Alcoholic liver disease (ALD) is a complex of pathological changes in the liver, the development of which is caused by chronic alcohol consumption in toxic doses.
About 30% of all diffuse lesions of liver tissue are associated with ALD1. Long-term consumption of alcoholic beverages negatively affects all organs and systems, including the liver. The fact is that ethanol in the liver cells is metabolized into acetaldehyde, which has a toxic effect on the cells.9 It is worth noting that women, on average, have lower activity of the enzyme that produces acetaldehyde compared to men, which explains more severe ALD among women and the development of alcohol-induced liver damage in a shorter period of time and at lower doses of alcohol consumed1 (20 g/day for women compared with 30 g/day for men).10
Liver cirrhosis in Russia
In most developed countries, ALD is one of the most common diseases, diagnosed in 10-25% of men and slightly less frequently among women2. WHO (World Health Organization) studies have shown that liver cirrhosis in Russia ranks sixth among all causes of mortality2.
ALD could be called alcoholic fatty liver disease, which is associated with the development of fatty liver in the first stage of the disease with systematic consumption of ethanol in high doses.1 This phenomenon, the accumulation of fat in liver cells, also occurs in non-alcoholic fatty liver disease.
Data
· Alcohol damage occurs due to the toxic effects of alcohol on organ cells.
· The most common damage is fat accumulation. In some cases, cirrhosis and ascites develop.
· Up to a certain point, the damaged liver can recover if you stop drinking alcohol or reduce its amount.
· Cirrhosis is a serious chronic disease that has no cure. But its development can be slowed down by avoiding alcohol consumption and drug therapy.
· Treatment of alcohol-induced liver damage involves first stopping alcohol consumption.
Literature:
- Carbohydrate metabolism, liver and alcohol / E. A. Kosenko, Yu. G. Kaminsky; USSR Academy of Sciences, Scientific. center of biol. research, Institute of Biol. physics. - Pushchino: NCBI, 1988. - 149] p.
- Alcohol and liver / Julus Kalibatas; Ministry of Health of the Lithuanian SSR, Rep. House san. enlightenment. - Vilnius: Mokslas, 1986. - 21 p.
- Alcoholic liver disease: (Classification, diagnosis, treatment): Educational method. allowance / P. I. Podcheko; Ministry of Health of the Russian Federation. Smolen. state honey. acad. - Smolensk, 2003 (State Unitary Enterprise Smol. region. typ. named after V.I. Smirnov). — 30 s.
The text was checked by medical experts: Head of the socio-psychological service of the Alkoklinik MC, psychiatrist-narcologist L.A. Serova.
CAN'T FIND THE ANSWER?
Consult a specialist
Or call: +7 (495) 798-30-80
Call! We work around the clock!
Dynamics of development of liver damage by alcohol
With systematic alcohol consumption, the patient's liver undergoes the following changes.
- At the first stage, inflammation of the liver forms - hepatitis.
- At the second stage, hepatitis turns into fatty hepatosis. At this stage, the penile cells are replaced by fat cells.
- Then the organ does not have time to form new healthy cells and connective tissue (similar to tendons) appears instead. This stage of liver damage is called cirrhosis.
- When the liver ceases to fully perform its functions, the disease ascites occurs. With it, water accumulates in the abdominal space. This condition is called hydrocele.
Hepatitis and alcoholic inflammation give the following symptoms:
· Bitterness in the mouth;
· Vomit;
· Bloating;
· In advanced stages, jaundice appears - yellowing of the skin and sclera.
Cirrhosis is a disease that has no cure. Due to irreversible changes in the cells of the organ, severe poisoning of the body occurs not only with alcohol derivatives, but also with other breakdown products formed in the human body. The brain suffers primarily from this.
Content:
- Effects of alcohol on the liver
- Stages and symptoms
- Common Consequences
- Diagnostics and treatment methods
The hepatobiliary system is the body’s filtering station, purifying the blood and eliminating toxins.
Regular intake of ethanol and round-the-clock work to remove decay products lead to cell degeneration and disruption of gland function. In turn, constant alcohol intoxication of the liver provokes the development of a number of serious pathologies. The article describes the symptoms and causes of poisoning, methods of therapy and restoration of functions used by hepatologists.
Development of the syndrome
Almost everyone who drinks alcohol to excess is at risk for fatty liver disease, but only a small proportion of patients develop liver inflammation, and an even smaller percentage develop cirrhosis.
At the initial stages, a liver damaged by alcohol does not produce pronounced symptoms, but over time it begins to bother the patient more and more.
A clear sign of liver failure is the presence of icteric symptoms. With it, the patient's skin and whites of the eyes turn yellow, and a bitter taste appears in the mouth.
The organ performs the function of purifying the blood. In cases of liver failure, increased amounts of toxins are distributed throughout the body. They have a harmful effect on the brain. Over time, this leads to a person acquiring brain diseases. This is called hepatic encephalopathy or liver brain failure.
