
The treatment regimen, dosage and necessary medications are prescribed only by a doctor!
With timely treatment, recovery occurs relatively quickly. To prevent the disease, it is necessary to strengthen the immune system. It is this that is the limiting factor in the development of Klebsiella.
Other diseases
In addition to pneumonia and urological infections, Klebsiella can cause other dangerous pathologies. The most common diseases include:
- Conjunctivitis is an inflammatory lesion of the mucous membrane of the eye, accompanied by the discharge of pus.
- Meningitis is an inflammation of the membranes of the brain and spinal cord due to bacterial invasion. This is a very serious disease that often kills people with weakened immune systems.
- Acute inflammatory bowel diseases.
- Abscesses of the liver and spleen - the formation of purulent cavities in the organs (most often after surgery).
- Inflammation of the pleural cavity and pericardium.
- Inflammation of the mucous membrane of the maxillary sinus.
The listed diseases associated with Klebsiella invasion extremely rarely occur in people with intact function of the body's defense systems.
Klebsiella in a baby
Klebsiella is killed by antibiotics
Due to the incomplete development of the immune system, the child’s body is susceptible to various infections that rarely occur in adults. In particular, a number of infectious diseases in infants are associated with Klebsiella activity.
According to research, this bacterium is a representative of the normal microflora of the body in 57% of children in the first year of life, but in approximately 13% of children the microorganism can cause various diseases.
The most dangerous form of infection in children of the first year of life is pneumonia. Since the child cannot independently complain about his health, parents need to pay attention to the behavior of the baby.
Department of Prematurity and Neonatal Pathology
Urinary tract infections in young children are no less common than viral respiratory diseases. Parents often attribute vomiting, nausea, and pain in the abdomen to colic, malnutrition, or intestinal infections. However, if such symptoms occur, it is recommended to consult a doctor. If it is a urinary tract infection, then its untimely diagnosis and treatment will lead to unpleasant consequences for the baby.
A urinary tract infection occurs when there are bacteria in a child's body that begin to multiply at high speed in the urinary tract.
Most often this pathology is caused by microbes such as:
- Escherichia coli,
- Staphylococcus aureus,
- Pseudomonas aeruginosa,
- klebsiella
Often infections in infants develop against the background of malformations of the urinary tract.
These include:
- vesicoureteral reflux;
- narrowing of the ureters;
- incorrect location of the organs of the urinary system;
- horseshoe kidney and others
Another cause of infection is the presence of a microbial focus in the body. In case of infectious-inflammatory pathology of other organs, bacterial flora can enter the kidneys and urinary tract, causing inflammation there. The bacterium can also enter the child’s body from the mother during breastfeeding.
Urogenital infection in infants manifests itself with the same symptoms as in adults. The problem is that a newborn baby cannot complain.
To identify symptoms of the disease, parents need to closely monitor their child.
Initially, signs such as tearfulness, anxiety, poor sleep and decreased appetite appear.
In children under one year of age, a urinary tract infection may manifest itself as a decrease or increase in urine output compared to the age norm, a change in the color and saturation of urine (a child’s urine may become bright yellow (with an increase in the concentration of urine, which is usually accompanied by a decrease in its quantity), red or brown (impurity blood) When bacteria appear, the urine does not change its color, but becomes cloudy and loses its transparency.
Swelling may appear due to the characteristics of the baby’s body, and an unpleasant odor may appear from the diaper.
The appearance of restlessness and crying when urinating, which indicates the presence of pain and cramping in the baby. Often mothers note that the child strains when urinating. In this case, an intermittent stream of urine is recorded.
A rise in temperature to high numbers, if it does not go away after taking antipyretics and persists for several days, is a reason to suspect an infection.
An infection of the genitourinary system in an infant is detected by conducting a laboratory urine test, urine culture, blood test, and blood test.
With inflammation, blood and urine tests reveal an increase in the number of leukocytes. With bacterial culture, it is possible to identify which bacteria caused the infection and determine the individual sensitivity of the microbe to the antibiotic.