Total information
The liver breaks down ethyl alcohol. When it is regularly taken in large doses, it does not cope with detoxification functions - ethanol and its metabolites circulate in the bloodstream, affecting organs and tissues. At the same time, the liver itself also gets affected. Daily doses of ethanol that provoke poisoning have been established:
- for men - 40 g;
- for women - 20 g.
This volume is equivalent to 100 g of regular vodka, 400 g of dry wine or 0.8 liters of beer. Negative consequences can occur both with a one-time use of a dose that is equal to or exceeds the toxic one, and with regular and long-term use of small quantities.
Symptoms of the disease
The damaged organ does not show pronounced symptoms . Problems are most often discovered by chance, during tests, or characteristic symptoms begin to appear in the advanced stages of alcoholism. Violations in the functioning of the organ manifest themselves in the form of:
- chronic fatigue,
- digestive problems,
- bloody vomiting,
- susceptibility to infections;
- mental disorders.
Alcoholic liver inflammation usually appears suddenly and has similar symptoms.
Stages and symptoms
Poisoning of the largest gland is dangerous, as it disrupts the body’s life support. Large doses of alcohol are the hardest to handle. There are three stages of intoxication depending on the amount drunk and the corresponding degree of intoxication.
- An alcohol concentration of 1.5 ppm
is a conditionally safe state of mild intoxication, characterized by elevated mood and noticeably slower speech. - The second is of moderate severity,
the ethanol content is 1.5-3 ppm, the manifestation of neurological lesions of the brain is characterized by impaired coordination, loss of self-control, confusion of consciousness and speech, and unconsciousness. - The third or last degree of severe condition,
from 3.0 to 5.0 ppm or severe intoxication - manifested by nausea, vomiting, possible delirium, loss of consciousness, coma.
An alcohol content of more than 5 ppm is fatal poisoning; urgent medical attention is required, without which death occurs within 2-3 hours.
Symptoms to watch out for:
- pain in the right hypochondrium, kidney area;
- onset of nausea, vomiting, bad breath;
- yellowing of the sclera of the eyes;
- coating on the tongue;
- problems with the gastrointestinal tract - lack of appetite, frequent bloating, diarrhea or constipation;
- constant fatigue, powerlessness;
- increased body temperature, blood pressure;
- pale dry skin, peeling or rashes, itching;
- discoloration of stool, change in urine color.
With severe lesions, the urine becomes dark brown in color as blood cells enter it.
Alcoholic liver toxicosis is a serious poisoning that cannot be cured without the help of a doctor; you must go to a specialized clinic. The sooner the patient receives help, the lower the risk of irreversible consequences.
Establishing diagnosis
The doctor determines the duration of alcohol use or the degree of alcoholism. Based on these data, the patient is prescribed a medical examination. Both general diagnostics and blood tests can determine the extent of liver damage. For this purpose the following is carried out:
- Lab tests.
- Histological studies.
- Ultrasound. To have a visual idea of the disease picture, an ultrasound examination of the liver is performed.
- Biopsy. To do this, the doctor removes a tissue sample using a needle.
- Magnetic resonance and computed tomography.
Diagnostics
One of the key issues in diagnosing ALD is to suspect alcohol as the cause of the pathology. Naturally, patients are not always ready to admit that they abuse alcoholic beverages. Even special questionnaires have been developed that help to unobtrusively clarify the patient’s relationship with the “green serpent”6.
Laboratory results also help confirm the diagnosis8:
increased number of leukocytes in peripheral blood - leukocytosis
decreased levels of hemoglobin and red blood cells - anemia
the increase in AST, ALT is insignificant, the AST/ALT ratio is usually greater2,
Bilirubin levels and blood clotting indicators (prothrombin time) can indicate the severity of the disease.
Of the instrumental studies, ultrasound diagnostics (US) remains the most screening value for diagnosing liver pathology. A comprehensive ultrasound of the abdominal organs, including the liver and gallbladder, helps to exclude obstructive jaundice; steatosis (“fatty liver”) can also be detected: uniform enlargement of the organ, increased echogenicity, diffuse heterogeneity, rounded edges of the organ. Liver elastography is also used, which allows one to assess the presence and degree of fibrotic changes.
Imaging methods such as MRI and CT are also available, however, due to cost, they are used much less frequently. Liver biopsy gives the most complete picture of the form and stage of the disease, however, it is associated with an increased risk of complications, this method has contraindications, must be carried out with a number of precautions, and is therefore used even less frequently.
Causes of alcoholic liver damage
Alcohol affects the metabolism of organ cells. This causes fat (fat cells) to accumulate. In some cases, this causes inflammatory reactions in the liver, leading to the formation of scar or connective tissue.
If exposure (irritation) occurs over a long period of time, the connective tissue contracts and destroys the liver structure. Thus, individual liver cells will not function normally and blood will have difficulty flowing through the organ. This causes the blood to seek other routes, such as through the esophagus. So, as a result of liver disease, varicose veins can appear.