As noted above, the cause of infection in infants may be a congenital anomaly of the genitourinary organs.
If this pathology is suspected, the following examinations should be performed:
— ultrasound examination of the urinary system;
— voiding cystography;
- retrograde radiography of the kidneys;
- CT or MRI of the kidneys.
The basis for treating urinary tract infections is antibiotic therapy. A broad-spectrum antibiotic or a drug based on sensitivity is prescribed. The antibiotic is taken orally or administered intravenously.
It is important that if an infection is detected, the infant should be hospitalized for the entire duration of treatment. In addition to antibiotics, anti-inflammatory drugs and antipyretics are used. Moreover, many medicines are produced in a convenient form of administration, for example, in suppositories.
Herbal uroseptics are often prescribed, which do not have a toxic effect and contribute to the child’s recovery. Under no circumstances should you start treatment on your own or stop taking medications without a doctor’s prescription. This will lead to the disease going into a latent stage and periodically exacerbating, again and again causing unpleasant symptoms. In addition, many medications are contraindicated for children and their uncontrolled use will cause irreparable harm to the child.
Infection in infants with developmental defects will constantly recur, despite high-quality treatment. Therefore, the only way out is to promptly correct the defect. It should be noted that surgery is possible only after the acute inflammatory process has been eliminated.
Prevention of genitourinary tract infections in infants.
In order to exclude illness in a child, the following points should be followed:
- carefully monitor the hygiene of the child’s genitourinary organs.
- avoid hypothermia of the baby;
- Monitor your diet.
Every year, about 1,400 children are treated in the Department of Prematurity and Neonatal Pathology. Of these, 65-70 have urinary tract infections, 28-30 children have various congenital defects of the kidneys and urinary system. All children undergo a complex of examinations and treatment according to developed standards. All children are discharged with improvement and recovery and are subsequently observed by nephrologists and urologists at the regional children's clinic.
A genitourinary tract infection is not such a terrible diagnosis. If there is a complete examination and high-quality, adequately selected therapy, the child will recover without any residual effects.
Additional diagnostics
To clarify the patient’s condition, it is necessary to contact an infectious disease specialist. During the appointment, the doctor will ask the patient about complaints, review medical history to identify risk factors, and conduct a physical examination.
Typically, severe symptoms of infection are detected during a general examination. In addition, if the patient was in the hospital before the onset of the disease, the doctor can immediately guess what pathogen caused the infection.
To clarify clinical and diagnostic data, instrumental and laboratory studies are required. Prescribed diagnostic procedures:
- Blood test for pathogenic microorganisms, liver and kidney functions, plasma biochemistry and the amount of formed elements.
- Urine and stool analysis. In case of infectious diseases of the intestines and urinary system, increased levels of Klebsiella can be detected in the patient’s biological fluids.
- Chest X-ray is a standard scanning method that can detect an abscess or advanced pneumonia.
- Computed tomography and magnetic resonance imaging are highly accurate scanning methods that improve diagnostic data.
- Urethral smear followed by microbiological examination of the material.
Obtaining diagnostic results allows you to prescribe effective treatment.
Treatment of klebsiella
Treatment of diseases caused by Klebsiella depends on the location and severity of the pathological process. Antibiotics are prescribed in severe cases due to sensitivity; in mild cases or only an increase in Klebsiella is detected in tests, they are not used. Be sure to use a variety of drugs that restore intestinal microflora.
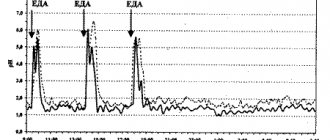
Klebsiella pneumonia As a rule, antimicrobial therapy is recommended to begin even before culture results and determination of drug sensitivity to antibiotics are obtained. In this case, Normoflorin biocomplexes, containing waste products of living lacto- and bifidobacteria with active antiseptic and anti-inflammatory effects, have a therapeutic effect against klebsiellosis, which has been proven by scientific research and many years of practice, both in newborns, pregnant women, lactating women, and adults and the elderly.
Back to list Previous article Next article