Mechanism of treatment of the syndrome
The goal of treatment is to stop the further development of liver disease and stop necrosis of organ cells. The most important thing is that the patient completely stops drinking alcohol. Diet is also a significant factor in recovery. The patient needs to be provided with good nutrition with vitamin supplements and plenty of fluids.
Diuretics and antihypertensive drugs are also used in therapy. They lower liver blood pressure. If liver function is so poor that waste products such as ammonia are not eliminated naturally, they affect the brain and liver failure (hepatic encephalopathy) develops. Since ammonia is produced in the colon, its elimination can be increased with the help of laxatives. Cirrhosis is treated with antibiotics and protein-rich diets.
In cases of severe jaundice and alcoholic inflammation, they are treated with the adrenal cortical hormone - prednisole.
When to ask for help
If you or your family think there is a problem with alcohol, talk to your GP or consult a drug specialist . If you suspect that you have developed liver disease, you should inform your doctor and undergo the necessary examinations.
You need to contact a specialist in the following cases:
· Systematic consumption of alcohol for 1 year ( Alcoholism ).
· General malaise: drowsiness, chronic fatigue.
· Previous liver diseases.
· Presence of dyspeptic syndrome: morning sickness, indigestion, vomiting, change in stool.
· Tremor of the limbs.
· Sudden change in body weight (dystrophy or obesity).
· Enlarged parotid lymph nodes (Dupuytren's contracture).
· Signs of hypogonadism. In men, they manifest themselves as a slight expression of secondary sexual characteristics: testicular atrophy, gynecomastia, female type of hair growth.
· Pain in the hypochondrium, heaviness in the stomach.
How do liver diseases develop?
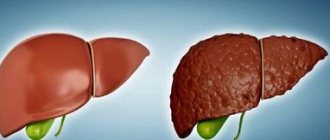
Fatty liver degeneration
If it is fatty liver, then stopping alcohol consumption will be enough to prevent further development of the disease. Over time, the number of fat cells will decrease and the symptoms of the disease will subside. The patient is prescribed a complete abolition of alcohol, special diet food and medications to restore organ cells.
Cirrhosis of the liver
Alcoholic cirrhosis of the liver is a dangerous and incurable disease with high mortality and a significantly reduced quality of life. Cirrhosis begins with fatty liver and, in the absence of timely treatment, leads to irreversible consequences and further death.
Cirrhosis develops into a chronic disease that progresses to ascites if alcohol consumption continues. This leads to a significant increase in mortality and a difficult life with the following symptoms.
· Chronic fatigue and constant lack of strength.
· Tendency to varicose veins in the esophagus. This phenomenon develops into bloody vomiting.
· Tendency to infections (decreased immunity).
· Mental disorders such as difficulty concentrating, bizarre behavior patterns, sleep disturbances, and depression often occur.
These complications significantly reduce life expectancy. In particularly advanced cases, the problem is solved by liver transplantation.
Alcohol liver inflammation
This disease occurs against the background of intensive alcohol for 1 or more years. Alcohol inflammation without cessation of alcohol consumption and lack of treatment leads the patient to death.
Pathogenesis
The disease can develop over a long period of time: months and years. The pathological influence of viruses on liver cells, toxic substances (drugs, alcohol), impaired blood supply to the organ, immune mechanisms, and the influence of inflammatory mediators lead to massive death of hepatocytes and replacement with connective tissue. This process disrupts all vital functions of the liver.
- 1. Fatty degeneration. Initial changes in the structure and function of hepatocytes, which can completely disappear within a few weeks if the intake of alcohol in the body is stopped.
- 2. Steatohepatitis. An inflammatory process develops. The structure and size of hepatocytes change; in severe cases, the cells die, which affects the general condition of the liver. At this stage, disturbances in the functioning of the organ already occur, and specialized treatment is also required.
- 3. Cirrhosis. The formation of irreversible fibrous changes in the organ, disruption of the general structure: the appearance of tuberosity, reduction in size. If left untreated, the condition progresses and liver functionality decreases. Dangerous complications develop not only in the organ itself, but also in the structures dependent on it.
The sooner you consult a doctor and, most importantly, stop drinking alcohol, the higher your chances of getting rid of the problem.
Morbidity statistics
- Cellular obesity is a fairly common problem among the population of post-Soviet countries. The disease affects up to 10% of all Russian residents. This is primarily associated with excessive alcohol consumption, excess weight and high rates of diabetes.
- Alcoholic cirrhosis occurs with a probability of about 1000 new cases per year. For example, in Denmark about 12,000 people have this disease; in the Russian Federation this number is not precisely determined. It is known that incidence rates are several times higher than in European countries. The lack of accurate data on incidence is explained by the fact that many cases are diagnosed only after an autopsy of the deceased patient.
- Alcohol-related inflammation is a rarer disease and has fewer new cases per year than cirrhosis.